The Urinary System
advertisement

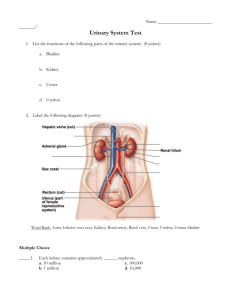
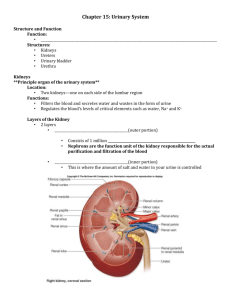
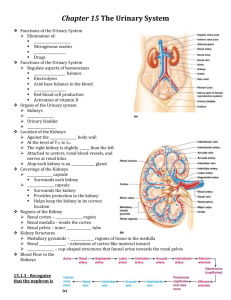
24 PART 1 The Urinary System The Urinary System • Important functions of the kidneys • Maintain the chemical consistency of blood • Filter many liters of fluid from blood • Send toxins, metabolic wastes, and excess water out of the body • Main waste products are three nitrogenous compounds • Urea • Uric acid • Creatinine Organs of the Urinary System • Kidneys • Ureters • Urinary bladder • Urethra Location and External Anatomy of Kidneys • Kidneys are red-brown in color • Located retroperitoneally • Behind the peritoneum • Lateral to T12–L3 vertebrae • Average kidney is 12 cm tall, 6 cm wide, 3 cm thick • Hilum • Is the concave surface • Vessels and nerves enter and exit Location and External Anatomy of Kidneys • Fibrous capsule • Capsule of dense connective tissue surrounds the kidney • Inhibits spread of infections • Perirenal fat capsule • External to renal capsule • Renal fascia • External to perirenal fat capsule • Contains fat Internal Gross Anatomy of the Kidneys • Frontal section through the kidney • Renal cortex • Superficial region, granular appearance • Renal medulla consists of • Cone-shaped renal pyramids • Renal pelvis • • Major calices Minor calices Internal Gross Anatomy of the Kidneys • Gross vasculature • Renal arteries branch into segmental arteries • Segmental arteries branch into interlobar arteries • Arcuate arteries branch from interlobar arteries Internal Gross Anatomy of the Kidneys • Nerve supply—renal plexus • A network of autonomic fibers • An offshoot of the celiac plexus • Supplied by sympathetic fibers from • Lowest thoracic splanchnic nerve • First lumbar splanchnic nerve Microscopic Anatomy of the Kidneys • Nephron is the functional unit of the kidney • Over 1 million nephrons in each kidney Mechanisms of Urine Production • Filtration • Filtrate of blood leaves kidney capillaries • Resorption • Most nutrients, water, and essential ions reclaimed • Secretion • Active process of removing undesirable molecules Nephron Structure • Nephron is composed of • Renal tubule • Renal corpuscle 24 PART 2 The Urinary System Nephron Structure • Renal corpuscle—first part of nephron • Glomerulus and glomerular capsule • Glomerulus—tuft of capillaries • Capillaries of glomerulus are fenestrated • Glomerular (Bowman’s) capsule • Parietal layer—simple squamous epithelium • Visceral layer—consists of podocytes Filtration Membrane • The filtration membrane • Filter that lies between blood in the glomerulus and capsular space • Consists of three layers • Fenestrated endothelium of the capillary • Filtration slits between foot processes of podocytes • Basement membrane Filtration Membrane • Basement membrane and slit diaphragm • Hold back most proteins • Allow passage of • Water • Ions • Glucose • Amino acids • Urea Renal Tubule • Filtrate proceeds to renal tubules from glomerulus • Proximal convoluted tubule • Nephron loop • Descending limb • Descending thin limb (DTL) • Ascending thin limb (ATL) • Thick ascending limb (TAL) • Distal convoluted tubule Renal Tubule • Collecting ducts • Receive urine from several nephrons • Play an important role in conserving body fluids • Posterior pituitary secretes ADH • Increases permeability of collecting ducts and distal convoluted tubules to water Classes of Nephron • Cortical nephrons • 85% of nephrons • Juxtamedullary nephrons • 15% of nephrons • Contribute to kidney’s ability to concentrate urine Blood Vessels Associated with Nephrons • Nephrons associate closely with two capillary beds • Glomeruli • Peritubular capillaries in cortical nephrons or vasa recta in juxtamedullary nephrons Blood Vessels Associated with Nephrons • Glomeruli • Produce filtrate that becomes urine • Fed and drained by arterioles • Afferent glomerular arteriole • Efferent glomerular arteriole Blood Vessels Associated with Nephrons • Glomeruli • Efferent arteriole has a smaller diameter than afferent arteriole • Generate 1 liter of fluid every 8 minutes • 99% of filtrate is resorbed by tubules Blood Vessels Associated with Nephrons • Peritubular capillaries • Arise from the efferent arterioles draining cortical glomeruli • Are adapted for absorption • Low-pressure, porous capillaries • All molecules secreted by nephrons into urine are from peritubular capillaries Blood Vessels Associated with Nephrons • Vasa recta • Continue from efferent arterioles of juxtamedullary nephrons • Are thin-walled looping vessels • Descend into the medulla • Are part of the kidney’s urine concentrating mechanism 24 PART 3 The Urinary System Juxtaglomerular Complex • Juxtaglomerular complex • Functions in regulating blood pressure • An area of specialized contact between terminal end of the ascending limb and afferent arteriole • Granular cells—modified smooth muscle cells with secretory granules • Contain the hormone renin • Renin—secreted in response to falling blood pressure in afferent arteriole Juxtaglomerular Complex • Macula densa—end of nephron loop • Adjacent to granular cells • Tall, closely packed epithelial cells • Monitor solute concentration in the filtrate • Signal granular cells to secrete renin • Initiates renin-angiotensin mechanism Juxtaglomerular Complex • Mesangial cells • Located around base of the glomerulus • Regulate blood flow within the glomerulus • Extraglomerular mesangial cells • Interact with macula densa and granular cells • Help regulate blood pressure Ureters • Carry urine from the kidneys to the urinary bladder • Oblique entry into bladder prevents backflow of urine • Histology of ureter • Mucosa—transitional epithelium • Muscularis—two layers • Inner longitudinal layer • Outer circular layer • Adventitia—typical connective tissue Urinary Bladder • A collapsible muscular sac • Stores and expels urine • Full bladder—spherical • Expands into the abdominal cavity • Empty bladder—lies entirely within the pelvis Urinary Bladder • Urachus—closed remnant of the allantois • Prostate • In males • Lies directly inferior to the bladder • Surrounds the urethra Urinary Bladder • Urinary bladder is composed of three layers • Mucosa—transitional epithelium • Thick muscular layer—detrusor • Fibrous adventitia Urethra • Epithelium of urethra • Transitional epithelium • At the proximal end (near the bladder) • Stratified and pseudostratified columnar—mid urethra (in males) • Stratified squamous epithelium • At the distal end (near the urethral opening) Urethra • Internal urethral sphincter • Involuntary smooth muscle • External urethral sphincter • Voluntarily inhibits urination • Relaxes when one urinates Urethra • In females • Length of 3–4 cm • In males—20 cm in length; three named regions • Prostatic urethra • Passes through the prostate gland • Intermediate part of urethra • Through the urogenital diaphragm • Spongy (penile) urethra • Passes through the length of the penis Disorders of the Urinary System • Urinary tract infections • More common in females • Burning sensation during micturition • Renal calculi • Kidney stones • Bladder cancer • 3% of cancers—more common in men • Kidney cancer • Arises from epithelial cells of uriniferous tubules The Urinary System Throughout Life • Embryo develops three pairs of kidneys • Pronephros • Mesonephros • Metanephros • Only metanephros persists to become the adult kidneys • Metanephric kidney produces urine by fetal month 3 • Contributes to the volume of amniotic fluid The Urinary System Throughout Life • Kidney and bladder function declines with advancing age • Nephrons decrease in size and number • Tubules are less efficient at secretion and resorption • Filtration declines • Recognition of desire to urinate is delayed • Loss of muscle tone in the bladder