Appendix 1 - the CBMTG 0801
advertisement

Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
A Randomized Trial of Thymoglobulin® to Prevent
Chronic Graft versus Host Disease in Patients
Undergoing Hematopoietic Progenitor Cell
Transplantation (HPCT) from Unrelated Donors
Sponsor:
McMaster University, Faculty of Health Science
1200 Main Street West
Hamilton, Ontario
LZN 3Z5
Study Chair:
Dr. Irwin Walker
Study Number: CBMTG 0801
Version Date: 15-Jan-2011
Summary of Protocol Versions
Version No.
1
2
3
4
Date
24-Nov-2009
23-Dec-2009
08-Feb-2010
15-Jan-2011
Comments
Preliminary version of the protocol. Submitted to McMaster IRB only.
Submitted to Health Canada & McMaster IRB. Not distributed to sites.
First version distributed to participating sites.
Includes Notification of Changes #1 (see Memo 001 dated 07-Jun2010) & Notification of Changes # 2 (see Memo 002 dated 13-Aug2010) and subsequent revisions up until 15-Jan-2011
Page 1 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
CONTENTS
1.
2.
3.
4.
Protocol Signature Page…………………………………………………………………………..6
Project Committees .............................................................................................................. ..7
Canadian Adult Allogeneic Transplant Centres ...................................................... 13
Hypothesis and End-Points.............................................................................................. 15
4.1.
4.2.
4.3.
Hypothesis ........................................................................................................................ 15
Primary End-Point ............................................................................................................. 15
Secondary End-Points ........................................................................................................ 15
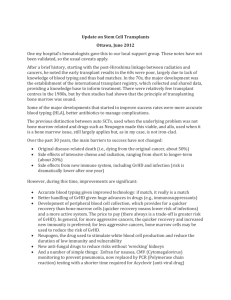
5. Project Summary .................................................................................................................. 16
6. Overview of Study Design................................................................................................. 17
7. Background............................................................................................................................. 19
7.1.
7.2.
7.3.
7.4.
7.5.
7.6.
7.7.
Chronic Graft versus Host Disease ...................................................................................... 19
The Principal Research Question to be Addressed ............................................................... 20
Rationale .......................................................................................................................... 20
Previous Studies ................................................................................................................ 21
Conclusions ....................................................................................................................... 22
Safety Considerations ........................................................................................................ 22
Thymoglobulin® ................................................................................................................ 23
8. Eligibility and Study Entry ............................................................................................... 25
8.1. Inclusion Criteria ............................................................................................................... 26
8.2. Exclusion Criteria ............................................................................................................... 26
8.3. Preparative Regimens ....................................................................................................... 27
8.3.1.
Myeloablative Preparative Regimens ................................................................................. 27
8.3.2.
Non-myeloablative (RIC) ..................................................................................................... 28
8.4. Donor Selection ................................................................................................................. 28
8.5. Informed Consent .............................................................................................................. 28
8.6. Protocol Approval ............................................................................................................. 29
8.7. Registration and Minimization (Randomization) ................................................................ 29
8.7.1 Participants Who Become Ineligible Following Randomization………………………………….…..28
8.7.1.1
8.7.1.2
8.7.1.3
Delayed Transplant…………………………………………………………………….……………….29
Cancelled Transplant……………………………………………………….…………………………..29
Transplant Proceeds (Inclusion/Exclusion Criteria Not Met)…….……………………..….….29
9. Treatment Plan ..................................................................................................................... 30
9.1. Overview .......................................................................................................................... 31
9.2. Source of Progenitor Cells .................................................................................................. 31
9.3. Preparative Regimens ....................................................................................................... 31
9.3.1.
Myeloablative Preparative Regimens ................................................................................. 31
9.3.2.
Non-myeloablative (RIC) Preparative Regimens ................................................................. 32
9.4. Administration of Thymoglobulin® (ARM B ONLY).............................................................. 32
9.5. Graft Versus Host Disease Prophylaxis ............................................................................... 32
9.5.1.
Methotrexate ...................................................................................................................... 33
9.5.2.
Mycophenolic Acid .............................................................................................................. 35
Page 2 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
9.5.3.
Cyclosporine and Tacrolimus .............................................................................................. 35
9.6. Co-Enrollment in Other Clinical Trials ................................................................................. 35
9.7. Graft versus Host Disease Diagnosis................................................................................... 36
9.8. Acute Graft versus Host Disease Treatment ........................................................................ 36
9.9. Chronic Graft versus Host Disease Treatment ..................................................................... 36
9.10. Supportive Care ................................................................................................................. 37
9.10.1. Veno-occlusive Disease Prophylaxis ................................................................................... 37
9.10.2. Antibacterial Prophylaxis During the Neutropenic Period.................................................. 37
9.10.3. Herpes Simplex Virus (HSV) Prophylaxis ............................................................................. 37
9.10.4. Antifungal Prophylaxis ........................................................................................................ 37
9.10.5. Management of Cytomegalovirus (CMV) ........................................................................... 37
9.10.6. Management of Epstein Barr Virus (EBV) ........................................................................... 37
9.10.7. Pneumocystitis Carinii Prophylaxis ..................................................................................... 39
9.10.8. Blood Product Support ........................................................................................................ 39
9.10.9. Administration of Growth Factors Following Graft Infusion............................................... 39
9.10.10. Prophylactic Intravenous Gammaglobulin ......................................................................... 39
9.10.11. Maintenance Therapy with TKI Inhibitors .......................................................................... 38
10.
Required Observations and Information ......................................................... 39
10.1. Pre-Transplant Clinical Evaluations .................................................................................... 39
10.2. Pre-Transplant Questionnaires .......................................................................................... 39
10.3. Hematopoietic Progenitor Cell Product Information ........................................................... 40
10.3.1. Peripheral Blood Progenitor Cell Product ........................................................................... 40
10.3.2. Bone Marrow Product......................................................................................................... 41
10.4. Post-Transplant Clinical Evaluations .................................................................................. 41
10.5. Post-Transplant Questionnaires ......................................................................................... 41
11.
Evaluation of Outcomes ........................................................................................... 43
11.1. Primary Endpoint .............................................................................................................. 43
11.2. Secondary Endpoints ......................................................................................................... 43
11.2.1. Time to Engraftment (Hematological Recovery) ................................................................ 43
11.2.2. Chimerism……………………………………………………………………………………………………………………..42
11.2.3. The Incidence of Acute GVHD ............................................................................................. 42
11.2.4. Date of Diagnosis of chronic GVHD…………………………………………………………….…..……………..43
11.2.5. The Incidence of Chronic GVHD According to NIH Consensus Guidelines.......................... 44
11.2.6. The Incidence of Chronic GVHD According to Sullivan Criteria .......................................... 44
11.2.7. Time to Non-relapse Mortality ........................................................................................... 44
11.2.8. Time to All-cause Mortality................................................................................................. 44
11.2.9. Time to Relapse of Hematologic Malignancy...................................................................... 43
11.2.10. Graft Rejection or Failure (Yes vs. No) ................................................................................ 45
11.2.11. Serious Infection ................................................................................................................. 45
11.2.12. CMV Activation ................................................................................................................... 45
11.2.13 Organ Specific and Global Severity Ratings of Chronic Graft versus Host Disease (NIH
Consensus Guidelines)……………………………………………………………………………………………….…..44
11.2.14. Number of months on immunosuppression up to 12 months post transplant…………….…44
11.2.15 Doses of Immunosuppressive Therapy Required at 12 Months………………………….….………44
11.2.16 Resumption of Immunosuppressive Therapy after 12 Months…………………………..………….45
Page 3 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
11.2.17 Presence or Absence of Immunosuprressive Therapy at 24 Months…………..…………………45
11.2.18. Quality of Life...................................................................................................................... 46
11.2.19. Economic Analysis .............................................................................................................. 47
11.3
Collection of Additional Data…………………………………….………………………………………………….………48
12.
13.
13.1.
13.2.
13.3.
13.4.
13.5.
13.6.
13.7.
14.
Criteria for Removal from Protocol Therapy and Off Study Criteria .... 49
Statistical Considerations........................................................................................ 50
Data Management ............................................................................................................ 50
Sample Size Calculation ..................................................................................................... 50
Stratification/Minimization ............................................................................................... 51
Analysis ............................................................................................................................ 52
Interim Analysis ................................................................................................................ 54
Handling of Missing Data .................................................................................................. 55
Loss to Follow-up............................................................................................................... 54
Adverse Events and Serious Adverse Events ................................................. 55
14.1. Definitions ........................................................................................................................ 55
14.1.1. Definition of an Adverse Event ........................................................................................... 55
14.1.2. Definition of a Serious Adverse Event (SAE) ....................................................................... 55
14.1.3. Definition of an Unexpected Adverse Reaction .................................................................. 56
14.1.4. Attribution of Causality and Definitions ............................................................................. 56
14.2. Adverse Event Monitoring and Source Documentation ....................................................... 56
14.3. Adverse Event Reporting ................................................................................................... 57
14.4. Grading of Adverse Events ................................................................................................. 57
14.5. Serious Adverse Event (SAE) Reporting Criteria (Sites) ........................................................ 57
14.5.1. Reporting of Participant Deaths (Sites)............................................................................... 58
14.6. Reporting of Secondary Malignancies (Sites) ...................................................................... 58
14.7. Pregnancies (Sites) ............................................................................................................ 57
14.8. Reporting of Serious Adverse Events to Government Regulatory Agencies .......................... 58
14.8.1. Canada ................................................................................................................................ 58
14.8.2. International Sites ............................................................................................................... 59
14.9. SAE Notifications ............................................................................................................... 59
14.10. Reporting of SAEs to Institutional Review Boards (IRB’s)..................................................... 59
14.11. Reporting of SAEs to Genzyme ........................................................................................... 59
14.12. Review of SAE's by the Medical Monitor and Statistician…………………………………………………….58
15.
16.
16.1.
16.2.
16.3.
16.4.
17.
Data Safety Monitoring Committee..................................................................... 60
Records and Reporting............................................................................................. 59
Data Management ............................................................................................................ 59
Data Entry, Confidentiality and Security ............................................................................. 61
Specific Instructions to Participating Sites Regarding 16.2 .................................................. 61
Access to Database and Statistical Analysis ........................................................................ 60
Regulatory Ethics Compliance .............................................................................. 62
17.1. Investigator Responsibilities .............................................................................................. 62
17.2. Independent Ethics Committee or Institutional Review Board ............................................. 62
18.
19.
Study Monitoring and Auditing ............................................................................ 62
Drug Accountability……. ………………...…..…………………………………………..62
Page 4 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Appendix 1 –Informed Consent Templates .................................................................... 64
Appendix 2 – Karnofsky Functional Scale ....................................................................... 84
Appendix 3 – Schedule of Events ........................................................................................ 85
Appendix 4 – Registration and Randomization (Minimization) Form ............... 88
– Confirmation of Eligibility/Change in Eligibility Form...………....92
Appendix 5 - Suggested Orders for Administration of Thymoglobulin® .......... 95
Appendix 6 – Regimen Related Toxicity: Bearman Toxicity Scale........................ 96
Appendix 7 – Acute Graft Versus Host Disease Staging and Grading .................. 97
Appendix 8 – Sullivan Criteria ............................................................................................. 98
Appendix 9 – Chronic GVHD Assessment Form............................................................ 99
Appendix 10 – Co-morbidities (HCT-CI) ........................................................................ 105
Appendix 11 – References.................................................................................................... 107
Page 5 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
1. Protocol Signature Page
I have read the protocol, “A Randomized Trial of Thymoglobulin® to Prevent Chronic Graft
versus Host Disease in Patients Undergoing Hematopoietic Progenitor Cell Transplantation
(HPCT) from Unrelated Donors” dated 15-Jan-2011, and agree to conduct the study according
to the protocol and the applicable ICH guidelines and GCP regulations, and to inform all who
assist me in the conduct of this study of their responsibilities and obligations.
Investigator’s Signature
Date
_________________
Investigator’s Name (Print)
____________________________________________________________
Study Site (Print)
Page 6 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
2. Project Committees
2.1. Steering Committee
Irwin Walker
Study Chair and
Department of Medicine
Juravinski Hospital and Cancer Centre
711 Concession Street
Medical Monitor
Hamilton, Ontario, Canada, L8V 1C3
Telephone: (905) 521-2100, ext 76384
Fax: (905) 575-7320
Email: walkeri@mcmaster.ca
Stephen Couban
Queen Elizabeth II Health Sciences Centre
Bethune Building, Room 431
1278 Tower Road
Halifax, Nova Scotia, Canada, B3H 2Y9
Telephone: (902) 473-7006
Fax: (902) 473-4420
Email: stephen.couban@cdha.nshealth.ca
Jean Roy
Hôpital Maisonneuve-Rosemont
5415 Assomption Boulevard
Montréal, Québec, Canada, H1T 2M4
Telephone : (514) 252-3404
Fax: (514) 254-5094
Email: jroy.hmr@ssss.gouv.qc.ca
Ronan Foley
Department of Pathology & Medicine
McMaster University
711 Concession Street
Juravinski Hospital and Cancer Centre
Hamilton, Ontario, Canada , L8V 1C3
Telephone: (905) 527-4322, ext 42075
Fax: (905) 575-2553
Email: foleyr@hhsc.ca
Kirk Schultz
BC Children’s Hospital
4480 Oak Street
Vancouver, BC, Canada, V6H 3V4
Telephone: (604) 875-2316
Fax: (604) 875-2911
Email: kschultz@interchange.ubc.ca
Page 7 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Cynthia Toze
Leukemia/BMT Program of British Columbia
Vancouver General Hospital
Gordon and Leslie Diamond Health Care Centre
10th Floor, 2775 Laurel Street
Vancouver, British Columbia, Canada, V5Z 1M9
Telephone: (604) 875-4863
Fax: (604)875-4763
Email: ctoze@bccancer.bc.ca
Stephanie Lee
Fred Hutchinson Research Centre
1100 Fairview Avenue North, D5-290
P.O. Box 19024
Seattle, Washington, United States, 98109
Telephone: (206) 667-5160
Fax: (206) 667-1034
Email: sjlee@fhcrc.org
Holly Kerr
Project Manager
Vancouver General Hospital
Gordon and Leslie Diamond Health Care Centre
10th Floor (Room 10133), 2775 Laurel Street
Vancouver, British Columbia, Canada, V5Z 1M9
Telephone: (604) 875-4111, ext 63196
Fax: (604) 875-5584
Email: hkerr@bccancer.bc.ca
David Szwajcer
University of Manitoba
ON2064-675 McDermot Ave
Winnipeg, Manitoba, Canada, R3E 0V9
Telephone: (204) 787-4179
Fax: (204) 786-0196
Email: david.szwajcer@cancercare.mb.ca
Tony Panzarella
Director, Department of Biostatistics
Princess Margaret Hospital
610 University Avenue
Toronto, Ontario, Canada, M5G 2M9
Telephone: (416) 946-4501, ext 4881
Fax: (416) 946-2048
Email: tony.panzarella@uhnres.utoronto.ca
Page 8 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
2.2. Study Statistician
Tony Panzarella
Director, Department of Biostatistics
Princess Margaret Hospital
610 University Avenue
Toronto, Ontario, Canada, M5G 2M9
Telephone: (416) 946-4501, ext 4881
Fax: (416) 946-2048
Email: tony.panzarella@uhnres.utoronto.ca
2.3. Quality of Life Studies
Cynthia Toze
Leukemia/BMT Program of British Columbia
Vancouver General Hospital
Gordon and Leslie Diamond Health Care Centre
10th Floor, 2775 Laurel Street
Vancouver, British Columbia, Canada, V5Z 1M9
Telephone: (604) 875-4863
Fax: (604) 875-4763
Email: ctoze@bccancer.bc.ca
Stephanie Lee
Fred Hutchinson Research Centre
1100 Fairview Avenue North, D5-290
P.O. Box 19024
Seattle, Washington, United States, 98109
Telephone: (206) 667-5160
Fax: (206) 667-1034
Email: sjlee@fhcrc.org
2.4. Coordinating Centre
John Shepherd
Supervisor and Head BMT Program
Leukemia/BMT Program of British Columbia
Vancouver General Hospital
Gordon and Leslie Diamond Health Care Centre
10th Floor, 2775 Laurel Street
Vancouver, British Columbia, Canada, V5Z 1M9
Telephone: (604) 875-4863
Fax: (604) 875-4763
Email: jshepher@bccancer.bc.ca
Page 9 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Holly Kerr
Project Manager
Vancouver General Hospital
Gordon and Leslie Diamond Health Care Centre
10th Floor (Room 10133), 2775 Laurel Street
Vancouver, British Columbia, Canada, V5Z 1M9
Telephone: (604) 875-4111, ext 63196
Fax: (604) 875-5584
Email: hkerr@bccancer.bc.ca
2.5.
Economic Studies
David Szwajcer
University of Manitoba
ON2064-675 McDermot Ave
Winnipeg, Manitoba, Canada, R3E 0V9
Telephone: (204) 787-4179
Fax: (204) 786-0196
Email: david.szwajcer@cancercare.mb.ca
Page 10 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
2.6. Data Safety and Monitoring Committee
Pediatric Blood and Marrow Transplantation Consortium
Data Safety and Monitoring Committee (PBMTC DSMC)
Kamar Godder, MD (Chair)
Pediatric BMT physician, PBMTC Member
Virginia Commonwealth University Health System-MCV
Pediatric Hematology/Oncology
1101 East Marshall Street, P. O. Box 980121
Richmond, Virginia, United States, 23298-0121
Phone: (804) 828-9605
Fax: (804) 828-0386
Email: kgodder@vcu.edu
Paul J. Martin MD
Adult BMT Physician
Fred Hutchinson Cancer Research Center
1100 Fairview Avenue N, D2-100
Seattle, Washington, United States, 98109-4798
Phone: (206) 667-4798
Fax: (206) 667-5255
Email: pmartin@fhcrc.org
Shaun Tumpane
Patient advocate
630 NW Alpine Terrace
Portland, Oregon, United States, 97210
Phone: (503) 243-4747
Fax: (503) 243-3636
Cell: (503) 701-7781
Email: stumpane@aol.com
Robyn Dillon, MSW LCSW
Virginia Commonwealth University
Department of Care Coordination
P.O. BOX 980104
Richmond, Virginia, United States, 23298
Phone: (804) 628-0422
Fax: (804) 828-0504
Email: rdillon@vcu.edu
Page 11 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Becky McMullin, RN, BSN
MD Anderson Cancer Center
Pediatrics
1515 Holcombe Blvd, Unit 87
Houston, Texas, United States, 77030
Phone: (713) 794-4823
Fax: (713) 794-4373
Email: bmcmulli@mdanderson.org
Page 12 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
3. Canadian Adult Allogeneic Transplant Centres
Royal Victoria Hospital
687 Pins Avenue
Montreal, QC H3A 1A1
Canadian Blood and Marrow
Transplantation Group – Clinical Trials
Network
Vancouver Hospital & Health Sciences
Centre
855 West 12th Avenue
Vancouver, BC V5Z 4E3
CancerCare Manitoba
675 McDermot Ave., Rm 2083
Winnipeg, MB R3N 1A5
Princess Margaret Hospital
610 University Avenue
Toronto, ON M5G 2M9
Hamilton Health Sciences
1200 Main Street W.
Hamilton, ON L8N 3Z5
The Ottawa Hospital
501 Smyth Road
Ottawa, ON K1H 8L6
Director: Dr Pierre Laneuville
Phone: (514) 843-1558 ; Fax: (514) 843-1418
E-mail : Laneuvillep@muhchem.mcgill.ca
Local Principal Investigator: Gizelle Popradi
Study Coordinator: Suzanne Gosselin
Chair: Dr. Ronan Foley
Phone: (905) 527-4322 x42075 Fax: (905) 575-2553
E-mail: foleyr@hhsc.ca
Director: Dr. John Shepherd
Phone: 604-875-4863; Fax: 604-875-4763
E-mail: jshepher@bccancer.bc.ca
Local Principal Investigator: Dr. Thomas Nevill
Study Coordinator: Holly Kerr
Director: Dr. Donna Wall
Phone: (204) 787-1992; Fax: 204-786-0196 Email:
donna.wall@cancercare.mb.ca
Local Principal Investigator : Dr. David Szwajcer
Study Coordinator: Erin Richardson
Director: Dr. John Kuruvilla
Phone: (416) 946-4466; Fax: 416-946-2983
E-mail: John.Kuruvilla@uhn.on.ca
Local Principal Investigator: Dr. John Kuruvilla
Study Coordinator: Sonal Malhotra
Director: Dr. Irwin Walker
Phone: (905) 521-2100 x 76384; Fax: 905-521-4971
E-mail: walkeri@mcmaster.ca
Local Principal Investigator: Dr. Irwin Walker
Study Coordinator: Tammy DeGelder
Director: Dr. Lothar Huebsch
Phone: (613) 737-8158; Fax: 613-737-8861
E-mail: lhuebsch@ottawahospital.on.ca
Local Principal Investigator: Dr. Jason Tay
Study Coordinator: Mai Le
Page 13 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Hôtel-Dieu de Québec
11, côte du Palais
Québec (Québec) G1R 2J6
Hôpital Maisonneuve-Rosemont
2nd Floor, Block 4, 5415 boulevard de
l’Assomption
Montréal, QC H1T 2M4
CHA Hôpital Enfant-Jésus
1050, chemin Sainte-Foy
Québec, QC GIS 4L8
Queen Elizabeth II Health Sciences
Centre
Bethune Building, Room 417, 1278
Tower Road
Halifax, NS B3H 2Y9
Director : Dr Félix Couture
Phone: (418) 691-5225; Fax: (418) 691-5383
Email: felixcou@videotron.ca
Local Principal Investigator: Dr. Félix Couture
Study Coordinator: Theresa Jones
Director: Dr. Jean Roy
Phone: (514) 252-3404; Fax: (514) 254-5094
E-mail: jean.roy@ssss.gouv.qc.ca
Local Principal Investigator: Dr. Jean Roy
Study Coordinator: Johanne Blais
Director: Dr. Guy Cantin
Phone: (418) 649-5727
Local Principal Investigator: Dr. Genieviève Gallagher
Study Coordinator: Yolaine Hébert
Director: Dr. Stephen Couban
Phone: (902) 473-7006; Fax: 902-473-4420
E-mail: stephen.couban@cdha.nshealth.ca
Local Principal Investigator: Dr. Stephen Couban
Study Coordinator: Val Dorcas
Page 14 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
4. Hypothesis and End-Points
4.1. Hypothesis
The addition of Thymoglobulin® to the preparative regimen will result in a decrease in the
proportion of patients with chronic graft versus host disease, resulting in improved quality of life
but without an increase in mortality, disease relapse or death due to infection.
