Minimum Standards - FSN_v1
advertisement
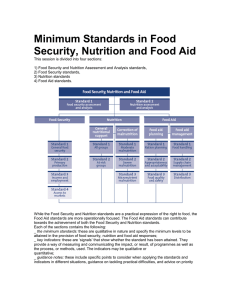
Minimum Standards1- Food Security and Nutrition Priorities for populations should focus on ensuring an adequate supply of food and the maintenance of adequate nutritional status. Undernutrition is a serious public health problem, and among the lead causes of death. It is imperative to ensure that the population has the necessary access to adequate nutrition, through physical, social and economic access to sufficient safe and nutritious food to meet their dietary requirements for an active and healthy life. FSN standard 1: Food Security All people have safe and equitable access to a sufficient quantity of food including local sources and imported foods. The ability of local markets to supply food is a major determinant of availability. The affected population requires the availability of food, the capacity to access this food, through production, procurement availability of loans or gifts and the use of cash or vouchers to increase the purchasing capacity of the population. The successful utilisation of the food is also determined by methods of preparation, storage and distribution of access within the household, as well as by the health of the individuals. Key indicators Assessment of availability of food both under production and in local markets VAM, FEWS Net. KI and FGD surveys etc. Economic and social ability of population to access food Nutritional status of population – to be determined by surveys Reduction in use of Coping Strategies by population Other indicators Contextual information from primary & secondary sources; existing data, early warning information, health centre reporting, community groups and government reporting. Nutrition Surveys, including trends Price surveys in markets including trends Overall Economic indicators and trends, including observation of population movements Monitoring of household coping strategies and take-up of such strategies in populations Anthropometric surveys and reporting of GAM and SAM Population data Surveys of micronutrition deficiency Key actions 1. Act to ensure population has access to immediate adequate food needs. 2. Promote Food Security for longer term needs. 3. Ensure that interventions do not displace or unbalance the existing market, and monitor effects of intervention upon existing social and economic situation. 1 The proposed outline is inspired by the Minimum Standards in Humanitarian Response (SPHERE) http://www.sphereproject.org/ 1 4. Monitor access to adequate food of identified vulnerable or specific identified sections of the population. Support the ability of the population to advocate for themselves, and to participate where possible in the management of the strategy 5. Support appropriate coping strategies and seek to minimise or find alternatives to coping strategies which will create risks or increase vulnerabilities of population. 6. Develop an exit strategy FSN standard 2: Infant and Young Child Feeding Optimal feeding practice maximises survival and reduces morbidity in children under 24 months of age. Exclusive breastfeeding for 6 months, continued breastfeeding to at least 24 months and introduction of adequate, safe and complementary foods at 6 months. Support to reduce the risks of artificial feeding, enable appropriate feeding for vulnerable individuals such as Low Birth Weight, those at risk of HIV & the Severely Malnourished. Support to pregnant and lactating women and support to other caregivers such as grandparents, single fathers, siblings etc. Key indicators % of infants under 6 months being exclusively breastfed. % of infants under 24 months still breastfed together with complementary feeding % of infant morbidity / mortality due to diarrhoea and similar illnesses attributable to contaminated foods Other indicators Key actions 1. Target mothers of all newborn babies with support for early initiation of exclusive breastfeeding. Non breastfed infants should be provided with support. Breastfeeding support should be intergrated within key services such as health. 2. Pregnant & breastfeeding women should receive micronutrient supplements, plus iron and folic acid supplements, and vitamin A within six to eight weeks of delivery. See international recommendations on dosages and timing. 3. Support exclusive breastfeeding for infants up to 6 months, and complementary feeding with safe food preparation availability between 6 months and 24 months. 4. Identify and avoid use of formula BMS, bottles, teats and similar aids to artificial feeding. If such articles are donated they should be placed under control of Unicef as the designated organisation for control of all artificial substitutes. FSN standard 3: Management of Acute Malnutrition Acute malnutrition response should address the underlying causes of malnutrition. Supplementary feeding should be based upon targeted or blanket approach. Choice should depend upon levels of acute malnutrition and caseload. Where severe acute malnutrition is addressed through therapeutic 2 care this should be community based where possible. Community mobilisation should be part of the response (communication, identification of cases, referral, follow-up) Key indicators Coverage of affected population by the programme. (how many receive treatment as against how many need treatment) Performance indicators – deaths, recovered, defaulted and non-recovered as a percentage of admissions. Fewer than 10% deaths in population discharging from programme, and fewer than 15% defaulted, with greater than 75% recovered. More than 90% of target population able to access programme centres, and coverage of greater than 70% in urban environment. Key Actions 1. Establish a clear strategy for the assessment and response intervention. 