Norfolk Neurology Network Action Plan
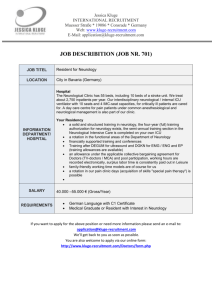
advertisement
Norfolk Neurology Network Action Plan 2013 Norfolk Neurology Network Action Plan This action plan is based on the priorities identified by the Quality Neurology audit undertaken across Norfolk in Autumn 2012. Top priorities: Education and professional training Non-specialist and care home staff need better training, with mandatory competency standards. Action: Discuss with Social Services. Information Information needs to be streamlined so that clearer materials are available to both professionals and patients, at diagnosis and to support selfmanagement. Action: Review Heron website. Information given by consultants at diagnosis- R Rendell to speak to NNUH consultants; J Fuller is in contact with James Paget consultants; KH and / or Lindsay Gowan to talk to QEH consultants. Quick wins: Produce a neurology services information booklet for patients that signposts to specific services; and for professionals listing colleagues’ roles and locations. Action: Review Heron website. Implement integrated care pathways (ICPs). Action: Postholder to facilitate implementation of Parkinson’s pathway to be appointed; E Frost to adapt ICP for MS. Training for non-neurology staff (eg GPs, general nurses, care home staff) and mandatory competency standards. This might include e-learning. Action: Voluntary sector to promote their training and e-learning resources- how? Brief reference guides for non-specialists (eg simple prompt cards for nonspecialists listing what to ask patients about their specific conditions). Action: collate resources already available from voluntary sector. Recommendations for action in the 10 areas considered in the audit: 1. A person-centred service: Integrated health and social care assessments Expand System One into all health and social care settings and use it for single assessment Specialist nurses sharing responsibilities more strategically to improve capacity issues 2. Early recognition Norfolk Neurology Network Action Plan 2013 Condition-specific information packs for GPs and consultants to give to patients Prompts for non-specialists about what to ask neurology patients A journey map or disease pathway covering both health and social care roles 3. Emergency and acute management Training for non-neurological staff about what to focus on for admissions of neurology patients A flagging system when a neurology patient is admitted to a non-neurology ward Copy good practice to get ‘medication on time’ initiatives into other hospitals 4. Early and specialist rehabilitation A secondary to primary care discharge pathway and policy to support sustainable rehabilitation A common progress assessment tool for all professionals Explicit information for professionals and patients on equipment, with eligibility criteria and clear guidelines on who is responsible for providing it 5. Community rehabilitation and support Better access to self-care programmes and information A key worker system to improve the co-ordination of care 6. Vocational rehabilitation Better information systems for both patients and professionals that support people to remain employed or to return to work. Action: Arrange training courses for AHPs 7. Providing equipment and accommodation A single point of contact (Action: done?) Information about what equipment is available (Action: Done?) Criteria for obtaining equipment and a self-assessment tool for eligibility (Action: Done?) 8. Providing personal care and support Stronger links with social services to guarantee services are integrated Clear referral processes to community care after discharge from acute settings Clear information on who provides care to people living in border areas Give service users more information about personal budgets Establish e-learning for nursing and residential homes to use as part of the induction package for new staff Norfolk Neurology Network Action Plan 2013 9. Palliative care Follow the Gold Standards Framework for everybody with a neurological condition Ensure advance care planning can be discussed with all neurology patients Provide ongoing training, particularly to care homes, on managing a person’s end-of-life care needs for living with a neurological condition 10. Supporting family and carers Urgent priority: produce explicit information about the carer support services available and distribute to both professionals and carers Map and highlight all respite services in the information booklet mentioned in QR1 and QR2 Inform carers of their right to a carer’s assessment 11. Care for people in hospital or other health and social care settings An alert system that prompts hospital and care home staff to seek advice about a person’s neurological condition when they are admitted for a nonneurological reason. This should include alerting community staff or the person’s keyworker Copy good practice to get ‘medication on time’ initiatives into other hospitals Accessible education for non-neurology staff on how to manage specific neurological conditions