4.2. Primary End-Point
Freedom of chronic graft versus host disease at 12 months from transplantation defined as
withdrawal of all systemic immunosuppressive agents without resumption up to 12 months after
transplantation (this end-point is binary i.e. Yes/No).
4.3. Secondary End-Points
1
Time to engraftment
Chimerism at day 30, 60 and 100 & 6 months post HPCT (non-myeloablative/RIC cohort only)
Incidence of acute GVHD
Date of diagnosis of chronic GVHD according to NIH Consensus Guidelines
Incidence of chronic GVHD according to NIH Consensus Guidelines
Incidence of chronic GVHD according to Sullivan Criteria1
Time to non-relapse mortality
Time to all-cause mortality
Time to relapse of hematologic malignancy
Incidence of graft rejection or failure
Incidence of serious infection
Incidence of CMV activation
Incidence of specific organ grades (NIH) of chronic graft versus host disease
Number of months on immunosuppression up to 12 months post transplant
Doses of immunosuppressive therapy at 12 months
Resumption of immunosuppressive therapy after 12 months
Presence or absence of immunosuppressive therapy at 24 months (Yes/No)
Quality of life
Cost effectiveness
Information entered in the Chronic GVHD Assessment Form (Appendix 9) will be used to determine the
Sullivan grades (limited vs. extensive vs. no chronic gvhd) at 100 days, 6 months, 12 months and 24 months. (A
reviewer from the Study Committee (or delegate) will determine the Sullivan grade at these time points).
Page 15 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
5. Project Summary
Title
A Randomized Trial of Thymoglobulin® to Prevent Chronic Graft
versus Host Disease in Patients Undergoing Hematopoietic Progenitor
Cell Transplantation (HPCT) from Unrelated Donors
Hypothesis
The addition of Thymoglobulin® to the preparative regimen will result
in a decrease in the proportion of patients with chronic graft versus
host disease, resulting in improved quality of life but without an
increase in mortality, disease relapse or deaths due to infection
Design
Multicentre, Non-Blinded, Randomized Controlled Trial
Sponsor
McMaster University, Faculty of Health Sciences, Hamilton, Ontario
Administrative Support
Canadian Blood and Marrow Transplant Group (CBMTG)
Funding
Canadian Institutes for Health Research: CA$1,245,055
Genzyme Corporation: US$800,000
198 patients
Sample size
Primary endpoint
Freedom from chronic graft versus host disease at 12 months from
transplantation defined as withdrawal of all systemic
immunosuppressive agents without resumption up to 12 months after
transplantation
Inclusion Criteria
Patients are aged 16-70 undergoing BMT using matched* unrelated
donor graft, myeloablative OR RIC, for any hematologic malignancy
Exclusion Criteria
Poor condition (centre determined), acute leukemia in relapse (<10%
blasts), second transplants, active infection, HIV infection, T-cell
antibody prophylaxis (antithymocyte globulin, anti-CD52 etc), use of
cord blood grafts, T-cell depletion of grafts
Preparative Regimens
According to centre protocol (to be declared at outset of trial)
Supportive measures
Institutional practices. Quantitative EBV testing is strongly
recommended.
Thymoglobulin®
4.5 mg/kg total dose (schedule: 0.5 mg/kg day -2; 2.0 mg/kg days -1
and +1)
* Fully MHC matched at HLA-A, B, C, and DRB1 loci or 1-antigen or 1–allele mismatched at either HLA-A,
Page 16 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
B, C or DRB1 loci.
6. Overview of Study Design
Page 17 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Assess Eligibility
Eligible Recipient
Donor
Informed Consent
Registration
Minimization
Standard Arm
No Thymoglobulin
Experimental Arm
Thymoglobulin
Institutional
Conditioning, GVHD
Prophylaxis and
Supportive Care
Institutional
Conditioning, GVHD
Prophylaxis and
Supportive Care
24-Month Follow-Up
24-Month Follow-Up
Page 18 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
7. Background
7.1. Chronic Graft versus Host Disease
Chronic graft versus host disease (cGVHD) is the most common long term complication of HPCT,
affecting 40-50% of those receiving sibling grafts and 60-80% of those receiving unrelated donor
grafts1,2. Chronic graft versus host disease is a multi-system disorder3 that seriously compromises
recipients’ health4,5, sometimes negating the disease-curing benefit of transplantation and
predisposing patients to secondary cancer6. Ill-health due to cGVHD is often aggravated by the sideeffects of immune suppressive treatments. In this proposal, we outline a study to test a promising
intervention that we hypothesize will prevent in some patients, and ameliorate in others, the
suffering caused by cGVHD.
In standard HPCT recipients receive a preparative regimen of chemotherapy, with or without
radiation. Unfit or older recipients receive milder regimens, non-myeloablative rather than
myeloablative. Immune suppressive drugs are given to prevent rejection and GVHD. The donor’s
progenitor cell graft is then obtained either from the bone marrow, or by pheresis after the donor
receives filgrastim. Progenitor cells are given by intravenous infusion and engraftment is revealed by
rising blood cell counts two to three weeks later. Minor histocompatibility antigen differences
between donor and recipient result in a donor immune attack on the recipient’s normal tissues
(GVHD) and on the diseased tissues (graft versus leukemia reaction, GVL). The latter contributes to
cure of the marrow disorder. Acute graft versus host disease (aGVHD) is a common, and sometimes
fatal, complication in the first 100 days and consists of inflammation of the skin, liver and
gastrointestinal tract, with immune dysfunction leading to infections. Chronic GVHD (cGVHD)
usually occurs after three months. It may be fatal or may take years to resolve and the patient may
be left debilitated. cGVHD is a multi-system disorder2 commonly causing inflammation and fibrosis
of skin, soft tissues and lungs7, mucositis and conjunctivitis. cGVHD results in fatigue, decreased
quality of life4,5, organ dysfunction, and immune dysfunction, and is strongly linked to the
development of secondary cancers6. Additional manifestations result from the side effects of
immune suppressive drugs used for its treatment. Eventually, immune tolerance develops and
immune suppressive drugs can be permanently withdrawn. However, because of the persistence of
cGVHD less than 15% of patients are able to discontinue immune suppressive therapy 1-2 years
following transplantation, and 25% remain on therapy after 4 years1,3,4. Recognition of both long
term and permanent sequelae of cGVHD has lead to the development of international practice
guidelines for long term follow up of transplant recipients8.
There has been little progress towards the prevention of cGVHD and there has been dissatisfaction
regarding its classification, but recent publications have given impetus to research by highlighting
the seriousness of the condition and providing both a provisional revised classification and
recommendations for research. Quality of life studies have described the impact of cGVHD on the
Page 19 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
lives of transplant recipients in a better way than have existing clinico-pathological classifications of
organ involvement4,5. A recent NIH-sponsored symposium critically reviewed all knowledge about
cGVHD, a new classification was formulated and recommendations for research methodology laid
out9-14. The recommendations are based on best evidence but are provisional and will need to be
validated in clinical trials, such as the one being proposed here.
The preface to the NIH series of publications15 stated: “Chronic graft-versus-host disease (cGVHD)
desperately needs fresh attention”. The commentary pointed to “the absence of standardized
criteria for diagnosis, staging and response criteria in this disorder” as being the major barrier to
progress in clinical research. Noted also was the absence of Food and Drug Administration (FDA)–
approved medications for the disorder, and that clinical research seeking to better understand
cGVHD lags behind other innovations in hematopoietic cell transplantation. The NIH symposium
provides directions and recommendations towards better research.
The present study is designed primarily to ameliorate the suffering from cGVHD. It will also
contribute to the testing and validation of the recommendations of the NIH-sponsored symposium
on cGVHD, and will be an opportunity for parallel immunological studies (in conjunction with the
CIHR-funded sub-study “BIOMARKERS IN CHRONIC GRAFT VERSUS HOST DISEASE” – Schultz, K et al.)
7.2. The Principal Research Question to be Addressed
Patients undergoing unrelated HPCT will be randomized to a standard arm (preparative regimen
without Thymoglobulin®) or experimental arm (preparative regimen with Thymoglobulin®) in order
to determine if the addition of Thymoglobulin® will result in a decrease in the proportion of patients
developing chronic graft versus host disease.
7.3. Rationale
Chronic graft versus host disease in unrelated HPCT is a serious health problem which is only
minimally ameliorated by current treatments, treatments that add to morbidity and risk of mortality.
Prednisone and cyclosporine together with second line medications have well known toxicities and
the many used attest to their low effectiveness2, 16, 17. Also attesting to their ineffectiveness is the
large number of ancillary and support measures recommended for each of the many
manifestations18. A non-drug treatment, photopheresis19, is arduous and expensive, requiring
patients to attend for three hours once to three times weekly for many months. Prevention of
chronic graft versus host disease would be a better strategy than finding more ameliorative
treatments, and evidence from a previous randomized trial20 suggests that Thymoglobulin®, an
antithymocyte globulin made in rabbits, may be effective in reducing the incidence and severity of
this complication. There is no other currently promising candidate treatment to prevent cGVHD.
Pre-transplant removal of T-lymphocytes (“T-cell depletion”) of grafts was tested in an NHLBI-funded
randomized trial; no diminution in the incidence of cGVHD was noted21. It is expected that
Thymoglobulin®, which is an in vivo method of depleting T-cells, will be more effective.
Page 20 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
7.4. Previous Studies
Bacigalupo et al. conducted two randomized trials of antithymocyte globulin (ATG, Thymoglobulin®)
given with the intention of decreasing the incidence and mortality of the acute form of graft versus
host disease (aGVHD). There was no effect on the incidence of aGVHD22 but on later follow up20
there was a marked decrease in cGVHD which was both statistically and clinically significant. There
were no adverse effects on transplant related mortality or leukemic relapse or survival. The studies
by Bacigalupo are the only randomized trials that directly study the effects of ATG and these are
therefore described in detail.
The first manuscript22 describes two successive randomized trials for the prevention of aGVHD in
which the outcomes of patients receiving ATG were compared with those not receiving ATG at doses
of 7.5 mg/kg and 15 mg/kg given with the preparative regimen. At the lower dose there was no
significant impact on the incidence of aGVHD while at the higher dose, the incidence of aGVHD was
markedly reduced (50% vs. 11%, p=0.001); however, overall survival was not improved because of a
counterbalancing increase in lethal infections (30% vs. 7%, p=0.02). The second manuscript20
described a long term (7.4 years and 5.3 years) follow up of patients on these two trials. Across both
trials, cGVHD was reduced from 62% to 39% (p=0.03) with similar trends at both dosage levels, 65%
vs. 38% (p=0.08) at the lower dose and 62% vs. 39% (p=0.04) at the higher dose. The decrease in
overall incidence of cGVHD was reflected by improvements in organ function, in the incidence of
“extensive” grade, and in patients’ performance by Karnofsky scale. Improvements in lung function
were particularly impressive. A summary is as follows:
Seventy five of the starting cohort of 109 patients, 38 who had received ATG and 37 who had not,
survived 100 days following transplantation and therefore qualified to develop cGVHD. The results
on follow up (median 5.7 years), for cGVHD, for bronchiolitis, for Karnofsky scores and survival were:
ATG
No ATG
P value
Number of participants
38
37
% cGVHD
37
60
.05
% extensive cGVHD
15
41
.01
Chronic lung dysfunction
19
51
.005
% Karnofsky ≥90%
89
57
.03
Survival (actuarial, 6yrs)
44
31
.80
Page 21 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Conclusions from studies of Bacigalupo: ATG resulted in an important reduction in the incidence of
cGVHD; however the primary endpoint was aGVHD and so the results for cGVHD can only stand as
hypothesis generating. The efficacy of Thymoglobulin® for the prevention of cGVHD needs to be
established by a prospective randomized trial with cGVHD as the primary endpoint.
A recent publication23 describes in a randomized trial positive effects on the incidence of both
aGVHD and cGVHD using Fresenius®, an alternate anti-lymphocyte globulin, prepared from
lymphoblasts rather than thymocytes as is Thymoglobulin®. The two products differ in a number of
other ways, and Fresenius is not available in North America. However, this study provides additional
support for the general approach of using an anti-lymphocyte globulin to prevent cGVHD.
Literature Search: To avoid bias in the assessment of present knowledge, a systematic literature
search of Medline was undertaken. No other randomized trials were found. Of 372 citations, just 4
were immediately relevant to this proposal and they support the findings in the randomized trial of
Bacigalupo in suggesting a decrease in the incidence of chronic graft versus host disease without
adverse effects on rates of leukemic relapse and infections.
7.5. Conclusions
A positive result in this study on the background of previous studies would provide strong impetus
toward wide-spread adoption of Thymoglobulin® into the transplant preparative regimen of patients
receiving unrelated donor grafts, potentially for all such transplants, both myeloablative and nonmyeloablative, and in both children and adults. Such a recommendation would depend on the
transplant community’s appraisal but would be supported by the results of the previous study by
Bacigalupo20, by its present status in Europe of being licensed for the prevention of GVHD, and by
the very recent report23 of similar results using a different preparation of antilymphocyte globulin
(Fresenius). The inclusion of Thymoglobulin® would be additive to existing preparative regimens
with no disruption to schedules, and with no adverse pharmacological interactions. Further, this
agent is familiar to hematologists being presently used for the treatment of aplastic anemia.
7.6. Safety Considerations
The main risks to participants are those of the transplant procedure, the decision to proceed being
completely independent of the decision to volunteer for the study. The risks of participating in
the study are those related to the intervention, the administration of Thymoglobulin®, an
antiserum prepared in rabbits. Most patients experience some symptoms during the first
infusion, which are in almost all cases easily controlled by brief administrations of steroids,
acetaminophen and diphenhydramine. Only rarely will patients have severe reactions resulting in
discontinuation. Thymoglobulin® is an immunosuppressive agent, so a risk of serious infection
Page 22 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
needs to be stated. A high risk of infection appears to be related to doses higher than will be used
in this study. In randomized studies by Bacigalupo the serious infections experienced with high
doses were not replicated with the use of low doses, being no higher than controls22. In our study
the dose of Thymoglobulin® will be even lower. Other studies support the conclusion that the risk
of serious infection is low with currently used doses, possibly even lower than controls because of
a decrease in GVHD and hence a decrease in immune deficiency24-26. An increased rate of relapse
of leukemia has been reported in related donor transplants24,25 but without an increase in overall
mortality; there was no increased risk of relapse in two randomized trials using unrelated
donors22,27. Post transplant lymphoproliferative disorder (PTLD) has been an occasional
complication of Thymoglobulin®, a phenomenon related to reactivation of EBV infection, itself a
common occurrence following transplantation. Risk factors for the development of PTLD after
transplantation include EBV seropositivity, T-cell depletion, administration of ATG, and posttransplant EBV activation28-30. Among randomized trials, PTLD occurrence was not reported in the
trial of Bacigalupo while in the trial of Finke [modified from original: there were six cases, five in
the ATG arm, two of whom died, and one in the control arm23, 31. Prevention of PTLD involves
monitoring for activation by QPCR and pre-emptive administration of rituximab at the first sign of
significant reactivation32. Risks of infection, leukemic relapse and PTLD all need to be stated in the
consent form but the level of risk for each appears to be low.
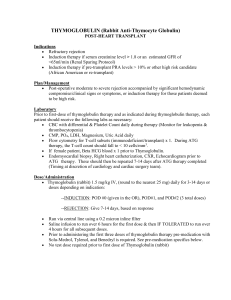
7.7. Thymoglobulin®
The following text has been extracted selectively but verbatim from the Thymoglobulin® Product
Monograph and the Investigators Brochure. More detailed information is available in these
documents which can be made available.
Background
Thymoglobulin® (Anti-thymocyte globulin [rabbit]) is a purified, pasteurized, gamma immune globulin
obtained by immunization of rabbits with human thymocytes. Thymoglobulin® contains a mixture
primarily of antibodies to T cell antigens, but it is largely unknown which specificities mediate the
alteration in immunoregulation.
Pharmacokinetics
Page 23 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
The initial half life has been found to be approximately 10 days and the terminal half-life approximately
30 days. Active Thymoglobulin® (that fraction which can bind to lymphocytes) has a similar initial half
life but has a much shorter terminal half life than total or inactive Thymoglobulin®
Regulatory status
In Canada, Thymoglobulin® is labeled as indicated for use in patients having renal transplantation.
Thymoglobulin® is not labeled for use in patients undergoing blood and marrow transplantation, but
Health Canada has given approval for its use for patients in this protocol. In some countries it is
approved for use in various indications including prevention and treatment of rejection in solid organ
transplants, prevention and treatment of graft-versus-host disease (GvHD) in HPCT, and treatment of
aplastic anemia (AA).
