P161 IMPROVEMENT IN NUTRITIONAL STATUS OF A
advertisement

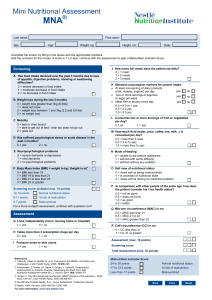
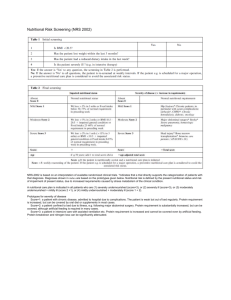
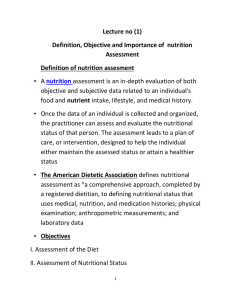
P161 IMPROVEMENT IN NUTRITIONAL STATUS OF A HAEMODIALYSIS PATIENT WITH SEVERE ANXIETY ACHIEVED BY EFFECTIVE MULTIDISCIPLINARY TEAM WORKING – A CASE REPORT King, M. Department of Nutrition and Dietetics, Salford Royal NHS Foundation Trust Malnutrition is a common problem in end stage renal disease. The prevalence of malnutrition in haemodialysis patients is estimated between 30-75% and is associated with poor clinical outcomes and mortality. The main causes of malnutrition in haemodialysis patients include inadequate dialysis dose, inflammation, dietary restrictions, nutrients lost via the dialysate and the catabolic properties of dialysis. In this case report, severe anxiety leading to anticipatory nausea also contributed to malnutrition. A 30 year old women was referred to the dietetic department in September 2011 after “crash landing” with an eGFR 6. She was diagnosed with Haemolytic Uraemic Syndrome and was commenced on haemodialysis. Nutritional assessment included monitoring of blood biochemistry, anthropometry (base weight, Body Mass Index, percentage weight loss, hand grip strength, mid arm circumference, tricep skinfold thicknesses), fluid balance and energy and protein intake. There was a decline in daily dietary intake in the first three months after starting haemodialysis. Food fortification and oral nutritional supplements were commenced and not tolerated and the patient did not always consent to review. Due to further decline in nutritional status, the patient was admitted to hospital in October 2012 for enteral tube feeding. Initially, dietary intake improved but throughout admission it was variable depending upon anxiety levels. In addition to oral diet, nasogastric feeding was commenced but only small flow rates were tolerated and only 22% of energy and 26% of protein requirement could be provided by NG feeding. Several NG tubes were dislodged and re-insertion of NG tubes were delayed due to anxiety attacks. It was not deemed appropriate for insertion of a percutaneous endoscopic gastrostomy by the Trust’s Nutrition Support Team. Date Base BMI % weight loss MAC HGS TSF weight (kg/m2) (cm) (kg) (mm) (kg) Sept 2011 72 24.0 Baseline February 2012 60 20.0 16.7 October 2012 50.1 16.7 30.4 21 7.9 11.6 November 2012 44 14.7 38.9 19 11.7 9.7 January 2013 46 15.4 36.1 19.5 9.9 April 2013 53 17.7 26.4 19.5 10.6 4.8 December 2013 63 21.0 12.5 In November 2012, a multidisciplinary team meeting was held, with Consultant Nephrologist, Advanced Nurse Practitioner, Consultant Psychologist, ward manager, Dietitian, patient and husband. A frank discussion of the current situation was discussed and a nutritional care plan was agreed ensuring good communication between all team members. Subsequently, the patient began to focus upon increasing dietary intake and tolerated NG feeding, allowing for the patient to be discharged home with overnight NG feeding for a six month period leading to an improvement to nutritional status. An improvement in nutritional status was achieved in a patient with severe anxiety through use of effective team working and communication.