Erythema Multiforme - developinganaesthesia
advertisement

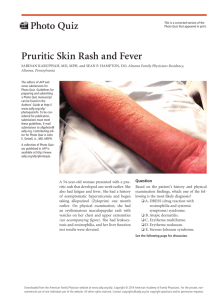
ERYTHEMA MULTIFORME Introduction Erythema Multiforme (EM) is considered to be the mild and benign form of a range of skin reactions that include Erythema multiforme (EM), Stevens-Johnson syndrome (SJS) and Toxic epidermal necrolysis (TEN) Stevens-Johnson syndrome is usually characterized by extensive mucosal involvement and systemic illness and toxic epidermal necrolysis is the most severe form characterized by more extensive skin and mucosal involvement and more serious systemic illness. These skin diseases are thought to have a common underlying auto-immunological mechanism and so are thought to be manifestations of the same disease process that can have a range of possible triggering causes. See separate guidelines for Stevens - Johnson syndrome. Pathology Causes include: 1. Idiopathic ● 2. Many cases are idiopathic, with no cause being clearly identified. Infective: Viral: ● Herpes simplex virus is the most commonly implicated infective agent in EM. Bacterial: ● Mycoplasma pneumonia 3. Drug reaction: 4. Chemical toxins Less commonly: 5. Malignancy: 6. Connective tissue disease. Clinical assessment Skin lesions: Left: Typical target lesion of erythema multiforme. Right: Raised atypical targets and arcuate lesions. 3 Classic “target lesions” help establish the diagnosis of erythema multiforme. Characteristics include: 1. Discrete round to oval lesions 2. These are triphasic target (or iris-like) lesions with: ● A central purple or dusky area ● Surrounded by a whitish oedematous concentric rim ● Surrounded again by a red halo. 3. As the lesions evolve, a central blister or erosion may occur. 4. Multiforme” lesions: ● 5. Scattered “multiforme” lesions are seen as a concentric pattern mix of erythematous macules, papules, vesicular and target lesions up to a few centimetres in diameter. Lesions are predominantly seen on: ● The face ● Distal limbs ● Less often, the proximal limbs and the trunk. 6. Pruritus is not a typical feature. 7. Some target lesions may involve mucosal areas, particularly the lips, but significant oral involvement, is only seen in SJS or TEN Prognosis EM not associated with any mortality. Time course Most cases are self-limited and resolve without sequelae within 2-4 weeks Differentiating EM from SJS and TEN: An important aspect of the clinical assessment of a patient with suspected erythema multiforme will be to distinguish this benign condition from the much more serious SJS or TEN SJS and TEN are rare diseases that are characterised by: 1. Moderate to extensive generalized mucocutaneous exfoliation resulting from epidermal cell death. By somewhat arbitrary convention: 2. ● SJS involves less than 10% body surface area skin shedding, (and has a 5% mortality) ● SJS-TEN overlap cases involve 10% to 30% of the body surface area skin shedding. ● TEN, involves more than 30% of the body surface area skin shedding (and is associated with a mortality of 20% to 30 %!) Systemic illness: ● Fever ● Constitutional symptoms, i.e. malaise, lethargy, anorexia, headache, myalgias, arthralgias. Investigations In clear cut cases, where the patient remains well, no particular investigations may be necessary at all. In selected patients with other suggestive symptoms a search for underlying malignancy or rheumatological disease may be considered. In cases where patients appear unwell bloods tests or others as indicated may need to be done. Skin biopsy of lesions may be considered in equivocal cases. Management There is no specific treatment and so management is symptomatic and supportive Avoid any suspected triggers, such as drugs, and advise the patient accordingly. Antiviral prophylaxis is considered those patients with frequent herpes simplex associated recurrences. Topical corticosteroids may provide some benefit, but systemic steroids are not indicated. Disposition Urgent dermatological review is only required when there is a need to distinguish the presentation from SJS or TEN. References 1. Dermatology Therapeutic Guidelines 3rd ed 2009 2. Bastuji-Garin S, Rzany B, Stern RS. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. Jan 1993; 129(1):92-6 3. O. Ogundele: Erythema Multiforme in Emergency Medicine, eMedicine Website, November 2010. Dr J. Hayes August 2011.