Mode of action
The in vitro mechanism of action by which polyclonal anti-lymphocyte preparations suppress immune
responses is not fully understood. Thymoglobulin® (Anti-thymocyte Globulin [Rabbit]) includes
antibodies against T cell markers such as CD2, CD3, CD4, CD8, CD11a, CD18, CD 44, CD45, HLA-DR, HLA
Class I heavy chains, and ß2 microglobulin. In vitro Thymoglobulin® (concentrations > 0.1 mg/mL)
mediates T cell suppressive effects via inhibition of proliferative responses to several mitogens. In
patients, T cell depletion is usually observed within a day from initiating Thymoglobulin® therapy.
Thymoglobulin® has not been shown to be effective for treating antibody (humoral) mediated
rejections.
The in vivo mechanism of action of Thymoglobulin®, is also not fully understood. The possible
mechanisms by which Thymoglobulin® may induce immunosuppression in vivo include T cell clearance
from the circulation, modulation of T cell activation, homing and cytotoxic activities, and T cell
depletion. The latter may occur through a number of mechanisms including complement-dependent
lysis in the intravascular space or the opsonization and subsequent phagocytosis by macrophages.
Monitoring Thymoglobulin® therapy reveals that T cell depletion in peripheral blood persists for several
days to several weeks following cessation of Thymoglobulin® therapy.
Contraindications
Thymoglobulin® is contraindicated in patients with hypersensitivity to rabbit proteins or to any product
excipients, or in those with active acute or chronic infections, which would contraindicate any additional
immunosuppression. In this protocol, “active infection” is included under Exclusion Criteria.
Serious warnings and precautions
Page 24 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Thymoglobulin® (Anti-thymocyte Globulin [Rabbit]) should only be used by physicians
experienced in immunosuppressive therapy for the treatment of renal transplant patients.
Premedication with antipyretics, corticosteroids, and/or antihistamines may decrease both the
incidence and severity of these (acute infusion-associated reactions, IARs) adverse reactions.
In rare instances, serious immune-mediated reactions have been reported with the use of
Thymoglobulin® and consist of anaphylaxis or severe cytokine release syndrome (CRS). Very
rarely, fatal anaphylaxis has been reported.
Emergency measures to treat anaphylaxis should be immediately available.
Thymoglobulin® should be used under strict medical supervision in a hospital setting, and
patients should be carefully monitored during the infusions.
Rapid infusion rates have been associated with case reports consistent with CRS. In rare
instances, severe CRS can be fatal.
Skin testing is not advised prior to Thymoglobulin® administration.
Adverse Reactions
The most frequent reported adverse events (more than 25% of patients) include: fever, chills,
leukopenia, pain, headache, abdominal pain, diarrhea, hypertension, nausea, thrombocytopenia,
peripheral edema, dyspnea, asthenia, hyperkalemia, tachycardia, and infection.
Infections (bacterial, fungal, viral, and protozoal), reactivation of infection (particularly cytomegalovirus
[CMV]), and sepsis have been reported after Thymoglobulin® administration
Use of immunosuppressive agents, including Thymoglobulin® , may increase the incidence of
malignancies, including lymphoma or post-transplant lymphoproliferative disease (PTLD)
8. Eligibility and Study Entry
Only recipients are screened. Donors are not for the purposes of this study; they are screened to
meet the requirements of medical care, institutional guidelines and applicable government
regulations. There are no study interventions that impact donors. The choice of the donor also is
outside the procedures of this study. Recipients will be screened for study eligibility prior to the
start of conditioning. Inclusion and Exclusion criteria must be met as outlined in Sections 8.1 and
8.2 before the recipient can be randomized. (Randomization should be done no earlier than 21
calendar days before the planned date of transplant and no later than 1 day prior to the start of
the preparative regimen.)
Page 25 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
8.1. Inclusion Criteria
1. The participant is aged between 16 and 70
2. The participant has an hematologic malignancy i.e. one of:
Acute leukemia, myeloid, lymphoid, or biphenotypic, in 1st or 2nd remission or be in early
relapse (no chemotherapy within three months and blasts <10% and with previous
remission having been longer than 3 months)
Chronic myeloid leukemia, in chronic or stable accelerated phase
Chronic lymphocytic leukemia
Lymphoma
Myelodysplastic syndrome
Myeloproliferative disorder
3. The participant will receive one of the specified preparative regimens (section 8.3.)
4. The participant will receive either a bone marrow (“HPC, Marrow”) or blood progenitor cell
(“HPC, Apheresis”) graft
5. The participant has an unrelated donor who with high resolution or intermediate resolution
typing is either fully MHC matched at HLA-A, B, C and DRB1 with the recipient or is 1-antigen
or 1–allele mismatched at A, B, C or DRB1 loci
6. The participant meets the transplant centre’s criteria for unrelated donor allogeneic
transplantation2, either myeloablative or non-myeloablative (syn. RIC).
7. The participant has good performance status (Karnofsky ≥60%)
8. The participant is able to understand and sign the informed consent form
9. For the questionnaire component only, be able to complete the questionnaires in English or
with a validated translation (as posted on the project website)
Regarding disease classification:
If a centre is unsure about eligibility contact the Project Manager or Clinical Study Chair.
8.2. Exclusion Criteria
1. The participant is HIV antibody positive
2
Centres must provide their standard criteria for transplantation and their standard operating
procedures (SOP) regarding the decision-making process. This documentation must be submitted to
the Project Management Office and filed in the site trial files. A copy of this source documentation
must be accessible for monitoring and auditing purposes. Applicable source documentation must be
available at the site for monitor verification.
Page 26 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
2. The participant has a hypersensitivity to rabbit proteins or Thymoglobulin® pharmaceutical
excipients, glycine or mannitol
3. The participant has active or chronic infection (i.e. infection requiring oral or IV therapy)
4. The participant (if female and of childbearing potential) is pregnant or breast-feeding at the
time of enrollment
5. The participant (if female and of childbearing potential) does not agree to use an adequate
contraceptive method from the time of enrollment until a minimum of one year following
transplant3
6. The participant (if male and fertile) does not agree to use an adequate contraceptive method
from the time of enrollment until a minimum of one year following transplant
7. For the questionnaire component only, the participant is unable to participate due to
cognitive, linguistic or emotional difficulties (i.e. the participant can participate in the main
study but will be excluded from the questionnaire component
8. The participant is unable to understand the informed consent form.
8.3. Preparative Regimens
The participant must receive one of the following preparative regimens4:
8.3.1. Myeloablative Preparative Regimens:
Cyclophosphamide and Total Body Irradiation (CY-TBI)-based regimens that include at least
120 mg/kg cyclophosphamide intravenously and at least 1200 cGy of fractionated TBI.
Busulfan and cyclophosphamide (BU-CY)-based regimens that include at least 14 mg/kg
busulfan orally or 11.2 mg/kg busulfan intravenously (14 x 0.8 correction factor) or a
targeted busulfan dosing strategy aimed at a serum concentration greater than 600 ng/mL
at steady state and at least 120 mg/kg cyclophosphamide intravenously.
Fludarabine and busulfan-based regimens that include a fludarabine dose of at least 120
mg/m2, at least 8 mg/kg busulfan orally or 250 mg/m2 busulfan intravenously. Institutional
standards should be followed for targeting plasma levels.
Other myeloablative regimen(s) approved by the Study Chair.
Regimens containing ATG or alemtuzumab are not permitted.
3
Adequate methods of birth control include: Abstinence, previous tubal ligation, vasectomy, oral
injectable or implantable contraceptives, condoms, foam, or IUD.
4
Centres must provide their protocols for transplant regimens and the indications for each regimen they
intend to use for patients enrolled in the CBMTG 0801 trial. Regimens for GVHD prophylaxis must also
be submitted to the Project Management Office.
Page 27 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
8.3.2. Non-myeloablative (RIC)5
References given are those of the original author; a number of variations have since been
described:
Fludarabine and busulfan-based33
Fludarabine and TBI34
Fludarabine and melphalan35
Other non-myeloablative regimen(s) approved by the Study Chair.
Regimens containing ATG or alemtuzumab are not permitted.
Note: A suggested definition of non-myeloablative (or RIC) is busulfan ≤8 mg/kg; melphalan
≤140 mg/m2; TBI ≤500cGy single dose or ≤800cGy fractionated36.
8.4. Donor Selection
The donor must be either fully MHC matched at HLA-A, B, C, and DRB1 loci or 1-antigen or 1–allele
mismatched at either HLA-A, B, C or DRB1 loci (i.e. either a 7/8 or 8/8 match, considering only HLAA, -B, -C and DRB1).
Donors will be evaluated according to one or both of FACT Standard and Health Canada regulations,
or other national regulations. Donor choice is according to these regulations and standard
institutional practice.
The donor-related risk factors for chronic graft versus host disease that have been most consistently
found are HLA mismatch, multiparity of female donors and donor age.
8.5. Informed Consent
The participant and/or the participant’s legally authorized guardian must acknowledge in writing
that consent to become a study participant has been obtained.
Participants 16-18 Years of Age
Sites should follow the requirements of their local IRB with respect to the consent process for
participants aged 16-18. A copy of a consent template for participants aged 16-18 (which includes a
page of assent) has been included in Appendix 1 for sites. The use of this template is optional
depending on the requirements of the local IRB. A “Note-To-File” should be drafted that clearly
5
The term “non-myeloablative” is synonymous to “Reduced Intensity Conditioning”
Page 28 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
explains the site’s procedure with respect to the consent of participants aged 16-18. This “Note-ToFile” should be filed in the IRB section of the site regulatory files.
Delayed Transplant
If a transplant is delayed more than 2 months, consent must be obtained again in writing (using the
current IRB approved consent form).
8.6. Protocol Approval
This protocol must be reviewed and approved by the institutional review board (Institutional Review
Board – IRB, or Research Ethics Board – REB) at each participating transplant centre prior to
approaching potential participants.
8.7. Registration and Minimization (Randomization)
A “Registration and Randomization” form (Appendix 4) is submitted to the Project Management
Office once a participant has given informed consent AND all eligibility criteria have been met. The
form will be reviewed by the Project Manager (or delegate). If all criteria are met, then the
minimization (randomization) will be completed, and the site will be informed of the study arm
assigned by email and/or fax. Once this occurs, the participant will be considered enrolled in the
trial.
Randomization must be done no earlier than 21 calendar days before the planned date of transplant
and no later than 1 day prior to the start of conditioning. The Study Chair may allow randomization
to be done prior to 21 calendar days before the planned date of transplant, but the site must submit
a written request to the Project Management Office, and the early randomization must be approved
in writing by the Study Chair.
8.7.1. Participants Who Become Ineligible Following Randomization
It may occur that a participant’s status changes unexpectedly following randomization, such
that they no longer meet one or more of the inclusion and exclusion criteria. When this
occurs, the course of action is at the clinical discretion of the site transplant team. The site
may choose to: (1) Delay transplant until all criteria are met (see Section 8.7.1.1.); (2) Cancel
the transplant altogether (see Section 8.7.1.2.); or (3) Proceed with the transplant even
though the patient does not meet the study inclusion and exclusion criteria for the study
(See Section 8.7.1.3.). Sites should always keep in mind that it is best to randomize a
participant as close to the start of the preparative regimen as possible so that this
situation can be avoided.
Page 29 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
As the study progresses, the study steering committee and DSMC will carefully monitor the
percentage of participants who are randomized, but then become ineligible. (Participants
who become ineligible will not be replaced.)
8.7.1.1. Delayed Transplant
If a scheduled transplant is postponed following randomization, the participant can
remain on study as long as the inclusion and exclusion criteria are met within 21
calendar days before the rescheduled transplant date. A “Confirmation of
Eligibility” form (Appendix 4) should be submitted prior to the start of the
preparative regimen and no sooner than 21 days before the rescheduled transplant
date. Please see section 8.5 for requirements regarding participant consent in this
situation.
8.7.1.2. Cancelled Transplant
In this case, the participant is no longer eligible; however, because the study design
is “intention to treat”, the participant’s survival status will be followed for up to
two years from the date of randomization.
8.7.1.3. Transplant Proceeds (Inclusion/Exclusion Criteria Not Met)
In this case, participants randomized to receive Thymoglobulin® should NOT
receive the study drug (Thymoglobulin®). A change in eligibility status may mean
there is greater risk involved with receiving Thymoglobulin®. An experimental drug
or procedure should not be administered unless all eligibility criteria are met.
Regardless of what arm the participant has been assigned to, all study related
laboratory procedures should still be followed as per protocol. All study data
should be collected as per protocol. All questionnaires should be administered
according to the schedule specified in the protocol. All assessments for GVHD
should be completed according to the protocol.
9. Treatment Plan
The recipient will be randomized (minimized) to one of two study arms:
Arm A (Standard ): Participants will receive a standard HPCT preparative regimen (either
myeloablative or RIC) as outlined in Section 9.3.
Page 30 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Arm B (Experimental): Participants will receive a standard HPCT preparative regimen PLUS
Thymoglobulin® on day -2,-1 and Day +139,79 .
This is not a blinded study. Participants randomized to Arm A (standard arm) will NOT receive a placebo.
9.1. Overview
Preparative Regimen
(Arms A and B)
Thymoglobulin
(Arm B only)
Day Day Day Day
Day
Day
Day
–7
–6
–5
–4
–3
–2
–1
Myeloablative or non-myeloablative (syn.RIC*)
conditioning regimen†
®
0.5
mg/kg
Day
0¤
Day
+1
Graft
Infusion
2.0
mg/kg
2.0
mg/kg
* No distinction between “non-myeloablative” and “RIC” (Reduced Intensity Conditioning)
†See section 9.3
¤ Radiation may be given on day 0
9.2. Source of Progenitor Cells
For all patients this will be either bone marrow or blood. The choice will be determined by the
centre and by availability. Neither T-cell depletion of the graft nor the use of cord blood is
permitted.
9.3. Preparative Regimens
Recipients must receive one of the following preparative regimens6:
9.3.1. Myeloablative Preparative Regimens
6
Cyclophosphamide and Total Body Irradiation (CY-TBI)-based regimens that include at least
120 mg/kg cyclophosphamide intravenously and at least 1200 cGy of fractionated TBI.
Busulfan and cyclophosphamide (BU-CY)-based regimens that include at least 14 mg/kg
busulfan orally or 11.2 mg/kg busulfan intravenously (14 x 0.8 correction factor) or a
targeted busulfan dosing strategy aimed at a serum concentration greater than 600 ng/mL
at steady state and at least 120 mg/kg cyclophosphamide intravenously.
Centres must provide their protocols for transplant regimens and the indications for each.
Page 31 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Fludarabine and busulfan-based regimens that include a fludarabine dose of at least 120
mg/m2, at least 8 mg/kg busulfan orally or 250 mg/m2 busulfan intravenously. Institutional
standards should be followed for targeting plasma levels.
Other myeloablative preparative regimen(s) approved by the Study Chair.
Regimens must not contain anti-thymocyte globulin (ATG), anti-CD52 or other anti-T cell
antibody, rituximab, pentostatin, mesenchymal stem cells, or TNF inhibitors.
9.3.2. Non-myeloablative (RIC) Preparative Regimens
Non-myeloablative conditioning is sometimes referred to as reduced intensity conditioning
(RIC); no distinction will be made between these two terms. Many non-myeloablative regimens
have been described, and subsequent investigators have often used doses that vary from the
original descriptions. Banna37 has written an informative review, outlining dose ranges that
have been described in publications. In this trial, investigators have the option of adopting one
of the three most commonly used regimens outlined below. As stated previously, centres must
provide their protocols for transplant regimens and the indications for each. Centres are not
required to adhere to specific doses but should adhere to the criteria for “non-ablative” (or RIC)
suggested by CIBMTR (see footnote below7). Early references to the allowed regimens are as
follows, but Banna37 et al (see below) can be consulted for published variations:
References given are those of the original author; a number of variations have since been
described:
Fludarabine and busulfan-based33
Fludarabine and TBI34
Fludarabine and melphalan35
Other RIC regimen(s) approved by the Study Chair
Regimens must not contain anti-thymocyte globulin (ATG), anti-CD52 or other anti-T cell
antibody, rituximab, pentostatin, mesenchymal stem cells, or TNF inhibitors.
Note: A suggested definition of non-myeloablative (or RIC) is busulfan ≤8 mg/kg; melphalan
≤140 mg/m2; TBI ≤500cGy single dose or ≤800cGy fractionated36.
9.4. Administration of Thymoglobulin® (ARM B ONLY)
Thymoglobulin® will be administered on days -2, -1 and +139,79. A steroid-containing pre-medication
protocol should be followed (Appendix 5). Day “0” is the date that the progenitor cell infusion is
completed. In almost all cases it will be the same day that the infusion is commenced, but if the
7
Busulfan ≤8 mg/kg; melphalan ≤140 mg/m2; TBI ≤500cGy single dose or ≤800cGy fractionated.36 Giralt et al.
BBMT 2009;15:367
Page 32 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
infusion commences late on one day (eg, Friday) and is completed after midnight, then day 0 will be
Saturday. The date of the “Day +1” dose of Thymoglobulin should be adjusted as necessary,
depending on the actual date the progenitor cells infusion is completed. (In some cases the infusion
occurs later than planned.) The last dose of Thymoglobulin® should be commenced within 24 hours
of the completion of the progenitor cell infusion.
The total dose of Thymoglobulin® is 4.5 mg/kg (actual body weight, not effective body weight), given
in divided doses as follows:
Day -2: 0.5 mg/kg
Day -1: 2.0 mg/kg
Day +1: 2.0 mg/kg
Dr. James Russell has generously provided a set of suggested orders (Appendix 5).
Important:
Although Thymoglobulin® and progenitor cells are compatible, they should not be
infused at the same time, for reasons of determining the cause of reactions.
Progenitor cells should be infused as soon as possible after arrival from the donor
centre as delays can affect the outcome, particularly with respect to progenitor cells
obtained from the marrow.
9.5. Graft versus Host Disease Prophylaxis
Cyclosporine or tacrolimus, together with methotrexate or mycophenolate will be used in
conjunction with either myeloablative or non-myeloablative regimens. Participating transplant
centers must submit their standard regimens for GVHD prophylaxis to the Project Management
Office for review. See section 9.5.1. for requirements regarding methotrexate administration. See
section 9.5.3. for requirements regarding cyclosporine administration.
9.5.1. Methotrexate
Methotrexate is to be administered according to institutional practices. The first dose should be
administered at least 24 hours after the infusion of the progenitor cell graft. Doses should be
reduced for hepatic and renal dysfunction, mucositis and for significant fluid collections (ascites,
pleural effusions). The use of folinic acid rescue will be according to institutional practice.
Suggested Dose Reduction for Methotrexate Toxicity
Page 33 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Methotrexate dose adjustments for toxicity will be according to institutional practice; however,
the following adjustments for renal dysfunction, hepatic dysfunction and pleural effusions are
recommended.
Note: The reductions in methotrexate dose, based on direct bilirubin, calculated creatinine
clearance, mucositis and fluid collections, are additive.
Reduction of Methotrexate Dose for Hepatic Dysfunction
Direct Bilirubin
(micromoles/litre)
Direct Bilirubin
(mg/dl)
Percent Reduction of
Methotrexate Dose
0-34
35-50
51-100
Greater than 100
0- 2.0
2.0 -2.9
3.0-5.8
Greater than 5.8
0
25
50
100
Suggested Reduction of Methotrexate Dose for Renal Dysfunction
Calculated Creatinine
Clearance (mL/min)1
Greater than 85
65-84
50-64
0-49
Percent Reduction of
Methotrexate Dose
0
25
50
100
1
For males, calculated creatinine clearance = [(140 age in years) x (Ideal Body Weight) x
60]/[serum creatinine x 50]. For females, multiply the calculated creatinine clearance for males
by 0.85.
Suggested Reduction of Methotrexate Dose for Mucositis
It is recommended that sites grade mucositis according to the Bearman criteria on Days +1, +3,
+6 and +11. It is recommended that the dose of methotrexate will be reduced for mucositis as
indicated in the table below. (See Appendix 6 for Bearman Scale).
