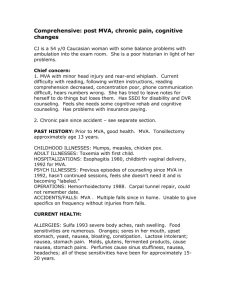
Jordan T Krute
advertisement
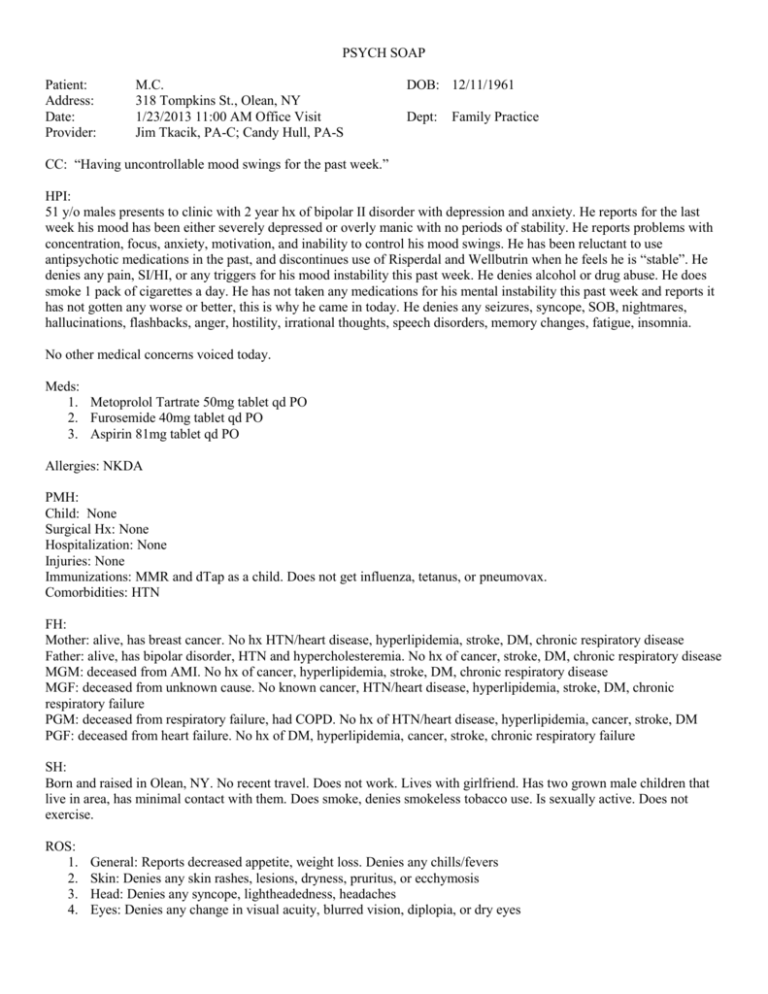
PSYCH SOAP Patient: Address: Date: Provider: M.C. 318 Tompkins St., Olean, NY 1/23/2013 11:00 AM Office Visit Jim Tkacik, PA-C; Candy Hull, PA-S DOB: 12/11/1961 Dept: Family Practice CC: “Having uncontrollable mood swings for the past week.” HPI: 51 y/o males presents to clinic with 2 year hx of bipolar II disorder with depression and anxiety. He reports for the last week his mood has been either severely depressed or overly manic with no periods of stability. He reports problems with concentration, focus, anxiety, motivation, and inability to control his mood swings. He has been reluctant to use antipsychotic medications in the past, and discontinues use of Risperdal and Wellbutrin when he feels he is “stable”. He denies any pain, SI/HI, or any triggers for his mood instability this past week. He denies alcohol or drug abuse. He does smoke 1 pack of cigarettes a day. He has not taken any medications for his mental instability this past week and reports it has not gotten any worse or better, this is why he came in today. He denies any seizures, syncope, SOB, nightmares, hallucinations, flashbacks, anger, hostility, irrational thoughts, speech disorders, memory changes, fatigue, insomnia. No other medical concerns voiced today. Meds: 1. Metoprolol Tartrate 50mg tablet qd PO 2. Furosemide 40mg tablet qd PO 3. Aspirin 81mg tablet qd PO Allergies: NKDA PMH: Child: None Surgical Hx: None Hospitalization: None Injuries: None Immunizations: MMR and dTap as a child. Does not get influenza, tetanus, or pneumovax. Comorbidities: HTN FH: Mother: alive, has breast cancer. No hx HTN/heart disease, hyperlipidemia, stroke, DM, chronic respiratory disease Father: alive, has bipolar disorder, HTN and hypercholesteremia. No hx of cancer, stroke, DM, chronic respiratory disease MGM: deceased from AMI. No hx of cancer, hyperlipidemia, stroke, DM, chronic respiratory disease MGF: deceased from unknown cause. No known cancer, HTN/heart disease, hyperlipidemia, stroke, DM, chronic respiratory failure PGM: deceased from respiratory failure, had COPD. No hx of HTN/heart disease, hyperlipidemia, cancer, stroke, DM PGF: deceased from heart failure. No hx of DM, hyperlipidemia, cancer, stroke, chronic respiratory failure SH: Born and raised in Olean, NY. No recent travel. Does not work. Lives with girlfriend. Has two grown male children that live in area, has minimal contact with them. Does smoke, denies smokeless tobacco use. Is sexually active. Does not exercise. ROS: 1. 2. 3. 4. General: Reports decreased appetite, weight loss. Denies any chills/fevers Skin: Denies any skin rashes, lesions, dryness, pruritus, or ecchymosis Head: Denies any syncope, lightheadedness, headaches Eyes: Denies any change in visual acuity, blurred vision, diplopia, or dry eyes 5. Ears, Nose, Sinuses: Denies any ear pain, change in hearing, tinnitus, epistaxis, runny nose, sinus tenderness, swollen glands 6. Throat: Denies any facial pain, mouth ulcerations/sores, dental pain or sensitivity, sore throat, difficulty swallowing 7. CV: Denies any chest pain, DOE, palpitations, lightheadedness, dizziness 8. Respiratory: Denies any SOB, cough, hemoptysis, pleuritic chest pain 9. GI: Denies abdominal pain, nausea, vomiting, heartburn, constipation/diarrhea, rectal pain, bleeding, melena 10. Vascular: Denies any ulcerations or color changes noted 11. Musculoskeletal: Denies any back pain, muscle aches, joint stiffness, cramping, edema 12. Hematologic: Denies any bleeding, bruising 13. Endocrine: Denies any polydipsia, polyuria, polyphagia, heat/cold intolerance, diaphoresis 14. Psychiatric: See HPI PE: BP 128/74, HR 78, T 98.6 °F, RR 18, Ht 72”, Wt 265#, O2 98% @ room air, Pain 0/10 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. General Appearance: WDWN WM in NAD, appearing stated age. Depressed affect Skin: No rashes or lesions noted. Bronze color, warm, moist with good turgor. Capillary refill <2 seconds b/l. Skull/scalp: Equal b/l hair distribution