AKI patient information leafletWHH
advertisement

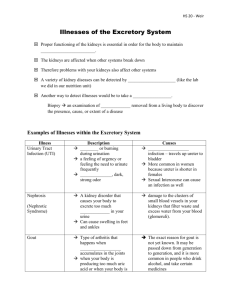
Acute Kidney Injury (AKI) Patient / Relatives copy Information for Patients & Family Patient Name: What do Kidneys do and where are they? ……………………………………………. Most people have two kidneys. They lie to either side of the back bone just below the ribs. Cause of Acute Kidney Injury Kidney ……………………………………………. You have been given this leaflet by your doctor because you have acute kidney injury. This leaflet explains the condition, what your kidneys do and what we will be doing to help you’ What is Acute Kidney Injury (AKI)? Acute Kidney Injury (AKI) –previously known as acute renal failure – is a term used to describe a range of conditions where there is a rapid reduction in kidney function. This means there is a failure to maintain fluid, salt and acidic balance. The main cause of AKI is a lack of blood flow to the kidneys. This can be caused by many things such as; dehydration, infection or blood loss. The body preserves the blood supply to the brain and heart – this redirects it away from the kidney which can cause it to fail. It can also occur due to toxins, when there is a problem inside the kidney or a blockage in the tubes carrying the urine away from the kidneys. About a quarter of the blood from the heart passes through the kidneys, which filter and clean our entire blood volume about 35 times per day Kidneys help balance the fluid and salts in your body. They remove waste products and toxins by producing urine. They are also important for maintaining healthy bones and red blood cells. Why is AKI dangerous? Your heart can be affected due to the changes in salts in the blood The build-up of waste products can cause damage to other organs You are also unable to get rid of the toxic remains of drugs you may be taking Patient information sheet for AKI (acute kidney injury) December 2014 for review December 2017 based on Aintree hospital’s leaflet reproduced for WHH with permission. Dr Chattington Who is at risk? Approximately 15% of adults that are admitted to hospital develop AKI. The elderly are more at risk, along with patients with chronic kidney disease (CKD), diabetes, heart failure or liver disease. What are the signs of AKI? You do not usually feel unwell until kidney function has deteriorated significantly sometimes to less than 10% The first sign of the kidneys not working properly is a person stops producing as much urine. HELP US TO HELP YOU 1. YOU SHOULD HAVE YOUR OBSERVATIONS 2. 3. 4. 5. What treatment will I have? Later symptoms include headaches, feeling tired, nausea and vomiting. A blood test can identify acute kidney injury before any symptoms. What tests will I need? Kidney function can be measured in a number of ways. The use of a urinary catheter may be used to measure urine output. Blood tests can measure the levels of waste products (creatinine and urea) that build up in the blood. Blood tests can also measure the levels of salts and acid in the blood to see if they are balanced. Urine tests for protein and blood can indicate leakage due to kidney damage. You may be sent for an ECG, X-rays or ultrasound scans of your kidneys. Some types of AKI may need a kidney biopsy to determine the cause. A tiny piece of your kidney is taken via a needle under local anaesthetic. TAKEN REGULARLY INCLUDING DAILY WEIGHT YOU SHOULD HAVE DAILY BLOOD TESTS FOR SALT AND KIDNEY FUNCTION LEVELS FEEL FREE TO ASK THE DOCTOR HOW ANY DRUGS MAY AFFECT YOU KIDNEY AND AVOID ALL ‘NSAIDS’ LIKE IBUPROFEN KEEP TRACK OF HOW MUCH YOU DRINK AND WHEN YOU PASS URINE YOU SHOULD BE BOOKED FOR AN ULTRASOUND SCAN TO LOOK AT THE KIDNEYS IF THEY CONTINUE TO BE IMPAIRED The cause of the AKI will need to be identified and treated. You may receive intravenous fluids to rehydrate your body. Some patients require tablets to reduce the build-up of fluid and acid. A urinary catheter may be used to relieve a urinary tract blockage. You may require antibiotics to treat an infection. You may very occasionally be put on dialysis if your kidneys do not respond. This involves passing the blood through a machine for a number of hours. The machine cleans the blood while your kidneys recover. Diet and fluids in acute kidney injury Why is diet important? When your kidneys are not working well, a build up of waste products and fluid can occur in your body. Eating the right foods can help prevent a build up of waste products, help control your blood pressure and keep salts in balance. Patient information sheet for AKI (acute kidney injury) December 2014 for review December 2017 based on Aintree hospital’s leaflet reproduced for WHH with permission. Dr Chattington Fluid Some patients need more fluid, others require fluid restriction. Your doctor should advise you how much fluid you should drink a day. As well as tea, water and other drinks, you will also need to count certain foods as part of your fluid allowance for example, jelly, ice cream, milk on cereal, porridge, milk puddings, soup, gravy and sauces. What can I do to stop this happening again? You could prevent AKI by minimising your risk factors Salt Too much salt in your diet can increase your blood pressure. Salt can also make you thirsty. If you are on a fluid restriction this can make it harder to keep to your fluid allowance. Try to use less salt in your diet and limit processed foods (high in salt). Do not use salt substitutes e.g. LoSalt or Selora Potassium When your kidneys do not work properly they struggle to maintain the potassium balance. Some blood pressure tablets can further increase potassium level in your blood. High levels of potassium can be dangerous to your heart. If your blood tests show an increased potassium level your doctor will refer you to a dietician for advice on a low potassium diet. You may also require medications to reduce the potassium in your body. How long do I need to be at the hospital for? You will usually need to remain in hospital until your kidney function recovers to a safe level. The cause of AKI will also need to be investigated so that it does not happen again Drink plenty fluids when unwell, especially if you are suffering from diarrhoea and vomiting. If you are not able to do this then urgently seek medical attention. If you have an infection, you should see your doctor if you are very unwell, dizzy and passing less urine. High blood pressure control – if you suffer from high blood pressure make sure you take your medication and measure your blood pressure regularly. Don’t drink as much alcohol. Too much alcohol is associated with high blood pressure which can affect your kidneys. Diabetic? Good blood sugar control can help protect your kidneys. Take all your medication. Taking your prescribed medication regularly as instructed by your clinician. This will help ensure your kidney function does not deteriorate. Avoid Non-steroidal anti-inflammatory drugs (NSAIDs) – ibuprofen, naproxen, voltarol or other types of pain killer such as celecoxib or enterocoxib –these drugs can damage your kidney – try to avoid them and use paracetamol for pain relief instead. Ask your pharmacist if in doubt If you can’t pass urine see your doctor immediately. What happens now? Whilst you are an inpatient your doctors will see you regularly and keep you informed of your progress. If you require dialysis more information will be given to you by the kidney specialists. If your kidney function does not recover fully you will probably be followed up in the kidney clinic. Patient information sheet for AKI (acute kidney injury) December 2014 for review December 2017 based on Aintree hospital’s leaflet reproduced for WHH with permission. Dr Chattington Warrington and Halton Hospitals NHS Foundation Trust is not responsible for the content of any material referenced in this leaflet that has not been produced and approved by the Trust. If you require a special edition of this leaflet This leaflet is available in large print, Braille, on audio tape or disk and in other languages on request. Please contact Customer Services on: Telephone 01925 275249 Patient information sheet for AKI (acute kidney injury) December 2014 for review December 2017 based on Aintree hospital’s leaflet reproduced for WHH with permission. Dr Chattington