Bearman Stomatitis
(Mucositis) Grade
Percent Reduction of
Methotrexate Dose
Grade 0, Grade 1, Mild Grade 2
0%
Page 34 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Moderate Grade 2
25%
Severe Grade 2, Grade 3
100%
Suggested Reduction of Methotrexate Dose for Fluid Collections
If the patient has a clinically significant pleural effusion or ascites, it should be drained if this is
feasible. If the clinically significant fluid collection cannot be drained, it is strongly
recommended that the dose of methotrexate be held.
Note: The reductions in methotrexate dose, based on direct bilirubin, calculated creatinine
clearance, mucositis and fluid collections, are additive.
9.5.2. Mycophenolic Acid
Where mycophenolic acid is used as part of prophylaxis against GVHD, it will be administered
according to the protocol submitted by the transplant centre.
9.5.3. Cyclosporine and Tacrolimus
Cyclosporine or tacrolimus will be administered orally or intravenously according to standard
practice at the site. The standard regimen must be approved by the Study Chair. The starting
dose will be according to institutional practice. After initiation of cyclosporine or tacrolimus,
the dose will be adjusted to maintain adequate trough levels according to standard institutional
practice.
Tapering of cyclosporine (or tacrolimus) in the absence of significant acute GHVD will be
according to institutional practice. In each institution it is essential that the same tapering
schedule be followed for patients on both arms of the study. If a participant develops acute
graft versus host disease prior to or during the tapering of cyclosporine or tacrolimus, further
adjustments of the dose and decisions about the initiation and speed of tapering will be
according to institutional practice.
9.6. Co-Enrollment in Other Clinical Trials
Co-enrollment in other clinical trials will be considered on a trial by trial basis. The protocol must be
reviewed by the Study Steering Committee and receive approval of the committee before coenrollment can occur. The sponsor of the other protocol must also approve co-enrollment. The
Project Manager will maintain a list of approved protocols. A copy of each approved protocol will be
kept in the trial files at the Project Management Office.
Page 35 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
9.7. Graft versus Host Disease Diagnosis
Acute Graft versus host disease will be diagnosed and graded according to Przepiorka et al40
(Appendix 7). Chronic Graft Versus Host Disease will be diagnosed and staged according to both
Sullivan criteria41 (Appendix 8) and NIH criteria10 (one “diagnostic” manifestation or one “typical”
manifestation plus other supportive evidence).
Sites will be asked to determine the NIH grade of chronic GVHD; however, a member of the study
steering committee (or delegate) will determine the Sullivan grade using the data entered in the
Appendix 9 form.
9.8. Acute Graft versus Host Disease Treatment
Grades 2-4 acute GVHD, which requires treatment, will be treated with corticosteroids, either
intravenous methylprednisolone 1-2 mg/kg/day or oral prednisone 1-2.5 mg/kg/day in single or
divided daily doses. The initial treatment with corticosteroids should be administered for at least 5
days. After 5 days, tapering of the corticosteroid can be initiated if the patient’s acute GVHD is
improving, according to local institutional practice.
If tapering of cyclosporine or tacrolimus has begun by the time of onset of Grades 2-4 acute GVHD
requiring treatment, the dose of cyclosporine or tacrolimus will be increased to re-establish a
therapeutic cyclosporine level (whole blood trough cyclosporin level of 200-400 micromoles/L).
Tapering of cyclosporine may recommence if acute GVHD improves.
If the acute GVHD does not respond or progresses during the initial treatment with corticosteroids,
the dose of corticosteroids may be increased and/or additional agents may be used according to
local institutional practice. All treatments for acute GVHD will be recorded.
9.9. Chronic Graft versus Host Disease Treatment
Chronic GVHD which requires systemic treatment, will initially be treated according to institutional
practice. Biopsy of involved organs or tissues is strongly recommended but not required. (It is
recommended that chronic GVHD that requires systemic treatment should be initially treated with
prednisone (0.5-2mg/kg PO daily in single or divided doses).
If cyclosporine or tacrolimus had been tapered or discontinued, it may be restarted either at the
same time as prednisone is started or as second line therapy, according to the clinician’s judgement.
If the chronic GVHD does not improve with initial therapy consisting of prednisone with or without
cyclosporine or tacrolimus, the dose of corticosteroids may be increased or additional agents may
be used according to local institutional practice.
NOTE:
Page 36 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
If the onset of cGVHD requires the initiation or continuation of immune-suppression beyond routine
institutional practice, it is strongly recommended that attempts be made to taper
immunosuppressive therapy between days 180 and 365 and the reason for failure be recorded.
All therapies and dosages for chronic GVHD will need to be recorded at 12 months as an important
secondary end-point is the dosage of immunosuppressive drugs at 12 months.
9.10 Supportive Care
9.10.1. Veno-occlusive Disease Prophylaxis
The use of agents for veno-occlusive disease prophylaxis will be according to local institutional
practice.
9.10.2. Antibacterial Prophylaxis During the Neutropenic Period
Prophylactic antibiotics, if used, will be administered according to local institutional practice.
9.10.3. Herpes Simplex Virus (HSV) Prophylaxis
HSV prophylaxis will be according to local institutional practice.
9.10.4. Antifungal Prophylaxis
Antifungal prophylaxis will be according to local institutional practice. Antifungal prophylaxis
(e.g. fluconazole 400 mg po/IV qd) is recommended when corticosteroids (equivalent of
prednisone 1 mg/kg/day or greater) are used to treat graft versus host disease.
9.10.5. Management of Cytomegalovirus (CMV)
Neither ganciclovir nor foscarnet will be used for primary prophylaxis. The general approach to
the prevention of CMV disease will be based on monitoring followed by pre-emptive treatment
of CMV infection (viremia). Monitoring for CMV infection in recipients at risk (recipient or
donor is positive for CMV antibody) will be by CMV antigenemia or QPCR. The frequency and
duration of CMV monitoring will be according to local institutional practice. Treatment of CMV
infection or CMV disease, with either ganciclovir or foscarnet, will be initiated according to local
institutional practice.
9.10.6. Management of Epstein Barr Virus (EBV)
Activation of latent EBV is common after HPCT28, occurring in one-third of those receiving Treplete grafts and two-thirds of T-cell depleted grafts, but rarely results in clinical consequences.
Occasionally, activation of EBV leads to the development of the serious complication of Post
Transplant Lymphoproliferative Disorder (PTLD, LPD). In the study by Finke23 there were five
cases among 103 participants randomized to (Fresenius®) and one case among 98 controls.
Anti-lymphocyte globulin was thus shown to be an important risk factor. The latest and most
Page 37 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
authoritative sources of information and recommendations can be found in two recent
publications.42, 43 These authorities are recommending screening of at-risk populations.
Screening
For study purposes we recommend routine screening for EBV activation in all enrolled
participants, by PCR or, preferably, by QPCR, according to local resources, weekly from day 0 to
day 100, then thereafter only in selected cases depending on the degree of immunosuppression,
the severity of graft versus host disease, and existing low level activation. At a minimum,
screening is strongly recommended in patients receiving Thymoglobulin®, in accordance with
current recommendations.42, 43 If sites have already established a standard approach to EBV
monitoring that is different from this recommended approach, the site will be permitted to
continue to follow their standard approach; However, a copy of the standard approach must be
submitted to the Study Chair for review. A copy will be kept in the Sponsor study files and site
files.
Indications for Treatment
As there are no laboratory or standards published, and because methodologies, reported units
(eg G Eq/mL vs copies/mL) and probably sensitivities, vary, threshold levels at which treatment
should be initiated cannot be stated. Physicians are advised to take into account knowledge
about local methodology. (The local laboratory director and sold organ transplant physicians
should be consulted.) The reported level, rising titres, and/or clinical features; biopsy of
enlarged lymph node should be considered where feasible when making a decision regarding
treatment. It is strongly recommended that plasma or serum based assays utilized should allow
for the reporting of 1,000 copies/mL at a minimum.
Treatment
Treatment of activation will be either pre-emptive or therapeutic depending on the clinical
situation. The recommended treatment is rituximab 375 mg/m2, to be repeated weekly as
necessary till resolution, clinically and by PCR.
Important
Although recommendations regarding testing and treatment have been included in the
protocol, decisions regarding whether or not to monitor post transplant, type of assay,
frequency of monitoring , when to treat and how to treat are at the discretion of the site
investigator(s).
Reporting
Cases of both significant EBV reactivation (ie requiring treatment) and PTLD are to be reported.
Page 38 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
9.10.7. Pneumocystitis Carinii Prophylaxis
All participants are to receive pneumocystitis carinii prophylaxis. This will be according to
institutional practice.
9.10.8. Blood Product Support
Irradiated red blood cell and platelet transfusions will be used. Transfusion thresholds will be
according to local institutional practice.
9.10.9. Administration of Growth Factors Following Graft Infusion
Neutrophil recovery is a secondary study endpoint and growth factors such as filgrastim should
not be routinely used following the infusion of bone marrow or peripheral blood. However, if a
participant develops primary engraftment failure (absolute neutrophil count of less than 0.5 x
109/L on Day +28), filgrastim may be administered and an additional infusion of donor cells with
or without additional conditioning. Filgrastim may be used at any time in a participant’s course
if considered necessary by the attending physician. This is to be recorded in the data collection
forms.
9.10.10. Prophylactic Intravenous Gammaglobulin
It is recommended that prophylactic intravenous gammaglobulin not be routinely administered
post-transplantation. There may be special cases, such as CLL patients already on
gammaglobulin prior to transplant, in whom it might be justified. As immunoglobulin levels are
to be recorded in the follow-up period, administration of gammaglobulin needs to be reported
in the data collection forms.
9.10.11. Maintenance Therapy with TKI Inhibitors
The use of maintenance therapy post transplant with imatinib or other TKI inhibitors is
permitted according to institutional practice.
10.
Required Observations and Information
10.1. Pre-Transplant Clinical Evaluations
The observations listed in this section may or may not be part of the standard pre-transplant
evaluation at the site; however, ALL observations listed in this section must be made according to
the time points specified below for participants enrolled in CBMTG 0801. Source documentation
for all observations should be available at the site for monitoring and auditing purposes.
The following observations should be made within 60 days prior to the start of the preparative
regimen (except as noted otherwise):
Page 39 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
10.1.1.
10.1.2.
10.1.3.
10.1.4.
History and physical exam
Height and weight
Karnofsky performance status
Co-Morbidity Index (Appendix 10). Complete this form then enter the score in
the Data Collection Forms.
10.1.5. CBC, differential, creatinine, total bilirubin, AST, ALT, ALP, blood group and
antibody screen
10.1.6. Infectious Disease Markers: CMV antibody, Hepatitis B surface antigen, total
antibody to Hepatitis B core antigen, Hepatitis C antibody, HIV-1 and HIV-2
antibodies, HTLV-1 and HTLV-2 antibodies and VDRL or equivalent testing for
syphilis; West Nile virus testing (according to local institutional practice); EB virus
antibodies (VCA-IgG and Epstein Barr nuclear antigen (EBNA)); testing for HSV
antibody is optional. Testing for infectious disease markers must be done within
30 days prior to transplant
10.1.7. Cardiac evaluation with assessment of ejection fraction by radionucleotide scan
or echocardiogram
10.1.8. Pulmonary evaluation with spirometry (FEV1) and diffusing capacity (DLCO) or
equivalent method approved by Study Chair
10.1.9. Renal evaluation with 24 hour urine for measured creatinine clearance or serum
calculated GFR
10.1.10. Beta-HCG in female participants of child bearing potential (within 30 days prior
to transplant
10.1.11. Bone marrow aspirate and biopsy (within 30 days prior transplant); cytogenetic
analysis is strongly recommended for recipients with myeloid malignancies
10.2. Pre-Transplant Questionnaires
The following questionnaires must be completed after consent but prior to the start of the
conditioning regimen:
Bradburn Scale44; CES-D Scale45, Illness Intrusiveness Ratings Scale46, Screening FACT-BMT47, EQ-5D
Questionnaire48, Socio-demographic Questionnaire and Societal Cost Questionnaire. These
questionnaires are described in more detail in section 11.2.16.
10.3. Hematopoietic Progenitor Cell Product Information
10.3.1. Peripheral Blood Progenitor Cell Product
10.3.1.1.
10.3.1.2.
10.3.1.3.
10.3.1.4.
10.3.1.5.
Number of apheresis procedures
Volume of blood processed during each apheresis procedure
Total volume of product
Total nucleated cell count of product
CD34+ cell count of collection
Page 40 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
10.3.2. Bone Marrow Product
10.3.2.1. Total volume of product
10.3.2.2. Total nucleated cell count of product
10.4. Post-Transplant Clinical Evaluations
The following items must be carried out and/or documented:
10.4.1.
10.4.2.
10.4.3.
CBC and differential and platelet count: according to institutional practice
Lymphocyte count at Day +25, 50, 75 and 100
Absolute CD4 and CD8 T cells counts at 100 days, 6 and 12 months (if
available)
10.4.4. IgG, IgA and IgM at 100 days, 6 and 12 months
10.4.5. Absolute eosinophil count at 100 days, 6 and 12 months
10.4.6. Lymphoid and myeloid chimerism at Day + 30 and Day + 60 and Day + 100 and
Month 6 (recipients of RIC HPCT only) as institutional resources permit.
(Combined chimerism acceptable.)
10.4.7. Direct bilirubin and serum creatinine on Days +1, +3, +6 and +11 (Participants
receiving methotrexate only, unless clinically indicated for other reasons)
10.4.8. Assessment of mucositis according to the Bearman Toxicity Scale (Appendix 6)
(Participants receiving methotrexate only) on Days +1, +3, +6, +11
10.4.9. Acute GVHD: Participants will be assessed daily while in hospital and then
according to local institutional practice for the presence and severity of acute
GVHD
10.4.10. The highest grade of acute GVHD from Day +0 to Day +100 according to the
Przepiorka Criteria (Appendix 7)
10.4.11. The grade of acute GVHD according to the Przepiorka Criteria (Appendix 7) at
Day +100, Month 6, Month 12 and Month 24
10.4.12. The Chronic GVHD Assessment Form8 (Appendix 9) is to be completed at 100
days, 6 months, 12 months, and 24 months post transplant, or until relapse or
death (whichever occurs first)8, and at the time of diagnosis of chronic GVHD
(if applicable).
The following information will be recorded in this form:
Symptoms of GVHD
Laboratory results and/or biopsy results related to GVHD (if applicable)
Date of diagnosis of cGVHD (if applicable) as per NIH Consensus Guidelines
The Chronic GVHD Assessment Form (Appendix 9) should be completed by in-person
assessment at the clinic if possible; if in-person assessment is not possible then the information
may be collected by telephone interview.
8
Page 41 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Grade of cGVHD at onset as per NIH Consensus Guidelines
Patient weight (patient reported weight is acceptable)
Karnofsky performance status
Dose of steroids and immunosuppressive agents
Dose of steroids and other immunosuppressive agents at diagnosis of
chronic GVHD prior to the start of treatment (if applicable)
Maximum grade of acute GVHD during the time period (if applicable)
10.4.13. Number of hospitalizations (and length of each admission) from start of
conditioning up until 24 months or relapse or death, whichever occurs first
10.4.14. Infections grade 4 and 5 (CTCAE v. 4.02) to be documented and recorded in
the data collection forms
10.4.15. The following information regarding grades 4 and 5 infections to be
documented and recorded in the data collection forms; type of infection
(bacterial, viral, fungal or protozoal – suspected or documented); primary
organ involved, start date
10.4.16. Screening for CMV reactivation according to institutional practice
10.4.17. All episodes of asymptomatic CMV reactivation (infection)
10.4.18. All episodes of symptomatic CMV reactivation (disease)
10.4.19. All episodes of EBV reactivation which are either symptomatic or which
require treatment (see Section 9.10.6.)
10.4.20. List of other drugs being used by the patient at one year post transplant
10.4.21. Presence or absence of TKI inhibitor use at 100 days, and at 6, 12 and 24
months and at diagnosis of cGVHD (if applicable)
10.4.22. Frequency of bone marrow evaluations post-transplant will be according to
local standard institutional practice
10.4.23. Screening for EBV by PCR or QPCR weekly from Day 0 to Day 100 (as local
institutional resources permit) and therefore only in selected cases in some
centres (see Section 9.10.6)
10.4.24. Screening for CMV according institutional practice, recording CMV activation
requiring treatment, either with or without symptoms
10.5. Post-Transplant Questionnaires
The following questionnaires are to be completed at Months 6, 12 and 24 months post HPCT:
Bradburn Scale, Patient Chronic GVHD Severity Scoring Table, CES-D Scale, Illness Intrusiveness
Ratings Scale, FACT-BMT , EQ-5D Questionnaire, Societal Cost Questionnaire and the Health Care
Questionnaire. For descriptions see Section 11.2.16. The Patient Chronic GVHD Severity Scoring
Table should also be completed at 100 days post transplant and at the time of diagnosis of cGVHD.
The Health Care Questionnaire and Societal Cost Questionnaire should also be completed at 100
days.
End of study follow-up is 24 months post transplant or relapse or death (whichever occurs first).
See Schedule of Events for a summary of all study evaluations (Appendix 3).
Page 42 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
11. Evaluation of Outcomes
11.1. Primary Endpoint
Freedom of chronic graft versus host disease at 12 months from transplantation defined as
withdrawal of all systemic immunosuppressive agents without resumption up to 12 months after
transplantation (this end-point is binary i.e. Yes/No).
11.2. Secondary Endpoints
11.2.1. Time to Engraftment (Hematological Recovery)
Time to neutrophil and platelet engraftment will be analyzed for ALL participants
(myeloablative and RIC) and separately for patients receiving myeloablative HPCT.
Time to Neutrophil Recovery: This is defined as the time from transplant (Day 0) to the
first day of achieving an absolute neutrophil count of 0.5 x 109/L or greater for 3
consecutive measurements on different days.
Platelet Recovery: This is defined as the time from transplant (Day 0) to the first day of
achieving a platelet count of greater than 20x109/L for 3 consecutive measurements on
different days without requiring platelet transfusions in the previous 7 days.
Primary Graft Failure: This is defined as the absence of neutrophil recovery (absolute
neutrophil count less than 0.5 x 109/L) in patients surviving until at least Day +28 posttransplant
11.2.2. Chimerism
The percentage of donor cells present at day 30, 60, 100 and at 6 months post
transplant will be compared between the two study groups. Reporting of chimerism
at these time points will not be mandatory, but sites will be asked to submit chimerism
results if it is standard practice at the institution to assess chimerism at these time
points. Lymphoid, myeloid and/or combined results will be collected in the data
forms.
11.2.3. The Incidence of Acute GVHD
The incidence of acute GVHD up to Day 100 will be compared. The incidence of acute GVHD at
Day +100 and Months 6, 12 and 24 will also be compared. Acute GVHD will be graded
according to the Przepiorka Criteria (Appendix 7).
Page 43 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
11.2.4. Date of Diagnosis of Chronic GVHD
The date of diagnosis of chronic GVHD (according to the NIH Consensus Guidelines) will
be compared between the two study groups)
11.2.5. The Incidence of Chronic GVHD (Regardless of Need for
Treatment) According to NIH Consensus Guidelines
This is based on the presence or absence of cGVHD of all grades and also specifically “mild”,
“moderate” and “severe” at Day +100, and at 6, 12 and 24 months post transplant, according
to the NIH diagnostic criteria10 (Appendix 9).
11.2.6. The Incidence of Chronic GVHD (Regardless of the Need
for Treatment) According to Sullivan Criteria
This is based on the presence or absence of limited and extensive cGVHD at Day +100, 6 months,
12 months and 24 months post transplant according to the Sullivan Grading Criteria9 (Appendix
8). In regards to the Sullivan Criteria, symptoms of GVHD that occur from day +100 onwards will
be considered “chronic”; symptoms of GVHD that occur prior to day +100 will be considered
acute.