without nits. No boney abnormalities or tenderness palpable. HEENT: Full visual fields b/l in all 4 quadrants, bulbar and sclera clear, PERRLA, EOMI without nystagmus/lid lag/strabismus or discharge. Retina deep orange, disc yellow, no exudates or hemorrhages visualized b/l. Hearing equal b/l with scratch test, TM’s visualized b/l, pars tensa pearly gray, external canal fleshy pink without discharge or cerumen, erythema, fluid levels, scar tissue, perforations, or drainage. Nasal musosa pink and turbinates visualized without drainage, edema, or obstruction. Moist mucosa/gums without oral or pharyngeal masses, ulceration or thrush. No sinus tenderness. Neck: Trachea midline, supple, smooth carotid upstrokes without JVD, no palpable thyromegaly or LAD. Full ROM without crepitus or tenderness. CV: RRR, S1 > S2 heard without any appreciable murmurs, rubs, gallops. PMI visible at L fifth intercostal space at anterior axillary line. Palpation without tenderness, lifts, heaves or thrills. PMI palpable at L 5th ICS at AAL. Respiratory: Symmetrical A/P-Lateral ratio 1:2. No rashes, deformities, intercostal retractions, or accessory muscle use noted. Palpation without tenderness or masses noted. Respiratory excursion full. Tactile fremitus symmetrical throughout all areas. Percussion resonant throughout thorax. CTA b/l. GI: abdomen is protuberant, without deformity, no abdominal/femoral bruits noted. No AAA appreciated. Active bowel sounds present all 4 quadrants, no appreciable hepatosplenomegaly, no palpable masses. Periumbilical and LUQ tympanic upon percussion. Liver percussible at 6cm right MCL. Spleen, bladder not percussible. Abdomen soft, nontender. Light & deep palpation reveal no masses or tenderness. No rebound tenderness or guarding. Musculoskeletal: No pain on palpation over bony prominence, no edema, no evidence of gout, no joint or bony deformity, no crepitus. Full passive and active ROM. Extremities: no clubbing or cyanosis Neurologic: A&O x3. Speech intact without aphasia. Short and long term memory without deficiencies. Without fasciculations or other involuntary movements. Strength equal b/l, sensation equal b/l in extremities and torso. Gait without ataxia, negative pronator drift, negative Romberg. MSE: Appearance – pt. is well groomed, showered, and appropriately dressed Behavior – appropriate with no abnormal movements. Good eye contact Attitude - cooperative Speech – good communication skills without vocabulary problems, stutter, or loudness Psychomotor – no tremor, ataxia, or retardation Cognition - appears intact, understanding conversation and psychiatric situation clearly Insight – good understanding of current condition and change in mood Judgment - sought help recognizing mood instability and increased depression Impulse control – not impulsive at this time, maintaining control Sensorium – spelled WORLD backwards appropriately ASSESSMENT/PLAN: 1. Axis I: Bipolar I disorder a. Start Risperdal 0.5mg tablet bid PO b. Discussed SE: orthostatic hypotension, tachycardia, sedation, dystonia, sexual dysfunction, constipation c. Discussed medication compliance 2. Axis I: Other personality disorder a. Start Diazepam 5mg tablet bid PO b. Discussed SE: sedation, hypotension, bradycardia, rash c. Discussed medication compliance 3. Axis I: Major depressive disorder a. Start Wellbutrin XL tablet 150mg PO b. Discussed SE: seizure, agitation, insomnia, headache, tachycardia c. Discussed medication compliance 4. Referral to psychology a. Discussed ongoing counseling b. Discussed family and social support system 5. Preventative health office visit a. Referral for labwork: CBC, CMP, TSH, UA, lipid profile b. Discussed healthy diet and regular exercise c. Discussed mental health illness d. Provided educational pamphlets on bipolar I disorder e. Provided educational pamphlets on coping mechanisms and stress reduction 6. RTC 1 month or sooner if needed 7. Go to ED if symptoms worsen or any adverse drug reaction to medications 8. Patient verbalized understanding Candy Hull Candy Hull, PA-S 1/23/13, 11:35 a.m.