Hematology Case Study 4 - Cal State LA
advertisement

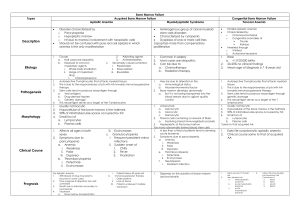
Hematology Case Study 4 Rachael, a 13-year old female, was admitted to the hospital with complaints of progressive weakness and shortness of breath with minimal physical effort. She has experienced recurrent fevers reaching 1020 F. Physical examination reveals a welldeveloped adolescent with good nutritional status and in no acute distress. There is no lymphadenopathy or organomegaly. Many petechial hemorrhages cover her chest and legs. Several bruises are found on her legs and thighs. Laboratory tests were ordered on admission. 1. What laboratory tests would be appropriate for screening for aplastic anemia? A CBC 2. Justify your selection of tests based on Rachael’s clinical signs and symptoms. A CBC is an important screening test for all anemias. It is important to know the patient’s hemoglobin and hematocrit, as anemia may be one cause of weakness and shortness of breath. A low platlet count may explain the presence of petechiae and bruises. Rachael is a 13-year old female. 3. If aplastic anemia is present, would you expect her to have an idiopathic or secondary form? Explain your answer. It is difficult to estimate the cause without a more complete history. Idiopathic forms are more common in this age group. For the past 3 months, Rachael’s family physician has been following her recovery from viral hepatitis. Her recovery was uneventful, with her liver enzyme levels returning to normal within two months. She has no other past medical history. There is no family history of hematologic disorders. 4. What aspect of this patient’s history may be associated with the occurrence of aplastic anemia? There is data suggesting an association with aplastic anemia and certain viral infections 5. Is it likely that Rachael has a congenital form of aplastic anemia? It is unlikely because it would have been detected at a younger age than Rachael currently is. Rachael has complaints of progressive weakness and shortness of breath with minimal physical effort. She has experienced recurrent fevers reaching 1020 F. Many petechial hemorrhages cover her chest and legs, and several bruises are found on her legs and thighs. 6. Correlate these clinical findings with her laboratory screening test results, which follow: Admission laboratory data for patient: RBC: 2.42 x 1012/L HGB: 7.1 gd/L HCT: 24% PLT: 8.0 x 109/L WBC: 1.2 x 109/L Differential: Segmented neutrophils: Lymphocytes: Monocytes: Uncorrected reticulocyte count: 2% 94% 4% 0.7% The patient’s weakness and shortness of breath are due to the anemia. The petechiae and bruising are due to low platlets. The recurrent infections are suggestive of infection. She is neutropenic and, therefore, at high risk for infection. 7. Evaluate each of he patient’s laboratory results by comparing them to reference ranges. All CBC parameters are low 8. Which of the patient’s routine laboratory results are consistent with those expected for aplastic anemia? All are consistent with those expected for aplastic anemia 9. Classify the morphologic type of anemia. Normocytic, hypochromic 10. Calculate the absolute lymphocyte count. Are her lymphocytes truly elevated as suggested by the relative lymphocyte count? The absolute lymphocyte count is 1.1 x 109/L which is slightly decreased. The relative lymphocytosis is high due to the severe neutropenia 11. Correct the reticulocyte count. Why is this step important? The corrected reticulocyte count is 0.4%, which is below the reference range. All reticulocyte counts need to be corrected when anemia is present in order to assess the bone marrow’s degree of compensation for anemia. 12. Calculate the absolute reticulocyte count. The absolute reticulocyte count is 16.9x109/L and this is consistent with a diagnosis of aplastic anemia Rachael was referred to a hematologist who ordered a bone marrow examination. The aspirate obtained was inadequate for evaluation due to lack of marrow. Only a single site could be aspirated. Preps made from the aspirate showed a markedly hypocellular marrow with very few hematopoietic cells. Cells present consisted of lymphocytes, plasma cells, and stromal cells. There were no malignant cells present. 13. Compare these results with those expected with a person with aplastic anemia. A markedly hypoplastic bone marrow is consistent with a diagnosis of aplastic anemia. 14. Interpret the significance of the lack of malignant cells and hematopoietic blasts. If malignant cells were present, a diagnosis of metastatic disease or lymphoma would have been likely. Bone marrows of patients with leukemia or myelodysplastic syndromes typically are hyperplastic with increased numbers of hematopoietic blasts present. 15. Appraise the prognosis for Rachael. The prognosis is poor unless a compatible bone marrow donor is found. 16. Predict a treatment regime. Treatment would be supportive therapy using blood components. Platlets should be administered immediately and a bone marrow donor should be searched for. 17. What other hematologic conditions needed to be ruled out for this patient? Myelodysplastic syndromes and megaloblastic anemia (both lead to pancytopenia) 18. What laboratory test would be most beneficial in differentiating aplastic anemia from these other disorders? Compare the results for aplastic anemia with those of the other disorders. B12 and folic acid levels could be used to rule out anemia due to a deficiency in either of these. However, a bone marrow was necessary to make a definitive diagnosis. If the anemia were a megaloblastic anemia or a myelodysplastic syndrome, it would be hyperplastic.