11.2.7. Time to Non-relapse Mortality
This is the time to death in the absence of disease relapse. In cases of death where there has
been disease relapse death is classed as relapse mortality even when the immediate cause of
death may be from infection or organ failure.
11.2.8.
Time to All-cause Mortality
This is the time to death from any cause.
11.2.9.
Time to Relapse of Hematologic Malignancy
This is the time to relapse of disease. It is the persistence or recurrence of the original
malignancy based on standard pathology testing for myeloid malignancies and progression or
recurrence of the original malignancy based on standard pathology or radiology testing for
lymphoid malignancies. The day of relapse is the day of the first diagnostic test demonstrating
relapse. Evidence of minimal residual disease by molecular testing in the absence of other data
will not be considered relapse.
9
A member of the Study Committee (or delegate) will use the information collected in the Chronic GVHD
Assessment Form (Appendix 9) to determine if “limited” or “extensive” chronic GVHD is present according to the
Sullivan criteria (Appendix 8).
Page 44 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
11.2.10. Graft Rejection or Failure (Yes vs. No)
This is a loss of previous hematological recovery (see above) as indicated by a neutrophil count
<0.5 x 109/L and/or platelet count <20 x 109/L of unknown cause (e.g. excluding medications,
sepsis, leukemic relapse etc) and in the presence of marrow hypoplasia involving the affected
cell line(s).
11.2.11. Serious Infection
Thymoglobulin® is a risk factor for infection. Therefore, all grade 4 and 5 infections (according
to the CTCAE v. 4.02) will be recorded in the Data Collection Forms (and reported as SAEs
according to sections 14.1.2. and 14.5.). In addition, the following information will also be
recorded in the Data Collection Forms: Type of organism (bacterial, viral, fungal or protozoal)
(suspected or documented); Activation of CMV requiring treatment (section 9.10.5.); Activation
of EBV either with symptoms or requiring treatment (section 9.10.6.); Primary organ involved.
11.2.12. CMV Activation
This is the presence of a positive test (CMV antigen, PCR or QPCR) for CMV viremia. A positive
test is one that represents an indication for treatment, the threshold being defined by each
institution. Positive tests at levels below treatment indications are not to be reported as
“activation”. CMV screening will be according to local institutional practice. (See Section
9.10.5.)
11.2.13. Organ Specific and Global Severity Ratings of Chronic
Graft versus Host Disease (NIH Consensus Guidelines)
These are individual organ system and global ratings according to NIH Consensus Guidelines10 as
assessed at Day + 100, and at 6, 12, and 24 months.
11.2.14. Number of Months on Immunosupression up to 12
Months Post Transplant
The total number of months on systemic immunosuppression up to 12 months post
transplant will be compared between the two study groups.
11.2.15. Doses of Immunosuppressive Therapy Required at 12
Months
Doses of all systemic medications required for the treatment of cGVHD at 12 months will be
reported.
Page 45 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
11.2.16. Resumption of Immunosuppressive Therapy after 12
Months
Resumption of systemic immunosuppressive drugs after 12 months will be compared
between the two study groups.
11.2.17. Presence or Absence of Immunosuppressive Therapy
at 24 Months (Yes vs. No)
The presence of immunosuppressive agents or other systemic therapy (e.g. hydroxychloroquine,
imatinib) for cGVHD at 24 months in a patient who had attained ‘success’ in the primary endpoint (absence of a need for treatment at 12 months).
11.2.18. Quality of Life
See Schedule of Events for summary of assessment (Appendix 3).
Justification for instruments:
A spectrum of previously reported validated instruments will be utilized to ensure that all
relevant patient-reported quality of life outcomes are measured:
Trial Outcome Index (TOI): The FACT-BMT is a 37-item instrument composed of the FACT-G and
transplant-specific subscale. The FACT-G is comprised of 4 domains, physical (7 items), social (7
items, including sexual satisfaction), emotional (6 items) and functional (7 items, including work,
sleep and leisure activities). The transplant-specific module contains 10 scored items, including
appetite, appearance, mobility, fatigue)47, 49; higher scores indicate better functioning. The Trial
Outcome Index (TOI) is composed of the physical, function, and transplant-specific modules50.
Chronic GVHD Symptom Scale51: The 30 item cGVHD symptom scale measures degree of bother
of cGVHD manifestations in skin, energy, lung, nutrition, psychological, eye and mouth.
Responses are captured on a five-point Likert scale (“no symptoms, or not bothered at all”,
“slightly bothered,” “moderately bothered,” “bothered quite a bit,” or “extremely bothered”).
Scores for each domain are converted to a 0-100 scale where higher scores indicating more
bother. In a previous study, although the SF-36 and FACT-BMT were sensitive to changes in
overall health, only the chronic GVHD symptom scale was sensitive to changes in patientperceived chronic GVHD severity51.
Bradburn Affect Balance Scale44: The Bradburn Affect Balance Scale has been included as an
indicator of psychological well-being
CES-D: The Center for Epidemiologic Studies Depression Scale45 will be used to measure
depressive symptomatology (emotional distress).
Page 46 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Illness Intrusiveness Ratings Scale46: Subjective well-being will also be assessed with regards to
illness-induced disruptions to lifestyles, activities, and interests using the Illness Intrusiveness
Ratings Scale. This 13 item scale evaluates illness and treatment related disruptions to valued
activities and interests. It has been previously used in patients with chronic illness such as renal
failure and both autologous and allogeneic BMT patients. Psychometric testing of the Illness
Intrusiveness Ratings Scale in a variety of chronic illness populations indicates high levels of
reliability and validity
Sociodemographic Questionnaire: Eight standardized questions will assess ethnicity, race, age,
sex, education, work status and occupation, and family income.
EQ-5D Questionnaire48: A standardized non-disease-specific instrument for describing and
valuing health-related quality of life. This instrument is also useful with respect to economic
evaluation. The EQ-5D has been specifically designed to complement other quality of life
measurements.
Administration of QOL and Health Economics Instruments:
Questionnaires will be completed by the following methods: direct completion by the study
participant using a hardcopy; verbatim telephone interview; or verbatim in-person interview.
A variety of options for questionnaire completion are being allowed in order to maximize the
questionnaire completion rate. Although patients are followed closely after progenitor cell
transplant at the transplant centres for the first 100 days post transplant, many are from out-oftown and eventually return to their home community. The option to conduct the
questionnaires by telephone interview is expected to increase the rate of questionnaire
completion.
With respect to the “Health Care Questionnaire”, source documents and clinic databases may
be used to obtain the data if the patient is too ill to participate (or cannot recall all the required
details). This is the only questionnaire in which sources other than the participant can be used
to obtain the answers to the questions.
Questionnaire administrator: This is the person who explains to the participant how to
complete the questionnaire and/or who conducts the questionnaire interview. A study
coordinator, research nurse, clinic nurse and/or administrative staff member with the transplant
centre can act as a questionnaire administrator. The physician caring for the participant should
not act as the questionnaire administrator. The questionnaire administrator should conduct a
brief check of the completed questionnaires in order to ensure questions have not been missed
accidentally or answered incorrectly. (The participant should not be questioned in detail
regarding answers or missing answers, but instructions can be repeated.) The questionnaire
administrator should indicate the method of questionnaire completion that was utilized at the
bottom of the form.
Page 47 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Participants will complete their initial QOL and Health Economics questionnaires prior to
beginning their conditioning regimen. The battery of surveys will contain ~94-156 items and will
take an estimated 20-30 minutes to complete. It is anticipated that missing data will be minimal
due to the variety of questionnaire completion methods that will be allowed.
Assessments will be conducted +/- one month for the 1 year and 2 year assessments.
Relapsed patients are eligible for ongoing QOL assessments (as appropriate depending on
their situation). The Health Economics questionnaires will be stopped at relapse.
All questionnaires are available in English and French. Participants can be enrolled in the study
even if they are not able to complete all study questionnaires due to language issues.
Questionnaires approved for use in the study are posted on the project website. Study
participants will be asked to complete all questionnaires for which there is a validated version
in the applicable language. (Participants can opt out of the questionnaire portion of the
study.)
The CES-D will be transmitted to the CBMTG 0801 Project Management Office by fax or email
pdf for data entry.
Risk and protections for study participants and conditions that will lead to breach of
confidentiality:
In order to identify at-risk patients in an ethical and timely manner, the CES-D - will be scored by
a qualified health care professional at the Project Management Office as soon as possible
following the interview with the patient. (Sites should submit the completed CES-D forms to the
project management office within 24 hours.) Recommendation for referral to “psychosocial
services” or psychiatry will be done to the caring physician (and/or study coordinator) if the
total score exceeds 15; this is the routine cut-off indicating an intensity of distress consistent
with that observed among depressed psychiatric patients. Study participants will be notified
that they and/or their physicians will be contacted if anything on their QOL surveys indicates
they are a danger to themselves or others. In addition, study participants will be told they may
skip over any questions they wish. Previous experience suggests that most participants will be
open and willing to complete QOL instruments.
11.2.19. Economic Analysis
A health economic analysis will compare the costs and health outcomes of standard care with
and without Thymoglobulin® following unrelated donor allogeneic marrow and blood
progenitor cell transplantation from a direct payer perspective. The cost analysis will use a
bottom-up, micro-costing approach, calculating costs as the product of unit prices and quantity.
The micro-cost analysis will track the utilization of healthcare resources and assign a unit cost
Page 48 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
based on wages, billings or acquisition costs. Relevant costs will include Thymoglobulin®
acquisition and administration, EBV monitoring, immunosuppressive drugs, non-prophylactic
antibodies and other drug utilization, blood products, physician fees, nursing and other health
human resources, hospital admissions and day-surgeries. Immunosuppressive and in-patient
drug utilization will be derived from hospital pharmacy records. Out-patient prescriptions will
be extracted from patient questionnaires. Healthcare utilization will be identified via chart
review, discharge abstracts and case report forms completed by all patients on an on-going
basis. The cost of utilization in all centres will be standardized using Ontario unit prices. Drug
prices will be derived from the Ontario Drug Benefit formulary, physician fees will be extracted
from the Ontario fee schedule and hospital costs will be based on Ontario Case Costing Initiative
(OCCI) average case cost estimates. As blood products are provided to hospitals without charge,
unit prices for blood products will be derived from Canadian Blood Services cost data. Other
non-hospital drug utilization will be based on a survey of retail pharmacies in Ontario. Care
giver time will be derived from patient case report forms and costs will be based on the rates of
national home care providers. Given the direct payer perspective, indirect costs such as
productivity losses to the patient and informal caregivers will not be considered. Long term
costs will be reported in present valuation discounted at a rate of 3%/annum. The time horizon
for this analysis will be from time of transplant to one year following transplant.
The addition of Thymoglobulin® following allogeneic bone marrow transplantation will increase
upfront costs. However, Thymoglobulin® can improve health outcomes and potentially reduce
long-term costs. Should the study demonstrate improved health outcomes, the second phase of
the economic study will evaluate the incremental costs and health outcomes associated with
Thymoglobulin® in a cost-effectiveness framework. Outcomes in the economic evaluation will
be reported in terms of cost per quality-adjusted life year (QALY) gained based on a generic
quality-of-life instrument, the EQ-5D (see section 11.2.16).
11.3 Collection of Additional Data
The following data will also be collected:
Maximum grade of acute GVHD in each time period
Grade of chronic GVHD at onset (according to NIH Consensus Guidelines)
Immunosuppressive therapy at time of diagnosis of chronic GVHD prior to treatment
Response of chronic GVHD to immunosuppressive therapy.10
10
Response to therapy will be assessed by comparing doses of immunosuppressive therapy recorded at the next
set time period. (Time periods for assessment are 100 days, 6 months, 1 year and 2 years.) This information will
be collected in the “Chronic GVHD Assessment Form”.
Page 49 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
12. Criteria for Removal from Protocol Therapy and Off Study Criteria
All participants will be followed from registration until death or at least 24 months from the day of
transplant. Participants will be considered off study if their transplant is delayed for any reason and it is
not possible to proceed to transplant; the participant withdraws consent from the study.
13. Statistical Considerations
13.1. Data Management
Information will be collected and recorded on Data Collection Forms (posted on the 0801
website). These will be completed at study entry (registration and randomization), day +100 then
at 6, 12, and 24 months post transplant (or until time of relapse or death, whichever is sooner).
Copies of the completed Data Collection Forms are to be submitted to the Project Management
Office within 30 days of each assessment time-point. The original Data Collection Forms,
Questionnaires and source documentation will be stored at each site.
13.2. Sample Size Calculation
The primary endpoint is the freedom from chronic graft versus host disease, as indicated by the
withdrawal of all systemic immunosuppressive agents and without resumption up to 12 months
after transplantation. If we assume that the no treatment group (i.e. the control group) has a
probability of response of 0.4 (higher than previously described and erring on the side of caution)1,
it would be clinically worthwhile to know if patients administered Thymoglobulin® could
increase this response proportion by at least an additional absolute difference of 0.2, to 0.6. To be
able to detect this difference or more as statistically significant at the type I error (2-sided) level of
0.05 with a power of 0.8, a total sample size of 194 patients would be required (East version 5.1.).
Assuming, conservatively, that 2% of patients are lost to follow-up in each group (based on
personal communication with a number of our colleagues across Canada) a total of 198 patients
would be recruited. We chose not to adjust the sample size for non-compliance for three reasons:
1) we expect rates of non-compliance to be close to zero based on experience in a previous
randomized trial52; 2) our trial size was already increased based on a conservative estimate of
losses to follow and 3) our trial is pragmatic in nature with an intention to treat analysis plan.
3
The primary endpoint could be construed as a "focused stringent-positive" variation of "chronic
GVHD-free survival." The ability to withdraw all immunosuppression serves as "stringent"
evidence that the patient did not have chronic GVHD, and patients must survive to this
"positive" milestone in order to claim success. The proposed endpoint has the advantage of
being analyzed as a success event, whereas "chronic GVHD-free survival" can be analyzed only as a
"compound" failure event. For "chronic GVHD-free survival," death or recurrent malignancy at
any time before the 1-year time point for assessment counts as failure, regardless of whether the
event occurred before or after the withdrawal of immunosuppression. With this endpoint, the
Page 50 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
intervention is being tested for its ability not only to prevent chronic GVHD but also for its ability
to prevent death and recurrent malignancy before the time point for assessment.
For the primary endpoint, death (or recurrent malignancy) before withdrawal of
immunosuppression equates to failure in the sense that success cannot be attained, but death or
recurrent malignancy after withdrawal of immunosuppression (before the 1-year time point for
assessment) still counts as success. This approach sharpens the "focus" on chronic GVHD as
outcome of greatest interest by not requiring the intervention to prevent death and recurrent
malignancy after it has provided the benefit of preventing chronic GVHD.
As quality of life is a secondary endpoint for this randomized trial, the available sample size is
predetermined by the primary endpoint of cGVHD at one year. Thus statistical considerations will
focus on the power to detect clinically meaningful differences in quality of life based on the
available sample size.
Hypotheses will address differences between the two treatment groups for FACT-BMT and the
chronic GVHD symptom scale over 3 potential time points: 6 months, 12 months and 24 months
post transplant. All other hypotheses will address differences between the 2 treatment groups for
each of the other instruments listed in sections 11.2.16. over 2 potential time points: pretransplant and at 12 months post transplant. For illustrative purposes, using a Type I error of 0.05,
2-sided testing and 100% compliance with quality of life assessments we will have 88% power53 to
detect a clinically meaningful 0.5 standard deviation difference in the FACT-BMT scores
(approximately 10)51 at the 12-month time point. A drop in the available sample size due to 80%
compliance, say, would result in a power of 81%53.
Given the possibility that the assumption made in the sample size calculation regarding the
control group proportion at 1 year might not hold, an interim check conducted on the blinded
data will occur after 50% (n=97) of the patients have reached the 1-year endpoint54. If it reveals
that the 1-year proportion is not in keeping with the proportion assumed in the sample size
calculation then a revised sample size will be calculated using a modified control group event
proportion. This change will be documented in a protocol amendment.
13.3. Stratification/Minimization
We will seek to achieve a balanced allocation of treatments over prognostic factors for cGVHD.
Known a priori prognostic factors are participant age (<10; 10-30; 31-50; > 50)55; female donor for
male recipient56 ; blood source of progenitor cells rather than bone marrow (highly significant for
related donors and the subject of present NMDP study of unrelated donors)59; and degree of
tissue type matching60 (full match; one antigen/allele mismatch). There are other risk factors for
cGVHD that have been identified but which will not be considered; first, a diagnosis of chronic
myeloid leukemia (established predominantly for related donors only)55, 57; second, choice of
donor (related vs. unrelated)61 which is not relevant to this proposal which uses unrelated donors
Page 51 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
only; third, are those for which information is not available at baseline i.e. the prior occurrence of
aGVHD55 and cytokine gene polymorphisms62. In addition to balancing for the above variables that
are risk factors for cGVHD it will also be necessary to balance those variables that will influence
relapse and mortality, these being disease and stage (Early vs. Late – see footnote11), and type of
preparative regimen (myeloablative vs. non-myeloablative)63. Finally, it will be necessary to
balance by centre to allow for differences in clinical practice.
Given the moderate size of the trial and the numerous strata that would result from our stated
aim of achieving balance upfront for the above-mentioned factors it would be impractical to use
stratified randomization; furthermore, potentially large overall imbalances in treatment allocation
could occur, defeating the purpose of stratified randomization. Instead patients will be allocated
to the treatment groups based on a method of dynamic allocation referred to as minimization. As
the name implies the method attempts to minimize the differences between treatment groups in
terms of these factors. Unlike stratified randomization, where each strata represents a
combination of each of the factors identified, minimization tries to achieve overall balance by
trying to achieve balance within each individual factor, not every combination of factors. This
alternative approach to balancing factors between treatment groups allows the possibility of
balancing over more factors. As demonstrated in a simulation study66 minimization can
incorporate 10 to 20 factors without difficulty.
Using minimization in our study the first patient will have their treatment randomly allocated (akin
to flipping a fair coin). For each subsequent patient we will determine which treatment would
lead to better balance between the groups with respect to the baseline prognostic variables
identified a priori. Each patient is then randomized using a weighting in favour of the treatment
that would minimize the imbalance. A weighting of 4 to 1 will be used in this study67, 68. That is,
there will be a probability of 0.8 of receiving the treatment that minimizes the imbalance. Thus,
the study statistician (T. Panzarella) will prepare two randomization lists using a computer random
number generator before the study begins: 1) a simple randomization list where both treatments
occur equally often; this list will only be used when the two treatments have equal sums for the
levels of the baseline prognostic factors; and 2) a list in which the treatment with the smaller total
of patient levels occurs with probability 0.8 while the other treatment occurs with probability 0.2.
Allocation will occur centrally by the Project Manager through the project management office (see
Section 7.7.1). This approach ensures that the process of treatment allocation will be concealed
from staff at the participant’s centre.
11
Early disease is defined as (de novo) AML or ALL in CR1; CML in CP1; MDS in Low or Intermediate-1 group by
IPSS76 or WHO-WPSS77; CLL and lymphoma with chemotherapy-sensitive disease OR most recent relapse free
interval greater than six months. All other states are designated as Late disease (including secondary and/or
therapy related AML in CR181, 83 and therapy related ALL in CR182). Other diagnoses are not classified as Early or
Late and will be included in the “other” category. (This includes CMML.81)
Page 52 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
13.4. Analysis
The primary endpoint, freedom from chronic graft versus host disease, as indicated by withdrawal
of all systemic immunosuppressive agents and without resumption up to 12 months after
transplantation, will be compared between treatment groups using logistic regression adjusted for
covariates employed in the design. This will yield significance tests of proper size69. Patients who
die or have recurrent or progressive malignancy within the first year but after withdrawal of
immunosuppression are considered a ‘success’ for the primary endpoint. Death or recurrent or
progressive malignancy occurring before withdrawal of all systemic immunosuppressive treatment
is treated as ‘failure’ for purposes of the primary endpoint. Withdrawal of immunosuppression
prompted by persistent malignancy / imminent death is not counted as success.