2. Link the management of moderate acute malnutrition and severe acute malnutrition to the existing health services where possible. Build programmes on existing health system where possible. 3. Discharged individuals should be free from medical complications – linkage to existing health programming is necessary to address this 4. Micronutrient deficiency should be addressed as well as acute malnutrition. 5. Underlying causes of malnutrition should be addressed. FSN standard 4: Livelihoods Livelihoods are the methods by which people acquire income and food. The resources available to them including capital (savings or credit), physical (homes or items which can be sold or used to manufacture income such as a mill or a shop), natural (land / water eg. crops or fish), human (labour) social (community support or remittances from relatives) and political (representation or influence). The loss of any of these forms of livelihood may reduce access to food. Livelihoods can be separated into Primary Production, Income Generation and Access to Markets. The purpose of a Livelihoods Intervention is to support populations who are unable to meet their basic needs without extra inputs. The Livelihood interventions should always have an exit strategy in order to avoid creating a situation of dependence. Key indicators Households have access to the necessary inputs to protect and restart primary production (note, in an urban environment this is less relevant since only small-scale production of food is likely (fishing in rivers, keyhole gardens etc.) Households have access to sufficient purchasing power (by means of income, cash / voucher distribution or credit to finance income generation activities) to provide for the basic needs 3 of both food and other essentials (if other essentials such as school are not met food may be reduced to provide cash surplus for these costs) All targeted populations have safe and full access to markets (including special vulnerable groups eg. disabled, single women, by generating incomes through their activities and are able to meet their basic needs. Key actions 1. Market Study to assess actual costs of basic food needs and analysis of household expenditure in target groups. 2. How did groups in population acquire food, and has this changed? 3. Identification of special groups and their requirements in order to access adequate food and other essentials. Eg. some groups may not be able to participate in income-generating activities and will need unconditional support as a safety net. 4. Survey of impact of interventions on existing markets and economies. Income generating activities should be appropriate to the situation. 5. Responses providing employment are available to men and women, and do not negatively impact on the local labour market or normal livelihood activities 6. Survey of fluctuations in existing markets 7. Survey of Coping Strategies and the consequences of these? (finance, health, environment, dignity?) 8. How will intervention exit strategy be implemented? 4 1. Appendix 1 Food Security and Nutrition Initial Needs Assessment Checklist This list of questions is primarily for use to assess needs, identify resources and describe local conditions. It does not include questions to determine external resources needed in addition to those immediately and locally available. 1 General _ How many people live in the location? Disaggregate the data as far as possible by sex, age, disability etc. Map their houses/locations _ What are the current or threatened food security situation? What are the extent and expected evolution of problems? _ Who are the key people to consult or contact? _ Who are the vulnerable people in the population and why? _ Is there equal access for all to existing facilities? _ What special security risks exist for women and girls? _ What food production and procurement process does the population currently employ? _What are the coping strategies employed by the population? 2 Food supply _ What are the current food supply routes, and how are they used by the population? Eg. Does population grow own food, catch wild food, sell labour to purchase food etc? _ How much food is available per person per day? _What is the access to markets? _What are the key constraints preventing people from accessing sufficient food supply? _ Does the food supply available meet nutritional requirements? 3 Nutrition _Suggest fill in by Nutrition programme specialist _Is there a change in the nutritional status of the population? _Are there disease outbreaks or other health related reasons for malnutrition? _What is the measles vaccination coverage of the population? Is there a high prevelance of HIV or TB? _Is there a high incidence of malaria? _Have people been exposed to harsh environment (eg in water or wet clothes) for long periods of time? _What formal sturctures such as Ministry of Health, community structures, religious institutions or similar can be used to channel interventions? _What methods are currently in use to identify nutritional status? _What particular vulnerable groups need to be targeted by an intervention? _Is food hygiene compromised as a result of the population’s situation? 4 Infant and Young Child Feeding _Suggest fill in by Nutrition programme specialist 5 Livelihood Programming _Identify the assets, social resources, activities and coping strategies _Assess the existing capacity of markets and labour markets to anticipate whether intervention will stress existing structures. _Is food, vouchers or cash programming most appropriate? _Is conditional or unconditional programming more appropriate? _How can minority or vulnerable sectors of population be targeted? 5 6