Secondary endpoints will also be collected and compared between treatments. These include time
to engraftment (all participants and also participants receiving myeloablative HPCT only),
comparison of percentage of donor cells (chimerism) at day 30, 60 and 100 and 6 months post
HPCT (non-myeloablative/RIC cohort only), incidence of acute GVHD, the date of diagnosis of
chronic GVHD (if applicable) according to the NIH Consensus Guidelines, the incidence of cGVHD
(regardless of need for treatment) according to NIH Consensus, the incidence of limited and
extensive cGVHD (Sullivan Criteria), time to non-relapse mortality, time to all-cause mortality,
time to relapse of hematologic malignancy, graft rejection or failure (Yes vs. No), incidence of
serious infection, incidence of CMV activation, incidence of specific grades of chronic GVHD (by
NIH Consensus Guidelines), number of months on immunosuppression up to 12 months post
transplant, doses of immunosuppressive therapy at 12 months, resumption of
immunosuppressive therapy after 12 months (Yes vs. No), presence or absence of
immunosuppressive therapy at 24 months (Yes vs. No), quality of life, cost effectiveness.
Comparisons of time to failure endpoints will incorporate Kaplan-Meier probability estimates, log
rank testing and, when adjustment of covariates is made, use of the Cox proportional hazards
model. If the analysis of a time to failure endpoint involves competing risks then the probability of
failure will be estimated using the cumulative incidence function70.
Binary/categorical secondary endpoints will be compared between treatment groups using logistic
regression. Doses of immunosuppressive drugs required at 12 months will be compared between
treatment groups using multiple regression. Quality of life will be measured before transplant and
at 6, 12, 18, and 24 months post transplant using instruments outlined in sections 9.2, 9.5 and
10.2.13. A cross-sectional analysis comparing the 2 treatment groups at each time point will occur
using an appropriate regression model adjusted for baseline variables including pre-transplant
quality of life. An exploratory analysis using a repeated measures regression model will be used to
compare treatment groups over time while accounting for the correlation within a patient over
repeated measures71. The effect of missing data and outliers will be subjected to sensitivity
analysis72. The results for each of the primary and secondary endpoints will be summarized by a
Page 53 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
significance test and 95 per cent confidence interval. Analysis of secondary endpoints and subgroup analyses (see next paragraph) will be considered exploratory and hypothesis generating.
Given that multiple comparisons increase the probability of a Type I error, adjustment of
individual statistical tests using a more strict cut point (p<0.01) will be used to facilitate
interpretation. All statistical tests quoted will be 2-tailed. Analysis will follow the intention-totreat principle. Most analyses will be conducted using SAS version 9.2. However, competing risk
failure time data will be analyzed using the library cmprsk in R (http://www.r-project.org).
Sub-group analysis will be conducted as follows: The two treatment groups will be compared
among subgroups based on the covariates diagnosis, gender, type of preparative regimen
(myeloablative vs. non-myeloablative), donor age and recipient age as defined in section 12.3.
Differences between treatments by subgroup will be tested using interaction effects. Results will
be considered hypothesis-generating.
13.5. Interim Analysis
One interim analysis will be conducted after half of the evaluable patients have been recruited
and followed for one year. A group sequential design utilizing the Lan-DeMets spending function
with an O’Brien-Fleming stopping boundary will be incorporated. Details of the stopping
boundaries are outlined in the table below. As a result of the interim look the trial could be: 1)
stopped early by rejecting the null hypothesis of no treatment difference; 2) stopped early by
rejecting the alternative hypothesis that the difference in proportions is at least 0.2; or 3) the
study is continued.
If the null hypothesis is true we expect to stop the study early after accruing, on average, 167
patients. If on the other hand the alternative hypothesis is true, we expect to reject the null
hypothesis and stop the study early after accruing, on average, 174 patients.
Analysis
Number
Sample size
(evaluable
patients)
Beta spent
Alpha spent
Stopping boundary for
rejecting null hypothesis
(Z statistic)
Stopping boundary for
rejecting alternative
hypothesis (Z statistic)
1
97
0.003
+ 2.963
0.04
+ 0.356
2
194
0.05
+ 1.969
0.20
+ 1.969
Page 54 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
13.6. Handling of Missing Data
Missing values represent a potential source of bias in a clinical trial. As stated in the ICH12
guideline “STATISTICAL PRINCIPLES FOR CLINICAL TRIALS” (guideline E9), “Unfortunately, no
universally applicable methods of handling missing values can be recommended”. Multiple
imputation is a strategy for handling missing data that attempts to incorporate missing data
uncertainty, and so will be utilized in this study.
13.7. Loss to Follow-up
In a similar multicenter randomized study, the CBMTG centres52 have been able to demonstrate a
high level of compliance. Based on that study, we anticipate 100% compliance both with the
preparative regimen and with administration of the GVHD prophylaxis. These are the primary
areas in which compliance problems might be expected. Since BMT is a medically intensive
intervention and requires follow-up by the BMT center frequently within the first 1-2 years postBMT, the possibility of loss to follow-up is very low. This was not an issue in the previous CBMTG
study52, in which only 1 of 228 patients was lost to follow-up. In this study, we anticipate that we
will lose ≤5% of patients to follow-up.
14. Adverse Events and Serious Adverse Events
14.1. Definitions
14.1.1. Definition of an Adverse Event
The ICH13 definition of an adverse event is: Any untoward medical occurrence in a patient or
clinical investigation participant administered a pharmaceutical product and which does not
necessarily have a causal relationship with this treatment. An adverse event (AE) can therefore
be any unfavourable and unintended sign (including an abnormal laboratory finding, for
example), symptom, or disease temporally associated with the use of a medicinal
(investigational) product, whether or not related to the medicinal (investigational) product.
For the purposes of this study, Thymoglobulin® is the “investigational” product.
14.1.2. Definition of a Serious Adverse Event (SAE)
The ICH definition of a Serious Adverse Event is any untoward medical occurrence that either:
Results in death
12
International Conference on Harmonization, www.ich.org.
13
International Conference on Harmonization, www.ich.org.
Page 55 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Is life-threatening
Requires inpatient hospitalization or prolongation of existing
hospitalization (or admission to ICU)
Results in persistent or significant disability/incapacity, or
Results in a congenital anomaly/birth defect.
14.1.3. Definition of an Unexpected Adverse Reaction
According to the ICH Guidelines: An unexpected adverse reaction is one in which the nature or
severity is not consistent with the applicable product information (e.g. Investigator’s Brochure).
For the purposes of this study, an unexpected adverse reaction is one that would not be
expected during or following the administration of Thymoglobulin®.
14.1.4. Attribution of Causality and Definitions
Investigators are required to assess the relationship, if any, of each AE (that meets the criteria
for reporting) to Thymoglobulin®. Clinical judgment is to be used to determine the degree of
certainty with which an AE can be attributed to Thymoglobulin®. Causality criteria are defined
as follows:
Not related: There is another obvious cause of the AE
Doubtful: There is another more likely cause of the AE
Possible: The AE could have been due to Thymoglobulin®
Probable: The AE is probably attributable to Thymoglobulin®
Very likely: The AE is most likely attributable to Thymoglobulin®
14.2. Adverse Event Monitoring and Source Documentation
All participants are to be assessed for adverse events according to local institutional practice
following standard HPCT except where additional assessment is required per protocol. Source
documentation of adverse events should be according to institutional practice, except in cases
where additional information is required to be documented by the protocol.
Donors are individuals who are remote from this study, donating at distant sites, mostly from
beyond Canada. In providing a progenitor cell product they will be undergoing procedures that
will not differ from those that they would have undergone had the participant not been enrolled
in this research study. Donor safety is protected by adherence to the regulations or standards of
their country of origin (e.g. FACT, Health Canada, Federal Drug Authority, JACIE etc). Transplant
centres involved in this study are not responsible for monitoring donor safety; they are
responsible only for the safety of the participants.
Page 56 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
14.3. Adverse Event Reporting
Adverse events will be reported in the Data Collection Forms on both study arms as described in
this section.
Adverse event reporting should begin on the day the preparative regimen commences.
All adverse events of grade 3 or greater (see Section 14.4) must be recorded in the “Adverse Event
Data Collection” form up until Day 30 post transplant. After Day 30, SAEs only will be recorded
(see sections 14.1.2 and 14.5).
The start date of each adverse event (that meets the criteria for recording) must be recorded in
the “Adverse Event Data Collection” form. The start date is defined as the date the adverse event
first meets the criteria for grade 3 or greater. Stop dates do not need to be recorded unless the
event is a serious adverse event (SAE) meeting the criteria for expedited reporting (See Section
14.5.).
Abnormal laboratory results do not need to be recorded unless considered by the investigator to
be relevant in terms of participant or trial safety (or in relation to a serious adverse event that is
being reported).
14.4. Grading of Adverse Events
The NCI Common Toxicity Criteria (CTCAE) Version 4.02 will be used to grade adverse events that
participants experience. A copy of version 4.02 of the CTCAE can be downloaded from the CTEP
home page [http://ctep.info.nih.gov]. Additionally, if assistance is needed the NCI has an Index to
the CTCAE that provides help for classifying and locating terms.
14.5. Serious Adverse Event (SAE) Reporting Criteria (Sites)
All SAEs as defined in Section 14.1.2 (unexpected AND expected) must be reported to the Project
Management office within 24 hours of the site’s knowledge of the SAE. The Principal Investigator
(or Co-Investigator) at the site should make the determination as to whether the SAE is
“expected” or “unexpected”. The “Serious Adverse Event (SAE) Expedited Report” form should be
used to report these SAEs. This form should be faxed to the Project Management Office at: (604)
875-5584.
The time period for reporting of SAE’s is from the start of the preparative regimen up to end of
study follow-up (24 months or death, whichever occurs first). The exception is participants who
relapse prior to the end of the study follow-up period. Please see next paragraph for instructions
regarding participants who relapse.
Participants who relapse:
Page 57 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Once a participant has relapsed, it is not necessary to report SAE’s to the Project Management
Office, except in the case of death. If a participant with disease relapse dies prior to the end of
the study follow-up period, then the “Serious Adverse Event (SAE) Expedited Report” form must
be submitted to the Project Management Office .
Important Note Regarding EBV:
Symptomatic and/or treated EBV reactivation will be considered an SAE (as this is a potentially
life-threatening adverse event).
14.5.1. Reporting of Participant Deaths (Sites)
All participant deaths must be reported to the Project Management Office within 24 hours of
the site’s knowledge of the death using the “Serious Adverse Event (SAE) Expedited Report”
form. This requirement is applicable from the start of the preparative regimen up to end of
study follow-up (24 months or death, whichever occurs first).
Death is considered a separate SAE from the SAE that precedes the death (i.e. the SAE leading
to the death). A separate SAE form must be completed.
14.6. Reporting of Secondary Malignancies (Sites)
If a participant develops a secondary malignancy at any time during study follow-up, this must be
reported to the Project Manager within 24 hours from the time the transplant centre becomes
aware (for review by the Study Chair). Post Transplant Lymphoproliferative Disorder is included
as a second malignancy.
14.7. Pregnancies (Sites)
Pregnancies occurring during study follow-up (24 months) must be reported by the investigational
staff within 1 working day of their knowledge of the event using the Pregnancy Notification Form.
Follow-up information regarding the outcome of the pregnancy and any postnatal sequelae in the
infant will be required. Pregnancies in partners of male participants included in the study must
also be reported.
14.8. Reporting of Serious Adverse Events to Government
Regulatory Agencies
14.8.1. Canada
The Sponsor (CBMTG) or delegate will be responsible for reporting Serious Adverse Events to
Health Canada according to Health Canada Guidelines. Participant deaths that are “expected” will
not be submitted to Health Canada (unless the DSMC and/or Study Steering Committee conclude
the death constitutes a safety concern).
Page 58 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
14.8.2.
International Sites
A lead site will be identified in each participating country. That site is responsible for reporting
Serious Adverse Events to the regulatory agency of that country according to applicable laws
and guidelines.
14.9. SAE Notifications
The Study Chair and/or Study Steering Committee will review all SAE’s received from the sites. If
an SAE is confirmed as being “unexpected” and/or significant with respect to participant safety,
then an “SAE Notification” summarizing the SAE will be distributed to participating sites.
14.10. Reporting of SAEs to Institutional Review Boards (IRB’s)
Sites should follow the guidelines of their local IRB with respect to the submission of SAE’s that
occur at the site as well as SAE Notifications.
14.11. Reporting of SAEs to Genzyme
Reporting of SAEs to Genzyme is the responsibility of the Project Management Office.
All SAEs that occur in participants randomized to the Thymoglobin® Arm (Arm B) must be
reported to Genzyme. (SAEs that occur in participants randomized to the No Thymoglobulin®
Arm (Arm A) do not need to be reported to Genzyme.) The Project Manager (or delegate) must
report SAEs involving a participant in Arm B (Thymoglobulin) to Genzyme within 24 hours of the
receipt of the site SAE report at the Project Management Office. All reports will be emailed to:
Genzyme Global Patient Safety and Risk Management
Fax 617-761-8506
PharmacovigilanceSafety@genzyme.com
The Project Manager (or delegate) will be responsible for communicating with Genzyme regarding
follow-up information related to SAEs. If Genzyme requires further information regarding an SAE
they will notify the Project Management Office. Genzyme will not contact sites directly.
14.12. Review of SAEs by the Medical Monitor and Statistician
The Study Chair (or delegate as agreed upon by the Steering Committee) will act as the
Medical Monitor for the study. The role of the medical monitor is to:
Review all individual SAEs that are reported
Visit sites as necessary to review data related to the safety of the participants
enrolled
Page 59 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Communicate with the DSMC regarding any SAEs which may necessitate a change
to the protocol and/or consent form
Communicate with site personnel, regulatory agencies, IRB’s, etc as necessary
The Medical Monitor will not review summarized SAE data (unless asked to do so by the
DSMC). The statistician will review summarized SAE data every 6 months (or more
frequently if necessary).
15. Data Safety Monitoring Committee
During the course of the study, an independent Data Safety Monitoring Committee (DSMC) will review
efficacy and safety data.
As described in Section 13.5, one interim analysis is planned. The DSMC will convene every 6 months.
Additional meetings/conferences calls will be conducted as necessary. The DSMC will use their
experience in reviewing the data submitted to them which will be done every 6 months. Specific
concerns of the investigators will be addressed, these being outcomes in the experimental
(Thymoglobulin®) arm which are sufficiently adverse compared to those in the control arm, with respect
to either:
a) The primary end-point, OR
b) An unacceptable number of serious toxicities due to Thymoglobulin® , OR
c) A significant increase in non-relapse mortality, infection related mortality, disease relapse or graft
failure.
All SAE’s received by the Project Management Office will be submitted to the DSMC as follows:
Unexpected SAE’s and/or SAE’s felt to be significant with respect to participant safety will be submitted
to the DSMC within 48 hours of receipt by the Project Management Office. All other SAE’s will be
submitted to the DSMC as part of the routine 6 month review process.
16. Records and Reporting
16.1. Data Management
The CBMTG 0801 Project Management Office (located in Vancouver, BC, Canada) will perform the
randomization, data collection and management, site monitoring, administration, meeting
support, and statistical support. A centralized database will be utilized and housed on a secure
server with daily backup. The project manager will communicate with data management and
clinical research personnel in each of the participating institutions.
Page 60 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
16.2. Data Entry, Confidentiality and Security
Data Collection Forms and Quality of Life Forms will be faxed to the Project Management Office at
the pre-specified registration and at follow-up time points. Data will be identified by an
alphanumeric code only. Data will be entered (by staff at the Project Management Office) into
the database using a web based electronic data capture system. The server for the database will
be located in the Leukemia/BMT Program of BC administrative office (in Vancouver, BC).
Appropriate security measures will be in place such that current Canadian privacy laws are
adhered to with respect to security and confidentiality of data, electronic data transmission, data
storage and data access. A secure ID and password will be necessary to access the system. Audit
trails of entries will be provided. The Project Manager and delegate will be the only individuals
that can edit data.
During the course of the study, web based data entry may be expanded to participating sites. Site
staff will only have authorization to enter and view data for participants at their site. Site staff
will not be able to edit data once they have submitted it. (See previous paragraph regarding
confidentiality and security measures.)
16.3. Specific Instructions to Participating Sites Regarding 16.2.
Sites should assign a temporary code using a letter and a number. The letter should not include
any actual initials of the participant and the number should be a unique number (i.e. not a hospital
number, SIN number or any other number that could be used to identify the participant). This
temporary code will be entered on the randomization form that is sent to the Project
Management Office. The Project Management office will then assign a permanent unique and
confidential alphanumeric code. This alphanumeric code will be entered on the randomization
form by the Project Management Office. The randomization form is sent back to the site once all
the administrative information has been entered: permanent alphanumeric code, date of
randomization, signature of person who completes the randomization, study arm assigned. The
site should keep a log that links the temporary code to the permanent alphanumeric code to the
participant's name and DOB. This log should never leave the site. (i.e. it should never be sent to
the sponsor). The permanent alphanumeric code will be used to identify all the data collection
forms that are sent to from the site to the Project Management Office. The permanent
alphanumeric code should be used regarding any other communication between the site and the
Project Management Office.
16.4. Access to Database and Statistical Analysis
The Project Manager (and delegate) will be the only individuals who have authorization to transfer
data to the statistician for study analysis. Statistical analysis will be carried out using SPSS and SAS
software.
Page 61 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
17. Regulatory Ethics Compliance
17.1. Investigator Responsibilities
The investigator at each site is responsible for ensuring that the clinical study is performed in
accordance with the protocol, current ICH Guidelines on Good Clinical Practice (GCP), and
applicable regulatory requirements.
GCP is an international ethical and scientific quality standard for designing, conducting, recording,
and reporting studies that involve participation of human participants. Compliance with this
standard provides public assurance that the rights, safety, and well being of study participants are
protected, consistent with the principles that originated in the Declaration of Helsinki, and that
the clinical study data are credible.
17.2. Independent Ethics Committee or Institutional Review Board
This study will be undertaken at a site only after IEC/IRB has given full approval of the final
protocol, amendments (if any), the informed consent form(s), applicable recruiting materials, and
the study management center has received a copy of this approval. This approval letter must be
dated and must clearly identify the documents being approved. The study management center
will require a copy of all IEC/IRB documents.
18. Study Monitoring and Auditing
The project manager will review the protocol and Data Collection Forms with the investigator and study
staff before study initiation at the site initiation visit or the investigator's meeting.
A monitor will visit sites as needed throughout the duration of the study to verify the quality of data and
to ensure the standards of Good Clinical Practice are being met. (The monitor may be a member of the
Study Steering Committee or delegate.) The Study Chair and/or delegate acting in the role of Medical
Monitor will visit the sites as necessary to review data related to the safety of study participants.
The investigator must give the monitor and/or medical monitor access to relevant hospital or clinical
records to confirm their consistency with the Data Collection Form entries. No information in these
records about the identity of the patients will leave the study centre. Monitoring standards require
verification of the presence of informed consent, adherence to the inclusion/exclusion criteria,
documentation of all adverse events required as per protocol, G-CSF administration, and the recording
of primary efficacy and safety variables.
Investigator(s) and/or the participating institutions must permit monitoring and auditing by their local
ethics board (REB/IRB/IEC) as necessary. Monitoring and/or auditing by applicable government
Page 62 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
regulatory agencies must be permitted. Monitoring and/or auditing by the Canadian Institutes of Health
Research (CIHR) must be permitted.
The Study Steering Committee will appoint auditors from outside the Study Steering Committee. The
Study Steering Committee will determine which sites are audited based on the number of participants
enrolled, the nature of issues identified during monitoring visits and as felt to be necessary in order to
maintain the quality of the data. Due to the complex nature of this study, a member of the study
steering committee may accompany an auditor as necessary.
19.
Drug Accountability
The site pharmacy must keep a drug accountability log for Thymoglobulin® . The following information
must be included: Date of dose, patient name and either a Date of Birth and/or hospital ID number,
number of vials per dose, lot number of each vial, expiry date of each vial and the initials of the person
who recorded the information. The weight of the patient should also be recorded.
Page 63 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Appendix 1
Informed Consent Form Template (Participants 19 – 70)
Informed Consent Form Template (Participants 16-18)
Page 64 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
(Participants 19 – 70)
Information/Consent Form (Participant)
PROJECT TITLE
A Randomized Trial of Thymoglobulin® to Prevent Chronic Graft versus Host Disease in Patients
Undergoing Hematopoietic Progenitor Cell Transplantation from Unrelated Donors.
PRINCIPAL INVESTIGATOR FOR CANADA
Dr Irwin Walker, MBBS, FRCP(C), FRACP, McMaster University and Hamilton Health Sciences
SPONSOR AND FUNDING
The sponsor is McMaster University, Faculty of Health Sciences. Administrative support is provided by
the Canadian Blood and Marrow Transplant Group (CBMTG), a non-profit multi-disciplinary organization.
This research project is funded by the Canadian Institutes for Health Research, Health Canada, and by
Genzyme Corporation, Cambridge, MA.
THE REASON FOR THIS RESEARCH PROJECT
We are trying to decrease the likelihood and severity of graft versus host disease. You are being invited
to participate in this research project because you are having either a bone marrow or blood progenitor
cell transplant from an unrelated donor and because graft versus host disease is a frequent and
sometimes serious complication of this procedure. Your participation in this study is entirely voluntary
and choosing not to take part will not affect your decision to have the transplant or the standard of
medical care which you will receive.
The project is testing whether giving a medication known as Thymoglobulin® will decrease the
frequency and severity of graft-versus-host disease (GVHD), a common and serious side effect of
transplantation. In order to decide whether or not you want to be a part of this research study, you
should understand what is involved and the potential risks and benefits. This form gives detailed
information about the research study, which will be discussed with you. Once you understand the
study, you will be asked to sign this form if you wish to participate. Please take your time to make your
decision. Feel free to discuss it with your friends and family, and/or your family physician
You will be receiving a bone marrow or blood progenitor cell transplant from a donor who is not related
to you. GVHD is more likely to occur than if you had had a donor who was related to you. The likelihood
that GVHD will occur is about 80%. As well, GVHD is also more likely to be severe when the donor is
unrelated. This means it (GVHD) is more likely to be life-threatening or to seriously affect your long
term health even if the underlying cancer is cured. GVHD is the most common reason that transplants
fail when unrelated donors are used, which is why we are testing Thymoglobulin®.
Graft-versus-host disease (GVHD) is a reaction of the donor’s immune system against the recipient’s
(your) tissues. When GVHD is mild and directed mainly against the cancer it is a benefit because it
decreases the likelihood that the cancer will relapse. However, if it reacts against your normal tissues it
Page 65 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
may be harmful, even life threatening. The harm from it usually outweighs its benefit. We would want
you to have a mild degree of GVHD for the benefit, but we want to prevent it being severe.
When GVHD starts within three months after transplantation it is called acute GVHD. Acute GVHD
causes skin rashes, inflammation of the liver and gastrointestinal side effects such as nausea, diarrhea
and ulcers. When GVHD continues or starts after three months it is called chronic GVHD. Chronic GVHD
commonly affects the skin and soft tissues, can interfere with movement, causes soreness of the mouth
that can interfere with eating, and can cause dryness and soreness of the eyes. Chronic GVHD can also
affect many other parts of the body, including the lungs. Chronic GVHD is less likely than acute GVHD to
be life-threatening but it causes ill health that can last for a number of years. Both acute and chronic
forms of GVHD cause delays in recovery of the immune system making you at risk of infections that
themselves can be dangerous.
HOW MANY PEOPLE WILL TAKE PART IN THE STUDY
About 198 patients from Canada (mainly), and possibly other countries, will take part in this study. It
will take about 3.5 years to enroll all the patients. Patients will be followed by the transplant team for 2
years after the transplant for this research, but for your health as long and as often as recommended.
WHAT IS THYMOGLOBULIN® ?
Thymoglobulin® is a concentrated solution of antibodies made from the serum of rabbits after they
have been injected with the human immune cells that cause GVHD. The rabbits react to the human
immune cells by producing these antibodies. These antibodies are refined into the product known as
Thymoglobulin® that can then be used to reduce the number of donor immune cells that cause GVHD.
Thymoglobulin® is a medication that is given by vein (intravenous). It has been tested in Europe and is
licensed for use in bone marrow transplantation to prevent GVHD. In North America, Thymoglobulin®
is licensed for use only in kidney transplantation. We would like to test its use in patients who are
having allogeneic bone marrow or blood progenitor cell transplants in Canada, so as to confirm the
beneficial results in the European studies and establish its use here in North America.
WHAT ARE THE POSSIBLE RISKS AND DISCOMFORTS?
The risks are having side effects of Thymoglobulin®. Side effects from Thymoglobulin® are quite
common, but are nearly always temporary and settle with medication or once the infusion is over.
About 60% of people will have a mild fever during the intravenous infusion, about 30% will have
shivering or a skin rash. Occasional patients (5-10%) may have a drop in blood pressure. If such
reactions are severe, the infusion may be stopped for a time until the symptoms clear. Benadryl,
acetaminophen (e.g. Tylenol) and steroids are given before the infusion to minimize these reactions and
may be repeated during the infusion. When reactions occur they are most likely to be troublesome only
Page 66 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
on the first day. It is most unlikely that side effects would be severe enough to discontinue
Thymoglobulin® altogether.
Another (possible and theoretical) side effect of Thymoglobulin® could be to increase the chance that
you may develop a serious infection, but when tested in Europe this wasn’t so. You will be monitored
closely for such infections.
Based on previous studies, the addition of Thymoglobulin® to the preparative regimen does not appear
to significantly increase the risk of relapse.
A potentially very serious side effect is infection with a special virus called EB virus that can lead to
lymph gland cancer (Post Transplant Lymphoproliferative Disorder). This has been reported on rare
occasions following bone marrow transplantation and is more common when Thymoglobulin® is used.
It appears to be uncommon, occurring in approximately 3% of transplant recipients. Your blood will be
tested once a week for EB virus infection. Treatment is often very effective when given soon after
infection is detected.
WHAT ARE THE POSSIBLE BENEFITS FOR ME OF AGREEING TO TAKING PART IN THIS STUDY?
The possible benefit to me would be preventing a serious case of graft versus host disease that could
threaten my health or life.
WHAT ARE YOU CONSENTING TO?
If you agree to take part in this research project you will be taking part in a randomized trial. Your
transplant doctor will review all the information from the “pre-transplant” work-up to determine if you
are eligible for the study. If you are eligible for the study, then before the transplant, you will be
assigned by a computer (by randomized chance like the toss of a coin) to either receive Thymoglobulin®
in addition to the normal transplant procedures, or receive the transplant without Thymoglobulin® and
be part of a matching group. The chances are 50% that you will be either in the Thymoglobulin® receiving group or the matching group. We will then compare the results of the two groups. If you
decline to take part in this research project the transplant procedure will be carried out in exactly the
same way but without Thymoglobulin® being given.
If you agree (consent) to take part in this research project, the only procedure that will be different from
the normal transplant procedures, and the only research procedures that you will be consenting to will
be the infusion of Thymoglobulin® and the filling out of some questionnaires so that we can better
understand how you are feeling. The Thymoglobulin® administration and questionnaires are described
as follows:
Page 67 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
The date and schedule of other procedures for the transplant will not be changed in any way than if you
were not taking part in this project. Thymoglobulin® is given by intravenous injection over a number of
hours, each day for three days, on the day of transplant and on the two previous days. The dose on the
first day is one quarter of the dose on the other two days, the dose being 0.5 mg for each kilogram of
your body weight on the first day, and 2.0 mg per kilogram on each of the next two days. Nothing else
will be done for this project and the transplant will go ahead normally. After discharge there will be no
additional medications or procedures and you will not have to attend the clinic any more often than if
you had not taken part in the project. We will, though, ask you to fill in some questionnaires, as follows:
After the transplant we will be interested in your opinion and feelings about how the transplant has
affected you. We will ask you to fill out some questionnaires (Quality of Life questionnaires) before the
transplant and then at six, twelve and 24 months following transplant. These questionnaires take
approximately 20-30 minutes to complete. Some of the questions are personal; you can refuse to
answer these questions if you wish. The information you provide is for research purposes only and will
remain strictly confidential. The individuals (e.g. doctors, nurses, etc) directly involved in your care will
not usually see your responses to these questions – if you wish them to know this information, please
bring it to their attention.
A research nurse or research assistant who works at this transplant centre will administer the
questionnaires. This person will explain how to complete the questionnaires. If the questionnaires are
being completed by interview, it is this person who will be asking the questions. Some of the questions
are personal; You can refuse to answer any question if you wish. The person who administers the
questionnaires will check your completed questionnaires to ensure you’ve understood the directions
correctly. They are only looking for questions that you may have missed by accident or items you may
have misunderstood. They will not discuss the answers you have given in detail. (If there are questions
you have left blank on purpose, please communicate this to the person administering the
questionnaire.)
Although your individual answers will not be shared with the transplant centre team and will not be filed
in your medical chart (unless you request this), your study doctor and the study nurse may be notified of
the overall “score” (result) of one of the questionnaires (depending on your score). This questionnaire
is called the “CES-D Scale”. The purpose of this questionnaire is to assess your level of emotional
distress. Once you complete this questionnaire it will be sent to the Project Management Office. The
score of your CES-D questionnaire will be calculated. If your score indicates a high level of emotional
distress the Project Management Office will then notify {enter name of site PI and study coordinator}.
{Enter name of site PI and study coordinator} will contact you regarding a referral to a psychologist,
social worker or your family doctor. You do not have to accept this referral if you don’t wish to.
Previous studies in which the CES-D scale has been used have shown that a referral to a mental health
professional can be beneficial when a score indicates a high level of emotional distress. That is why this
process is being followed. (This process is not being followed for the other questionnaires.)
Page 68 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
The researchers would also like to collect information about your bone marrow transplant and follow-up
to compare costs related to the two different transplant procedures in this study. The researchers are
requesting your permission to access your medical chart(s) and data bases (that already exist for
auditing and accounting purposes) in order to obtain health economic information. By signing this
consent you agree that the researchers can access this information for the purposes of this study.
CONTRACEPTION AND PREGNANCY:
The effects of Thymoglobulin® on the unborn child are unknown. The effects of chemotherapy (and
other medications you may receive before and after transplant) are not well known. Therefore, women
who are pregnant or breastfeeding cannot be enrolled in this study.
Women of childbearing potential who are enrolled in the study must agree to use an adequate method
of birth control from the time of enrollment until a minimum of one year following transplant.
Men enrolled in this study must agree to use an adequate method of birth control from the time of
enrollment until a minimum of one year following transplant.
It is important that you discuss the implications of discontinuing birth control after one year post
transplant with your transplant doctor. In some cases it may be recommended that pregnancy (or
fathering a child) should be prevented for a longer time period.
Adequate methods of birth control include:
Abstinence
Previous tubal ligation
Vasectomy
Oral, injectable or implantable contraceptives
Condoms
Foam
IUD
If you become pregnant (or father a child) at any time from your enrollment in this study until 2 years
following your transplant (the end of the study follow-up period), then you should inform your
transplant doctor and the study doctor immediately. You will be asked for your permission regarding
access to the health records of your pregnancy (if you are female) as well as the health records of your
infant.
WHAT HAPPENS IF THERE IS A CHANGE IN MY ELIGIBILITY FOR THE STUDY AFTER I HAVE BEEN
RANDOMIZED?
It is possible that your health status may change after you are randomized such that you no longer meet
the eligibility for the study.
Page 69 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
In some cases, your doctor will recommend that your transplant is postponed until your health is
optimal for transplant again. For example, if you require treatment for an infection, your transplant
might be postponed until the infection has resolved. In this situation, you can still fully participate in the
study as long as your situation changes so that you once again meet all the study eligibility criteria prior
to the rescheduled transplant.
In some cases, it is possible that your doctor may decide it is in your best interest to proceed with the
transplant as scheduled; However, the changes in your health status may be such that you no longer
meet all the eligibility criteria. This would affect your participation in the following way:
If you have been randomized to the “Thymoglobulin® Group”, you would no longer be able to
receive Thymoglobulin®
The researchers will follow your progress for up to 2 years following the date of randomization
The researchers will continue to collect the study data as originally planned
You will be asked to complete the study questionnaires as originally planned
In very rare cases, a transplant may need to be cancelled. In this situation, the researchers will continue
to follow your progress for up to 2 years from the date of your randomization.
IF I DO NOT WANT TO TAKE PART IN THE STUDY, ARE THERE OTHER CHOICES?
If you do not want to take part in this study it will not affect the decision to have the transplant.
Choosing not to participate in this study will in no way affect your care or treatment.
DECLARATION OF FINANCIAL INTEREST
Neither the Investigator nor the institution has a financial interest or a proprietary interest in the drug,
procedure or device under study.
RESEARCH-RELATED INJURY
If you become ill or injured as a direct result of participating in this study, necessary medical treatment
will be available at no additional cost to you.
Your signature on this form only indicates that you have understood to your satisfaction the information
regarding your participation in the study and agree to participate. In no way does this waive your legal
rights nor release the investigator, the research doctor, the study sponsor or involved institutions from
their legal and professional responsibilities.
WITHDRAWAL FROM THE STUDY
If you choose to participate and later decide to change your mind, you can say no and stop the research
at any time. A decision to withdraw from the study will not affect your health care. Your physician or the
study sponsor may stop your participation at any time, without your consent, if they feel it is in your
Page 70 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
best interest. You may be taken out of the study, if you do not follow your doctor’s instructions, if you
experience a side effect that needs medical treatment, or if the sponsor stops the study for any reason.
COMPENSATION
No costs will be charged to you for being in this study, nor will you be paid for participating in the study.
You will not be charged for the research drugs or any research procedures.
CONFIDENTIALITY
You will not be identified as a study participant in any reports or publications of this research. Your
records will be kept in a locked file cabinet in a locked room. Only the staff involved in the research
study will see them. The research records will also be sent to the national study coordinator who is at
the British Columbia Cancer Agency, but your name will be removed beforehand.
With your permission, your family doctor will also be informed of your participation in this research
study. This consent form will be placed in your Health Chart.
It is unlikely, though possible, that records could be inspected by representatives from the Canadian
Institute of Health Research, the Health Canada agency that funded this research, or Genzyme who
funded part of this research, or the ethics committee at this hospital.
WITHDRAWAL FROM THE STUDY
If you choose to participate and later decide to change your mind, you can say no and stop the research
at any time. A decision to stop being in the study will not affect your health care. Your physician or the
study sponsor may stop your participation at any time, without your consent, if they feel it is in your
best interest. You may be taken out of the study, if you do not follow your doctor’s instructions, if you
experience a side effect that needs medical treatment, or if the sponsor stops the study for any reason.
OTHER PERTINENT INFORMATION
Throughout the research study, you will be told about any new information that might affect your
decision about being in this research study. In particular, you will be told of any unforeseen risks that
may be identified.
WHOM DO I CALL IF I HAVE QUESTIONS OR PROBLEMS?
You should ask questions about anything that you do not understand before you sign this form. The
study staff will also be available to answer questions before, during, and after the study.
If you have questions about taking part in this study, or suffer a research related injury, you can talk to
your doctor. You can also meet with the research nurse who discussed the project with you. You can
also meet with the doctor who is in charge of the study at this institution. That person is:
{Enter Name of Site PI}
{Enter telephone number of Site PI}
Page 71 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Or, you can speak with {{Enter the name and telephone number for an independent research contact
for the institution}. You will receive a copy of this signed and dated consent form.
Page 72 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
CONSENT OF PARTICIPANT:
I have read the preceding information thoroughly. I have had an opportunity to ask questions and all of
my questions have been answered to my satisfaction. I agree to participate in this study. I understand
that I will receive a signed copy of this form.
Name
Signature
Date
Person obtaining consent (Investigator or Delegate):
I have discussed this study in detail with the participant. I believe the participant understands what is
involved in this study. In my judgment, this participant has the capacity to give consent, and has done
so voluntarily.
Name, Role in Study
Signature
Date
Witness: (required if participants are unable to read, or if translation is necessary)
I was present when the information in this form was explained and discussed with the participant. I
believe the participant understands what is involved in this study.
Name
Signature
Date
This study has been reviewed by {Insert name of REB}. The REB is responsible for ensuring that
participants are informed of the risks associated with the research, and that participants are free to
decide if participation is right for them. If you have any questions about your rights as a research
participant, please call {Insert the contact information for the representative of the REB}.
It is possible the researchers may be interested in following your health status after the 1 year follow-up
period for this study. Do you agree to be contacted in the future regarding extended follow-up? If yes,
please initial _________.
Page 73 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
(Participants 16 – 18)
Information/Consent Form for Participant and Parent(s)/Guardian(s)
PROJECT TITLE
A Randomized Trial of Thymoglobulin® to Prevent Chronic Graft versus Host Disease in Patients
Undergoing Hematopoietic Progenitor Cell Transplantation from Unrelated Donors.
PRINCIPAL INVESTIGATOR FOR CANADA
Dr Irwin Walker, MBBS, FRCP(C), FRACP, McMaster University and Hamilton Health Sciences
SPONSOR and FUNDING
The sponsor is McMaster University, Faculty of Health Sciences. Administrative support is provided by
the Canadian Blood and Marrow Transplant Group (CBMTG), a non-profit multi-disciplinary organization.
This research project is funded by the Canadian Institutes for Health Research, Health Canada, and by
Genzyme Corporation, Cambridge, MA.
WHO SHOULD READ THIS CONSENT FORM?
The information in this consent form is intended for the participant (the person who is being invited to
participate in this research project) and the parent(s) or guardian(s) of the participant.
THE REASON FOR THIS RESEARCH PROJECT
We are trying to decrease the likelihood and severity of graft versus host disease. You are being invited
to participate in this research project because you are having either a bone marrow or blood progenitor
cell transplant from an unrelated donor and because graft versus host disease is a frequent and
sometimes serious complication of this procedure. Your participation in this study is entirely voluntary
and choosing not to take part will not affect your decision to have the transplant or the standard of
medical care which you will receive.
The project is testing whether giving a medication known as Thymoglobulin® will decrease the
frequency and severity of graft-versus-host disease (GVHD), a common and serious side effect of
transplantation. In order to decide whether or not you want to be a part of this research study, you
should understand what is involved and the potential risks and benefits. This form gives detailed
information about the research study, which will be discussed with you. Once you understand the
study, you will be asked to sign this form if you wish to participate. Please take your time to make your
decision. Feel free to discuss it with your friends and family, and/or your family physician
You will be receiving a bone marrow or blood progenitor cell transplant from a donor who is not related
to you. GVHD is more likely to occur than if you had had a donor who was related to you. The likelihood
that GVHD will occur is about 80%. As well, GVHD is also more likely to be severe when the donor is
unrelated. This means it (GVHD) is more likely to be life-threatening or to seriously affect your long
Page 74 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
term health even if the underlying cancer is cured. GVHD is the most common reason that transplants
fail when unrelated donors are used, which is why we are testing Thymoglobulin® .
Graft-versus-host disease (GVHD) is a reaction of the donor’s immune system against the recipient’s
(your) tissues. When GVHD is mild and directed mainly against the cancer it is a benefit because it
decreases the likelihood that the cancer will relapse. However, if it reacts against your normal tissues it
may be harmful, even life threatening. The harm from it usually outweighs its benefit. We would want
you to have a mild degree of GVHD for the benefit, but we want to prevent it being severe.
When GVHD starts within three months after transplantation it is called acute GVHD. Acute GVHD
causes skin rashes, inflammation of the liver and gastrointestinal side effects such as nausea, diarrhea
and ulcers. When GVHD continues or starts after three months it is called chronic GVHD. Chronic GVHD
commonly affects the skin and soft tissues, can interfere with movement, causes soreness of the mouth
that can interfere with eating, and can cause dryness and soreness of the eyes. Chronic GVHD can also
affect many other parts of the body, including the lungs. Chronic GVHD is less likely than acute GVHD to
be life-threatening but it causes ill health that can last for a number of years. Both acute and chronic
forms of GVHD cause delays in recovery of the immune system making you at risk of infections that
themselves can be dangerous.
HOW MANY PEOPLE WILL TAKE PART IN THE STUDY
About 198 patients from Canada (mainly), and possibly other countries, will take part in this study. It
will take about 3.5 years to enroll all the patients. Patients will be followed by the transplant team for 2
years after the transplant for this research, but for your health as long and as often as recommended.
WHAT IS THYMOGLOBULIN® ?
Thymoglobulin® is a concentrated solution of antibodies made from the serum of rabbits after they
have been injected with the human immune cells that cause GVHD. The rabbits react to the human
immune cells by producing these antibodies. These antibodies are refined into the product known as
Thymoglobulin® that can then be used to reduce the number of donor immune cells that cause GVHD.
Thymoglobulin® is a medication that is given by vein (intravenous). It has been tested in Europe and is
licensed for use in bone marrow transplantation to prevent GVHD. In North America, Thymoglobulin® is
licensed for use only in kidney transplantation. We would like to test its use in patients who are having
allogeneic bone marrow or blood progenitor cell transplants in Canada, so as to confirm the beneficial
results in the European studies and establish its use here in North America.
WHAT ARE THE POSSIBLE RISKS AND DISCOMFORTS?
The risks are having side effects of Thymoglobulin® . Side effects from Thymoglobulin® are quite
common, but are nearly always temporary and settle with medication or once the infusion is over.
Page 75 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
About 60% of people will have a mild fever during the intravenous infusion, about 30% will have
shivering or a skin rash. Occasional patients (5-10%) may have a drop in blood pressure. If such
reactions are severe, the infusion may be stopped for a time until the symptoms clear. Benadryl,
acetaminophen (e.g. Tylenol) and steroids are given before the infusion to minimize these reactions and
may be repeated during the infusion. When reactions occur they are most likely to be troublesome only
on the first day. It is most unlikely that side effects would be severe enough to discontinue
Thymoglobulin® altogether.
Another (possible and theoretical) side effect of Thymoglobulin® could be to increase the chance that
you may develop a serious infection, but when tested in Europe this wasn’t so. You will be monitored
closely for such infections.
Based on previous studies, the addition of Thymoglobulin® to the preparative regimen does not appear
to significantly increase the risk of relapse.
A potentially very serious side effect is infection with a special virus called EB virus that can lead to
lymph gland cancer (Post Transplant Lymphoproliferative Disorder). This has been reported on rare
occasions following bone marrow transplantation and is more common when Thymoglobulin® is used.
It appears to be uncommon, occurring in approximately 3% of transplant recipients. Your blood will be
tested once a week for EB virus infection. Treatment is often very effective when given soon after
infection is detected.
WHAT ARE THE POSSIBLE BENEFITS FOR ME OF AGREEING TO TAKING PART IN THIS STUDY?
The possible benefit to me would be preventing a serious case of graft versus host disease that could
threaten my health or life.
WHAT ARE YOU CONSENTING TO?
If you agree to take part in this research project you will be taking part in a randomized trial. Your
transplant doctor will review all the information from the “pre-transplant” work-up to determine if you
are eligible for the study. If you are eligible for the study, then before the transplant you would be
assigned by a computer (by randomized chance like the toss of a coin) to either receive Thymoglobulin®
in addition to the normal transplant procedures, or receive the transplant without Thymoglobulin® and
be part of a matching group. The chances are 50% that you will be either in the Thymoglobulin® receiving group or the matching group. We will then compare the results of the two groups. If you
decline to take part in this research project the transplant procedure will be carried out in exactly the
same way but without Thymoglobulin® being given.
If you agree (consent) to take part in this research project, the only procedure that will be different from
the normal transplant procedures, and the only research procedures that you will be consenting to will
Page 76 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
be the infusion of Thymoglobulin® and the filling out of some questionnaires so that we can better
understand how you are feeling. The Thymoglobulin® administration and questionnaires are described
as follows:
The date and schedule of other procedures for the transplant will not be changed in any way than if you
were not taking part in this project. Thymoglobulin® is given by intravenous injection over a number of
hours, each day for three days, on the day of transplant and on the two previous days. The dose on the
first day is one quarter of the dose on the other two days, the dose being 0.5 mg for each kilogram of
your body weight on the first day, and 2.0 mg per kilogram on each of the next two days. Nothing else
will be done for this project and the transplant will go ahead normally. After discharge there will be no
additional medications or procedures and you will not have to attend the clinic any more often than if
you had not taken part in the project. We will, though, ask you to fill in some questionnaires, as follows:
After the transplant we will be interested in your opinion and feelings about how the transplant has
affected you. We will ask you to fill out some questionnaires (Quality of Life questionnaires) before the
transplant and then at six, twelve and 24 months following transplant. These questionnaires take
approximately 20-30 minutes to complete. Some of the questions are personal; you can refuse to
answer these questions if you wish. The information you provide is for research purposes only and will
remain strictly confidential. The individuals (e.g. doctors, nurses, etc) directly involved in your care will
not usually see your responses to these questions – if you wish them to know this information, please
bring it to their attention.
A research nurse or research assistant who works at this transplant centre will administer the
questionnaires. This person will explain how to complete the questionnaires. If the questionnaires are
being completed by interview, it is this person who will be asking the questions. Some of the questions
are personal; You can refuse to answer any question if you wish. The person who administers the
questionnaires will check your completed questionnaires to ensure you’ve understood the directions
correctly. They are only looking for questions that you may have missed by accident or items you may
have misunderstood. They will not discuss the answers you have given in detail. (If there are questions
you have left blank on purpose, please communicate this to the person administering the
questionnaire.)
Although your individual answers will not be shared with the transplant centre team and will not be filed
in your medical chart (unless you request this), your study doctor and the study nurse may be notified of
the overall “score” (result) of one of the questionnaires (depending on your score). This questionnaire
is called the “CES-D Scale”. The purpose of this questionnaire is to assess your level of emotional
distress. Once you complete this questionnaire it will be sent to the Project Management Office. The
score of your CES-D questionnaire will be calculated. If your score indicates a high level of emotional
distress the Project Management Office will then notify {enter name of site PI and study coordinator}.
{Enter name of site PI and study coordinator} will contact you regarding a referral to a psychologist,
social worker or your family doctor. You do not have to accept this referral if you don’t wish to.
Page 77 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Previous studies in which the CES-D scale has been used have shown that a referral to a mental health
professional can be beneficial when a score indicates a high level of emotional distress. That is why this
process is being followed. (This process is not being followed for the other questionnaires.)
The researchers would also like to collect information about your bone marrow transplant and follow-up
to compare costs related to the two different transplant procedures in this study. The researchers are
requesting your permission to access your medical chart(s) and data bases (that already exist for
auditing and accounting purposes) in order to obtain health economic information. By signing this
consent you agree that the researchers can access this information for the purposes of this study.
CONTRACEPTION AND PREGNANCY:
The effects of Thymoglobulin® on the unborn child are unknown. The effects of chemotherapy (and
other medications you may receive before and after transplant) are not well known. Therefore, women
who are pregnant or breastfeeding cannot be enrolled in this study.
Women of childbearing potential who are enrolled in the study must agree to use an adequate method
of birth control from the time of enrollment until a minimum of one year following transplant.
Men enrolled in this study must agree to use an adequate method of birth control from the time of
enrollment until a minimum of one year following transplant.
It is important that you discuss the implications of discontinuing birth control after one year post
transplant with your transplant doctor. In some cases it may be recommended that pregnancy (or
fathering a child) should be prevented for a longer time period.
Adequate methods of birth control include:
Abstinence
Previous tubal ligation
Vasectomy
Oral, injectable or implantable contraceptives
Condoms
Foam
IUD
If you become pregnant (or father a child) at any time from your enrollment in this study until 2 years
following your transplant (end of study follow-up), then you should inform your transplant doctor and
the study doctor immediately. You will be asked for your permission regarding access to the health
records of your pregnancy (if you are female) as well as the health records of your infant.
WHAT HAPPENS IF THERE IS A CHANGE IN MY ELIGIBILITY FOR THE STUDY AFTER I HAVE BEEN
RANDOMIZED?
Page 78 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
It is possible that your health status may change after you are randomized such that you no longer meet
the eligibility for the study.
In some cases, your doctor will recommend that your transplant is postponed until your health is
optimal for transplant again. For example, if you require treatment for an infection, your transplant
might be postponed until the infection has resolved. In this situation, you can still fully participate in the
study as long as your situation changes so that once again you meet all the study eligibility criteria prior
to the rescheduled transplant.
In some cases, it is possible that your doctor may decide it is in your best interest to proceed with the
transplant as scheduled; However, the changes in your health status may be such that you no longer
meet all the eligibility criteria. This would affect your participation in the following way:
If you have been randomized to the “Thymoglobulin® Group”, you would no longer be able to
receive Thymoglobulin®
The researchers will follow your progress for up to 2 years following the date of randomization
The researchers will continue to collect the study data as originally planned
You will be asked to complete the study questionnaires as originally planned
In very rare cases, a transplant may need to be cancelled. In this situation, the researchers will continue
to follow your progress for up to 2 years from the date of your randomization.
IF I DO NOT WANT TO TAKE PART IN THE STUDY, ARE THERE OTHER CHOICES?
If you do not want to take part in this study it will not affect the decision to have the transplant.
Choosing not to participate in this study will in no way affect your care or treatment.
DECLARATION OF FINANCIAL INTEREST
Neither the Investigator nor the institution has a financial interest or a proprietary interest in the drug,
procedure or device under study.
RESEARCH-RELATED INJURY
If you become ill or injured as a direct result of participating in this study, necessary medical treatment
will be available at no additional cost to you.
Your signature on this form only indicates that you have understood to your satisfaction the information
regarding your participation in the study and agree to participate. In no way does this waive your legal
rights nor release the investigator, the research doctor, the study sponsor or involved institutions from
their legal and professional responsibilities.
WITHDRAWAL FROM THE STUDY
If you choose to participate and later decide to change your mind, you can say no and stop the research
at any time. A decision to withdraw from the study will not affect your health care. Your physician or the
study sponsor may stop your participation at any time, without your consent, if they feel it is in your
Page 79 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
best interest. You may be taken out of the study, if you do not follow your doctor’s instructions, if you
experience a side effect that needs medical treatment, or if the sponsor stops the study for any reason.
COMPENSATION
No costs will be charged to you for being in this study, nor will you be paid for participating in the study.
You will not be charged for the research drugs or any research procedures.
CONFIDENTIALITY
You will not be identified as a study participant in any reports or publications of this research. Your
records will be kept in a locked file cabinet in a locked room. Only the staff involved in the research
study will see them. The research records will also be sent to the national study coordinator who is at
the British Columbia Cancer Agency, but your name will be removed beforehand.
With your permission, your family doctor will also be informed of your participation in this research
study. This consent form will be placed in your Health Chart.
It is unlikely, though possible, that records could be inspected by representatives from the Canadian
Institute of Health Research, the Health Canada agency that funded this research, or Genzyme who
funded part of this research, or the ethics committee at this hospital.
WITHDRAWAL FROM THE STUDY
If you choose to participate and later decide to change your mind, you can say no and stop the research
at any time. A decision to stop being in the study will not affect your health care. Your physician or the
study sponsor may stop your participation at any time, without your consent, if they feel it is in your
best interest. You may be taken out of the study, if you do not follow your doctor’s instructions, if you
experience a side effect that needs medical treatment, or if the sponsor stops the study for any reason.
OTHER PERTINENT INFORMATION
Throughout the research study, you will be told about any new information that might affect your
decision about being in this research study. In particular, you will be told of any unforeseen risks that
may be identified.
WHOM DO I CALL IF I HAVE QUESTIONS OR PROBLEMS?
You should ask questions about anything that you do not understand before you sign this form. The
study staff will also be available to answer questions before, during, and after the study.
If you have questions about taking part in this study, or suffer a research related injury, you can talk to
your doctor. You can also meet with the research nurse who discussed the project with you. You can
also meet with the doctor who is in charge of the study at this institution. That person is:
{Enter Name of Site PI}
{Enter telephone number of Site PI}
Page 80 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Or, you can speak with {{Enter the name and telephone number for an independent research contact
for the institution}. You will receive a copy of this signed and dated consent form.
Page 81 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
SIGNATURE PAGE:
PARTICIPANT:
I have read the preceding information thoroughly. I have had an opportunity to ask questions and all of
my questions have been answered to my satisfaction. I agree to participate in this study. I understand
that I will receive a signed copy of this form.
Name
Signature
Date
Person obtaining consent (Investigator or Delegate):
I have discussed this study in detail with the participant and the parent(s)/guardian(s) of the participant.
I believe the participant understand what is involved in this study to the extent that he/she is able to
understand it. I am satisfied that all questions have been answered, and that the child assents to
participating in the research. In my judgment, this participant has the capacity to give consent, and has
done so voluntarily.
Name, Role in Study
Signature
Date
Witness: (required if participants are unable to read, or if translation is necessary)
I was present when the information in this form was explained and discussed with the participant. I
believe the participant understands what is involved in this study.
Name
Signature
Date
This study has been reviewed by {Insert name of REB}. The REB is responsible for ensuring that
participants are informed of the risks associated with the research, and that participants are free to
decide if participation is right for them. If you have any questions about your rights as a research
participant, please call {Insert the contact information for the representative of the REB}.
It is possible the researchers may be interested in following your health status after the 2 year followup period for this study. Do you agree that you can be contacted in the future regarding extended
follow-up? If yes, please initial _________.
Page 82 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
ASSENT OF PARTICIPANT:
I have had the opportunity to read this consent form, to ask questions about my participation in this
research, and to discuss my participation with my parent(s)/guardian(s). All my questions have been
answered. I understand that I may withdraw from this research at any time, and that this will not
interfere with the availability to me of other health care. I have received a copy of the consent form. I
assent (agree) to participate in this study.
Name
Signature
Date
PARENT / GUARDIAN:
I am satisfied that the information contained in this consent form was explained to my child / ward to
the extent that he/she is able to understand it, that all questions have been answered, and that my child
/ ward assents to participate in this research.
Name
Signature
Page 83 of 112
Date
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Appendix 2 - Karnofsky Functional Scale73
100% - normal, no complaints, no signs of disease
90% - capable of normal activity, few symptoms or signs of disease
80% - normal activity with some difficulty, some symptoms or signs
70% - caring for self, not capable of normal activity or work
60% - requiring some help, can take care of most personal requirements
50% - requires help often, requires frequent medical care
40% - disabled, requires special care and help
30% - severely disabled, hospital admission indicated but no risk of death
20% - very ill, urgently requiring admission, requires supportive measures or treatment
10% - moribund, rapidly progressive fatal disease processes
0% - death.
Page 84 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Appendix 3 – Schedule of Events
Schedule of Events (Day -60 to Day +11)
Study Procedures
Consent1
Randomization2
History and Physical
Weight
Height
Karnofsky Performance Status
CBC, diff
Co-Morbidity Index
Chemistry3
Blood Group
Antibody Screen
Infectious Disease Markers4
EBV by PCR or QPCR5
Beta-HCG (females)6
MUGA/Echocardiogram7
Pulmonary Evaluation8
Renal Evaluation9
BM Biopsy
Preparative Regimen
Day -60 up to start of
preparative regimen
X
X
X
X
X
X
X
X
X
X
X
X
X
Day
-7
Day
-6
Day
-5
Day
-4
Day
-3
Day
-2
Day
-1
Day
0
Day
1
Day
3
Day
6
Day
11
Frequency according to institutional practice
EBV monitoring begins on
day 05
X
X
X
X
X
Thymoglobulin® (ARM B)
Direct bili & serum creatinine10
Bearman Scale (Mucositis)10
Hospitalizations
According to regimen
X
X
X
X
X
X
X
X
X
All hospitalizations to be recorded from start of preparative regimen until
Month 24
Questionnaires
Bradburn
X
CES-D
X
Illness Intrusiveness Scale
X
FACT-BMT
X
EQ-5D
X
Socio-demographics
X
Societal Cost Questionnaire
X
Not
done
at
screening
Health Care Questionnaire
See next page for footnotes:
Page 85 of 112
X
X
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Schedule of Events (Day -60 to Day +11)
Footnotes:
1Consent
must be signed prior to completion of questionnaires and randomization (minimization);
however, the remaining screening evaluations are standard of care. Results dated prior to date of
signing of consent can be used for screening purposes, as long as the evaluations are completed
within the time period specified in the protocol (Day -60 up to start of preparative regimen).
2Randomization to occur no earlier than 21 days prior to planned date of HPCT and no later than 1
day prior to start of the preparative regimen
3Chemistry includes: creatinine, total bilirubin, AST, ALT, ALP.
4Infectious disease markers include: CMV antibody, Hepatitis B surface antigen, total antibody to
Hepatitis B core antigen, Hepatitis C antibody, HIV-1 and HIV-2 antibodies, HTLV-1 and HTLV-2
antibodies, VDRL or equivalent testing for syphilis, West Nile virus testing according to institutional
practice), 5EB virus antibodies (VCA-IgG and Epstein Barr nuclear antigen (EBNA). Testing for
infectious disease disease markers must be done within 30 days prior to transplant.
5EBV monitoring is recommended weekly from Day 0 to Day 100 (as institutional resources allow).
6Beta-HCG is to be done in females of child bearing potential.
7Cardiac evaluation with assessment of ejection fraction by radionucleotide scan or echocardiogram.
8Pulmonary evaluation with spirometry (FEV1) and diffusing capacity (DLCO) or equivalent method
approved by Study Chair.
9Renal evaluation with 24 hour urine for measured creatinine clearance OR serum calculated GFR.
10Myeloablative HPCT participants only
Page 86 of 112
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Schedule of Events (Day +12 to Month 24)
Study Procedures
CBC and differential
Lymphocyte count
Absolute CD4 and CD8 T cell count1
IgG, IgA and IgM
Absolute eosinophil count
Lymphoid & myeloid chimerism2
Chronic GVHD Assessment Form 3
Karnofsky Performance Status
Weight
EBV by PCR or QPCR4
CMV Monitoring5
Immunosuppresive Therapy
Hospitalizations
Questionnaires
Bradburn
CES-D
Day 25
Day 30
X
X
Day 50
Day 60
Day 75
Day 100
Mo 6
Mo 12
X
X
X
X
X
X
X
X
X
X
Frequency according to institutional practice
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
All hospitalizations to be recorded from start of preparative regimen until Month 2
Illness Intrusiveness Scale
FACT-BMT
EQ-5D
Societal Cost Questionnaire
Health Care Questionnaire
Patient cGVHD Severity Scoring Table6
X
X
X
1Absolute
CD4 and CD8 T cell counts if available at the institution.
and myeloid chimerism if available at the institution. (Can be reported as a combined result if this
is the usual practice at the institution.)
3Appendix 9: Chronic GVHD Assessment Form. This form should also be completed at the time a
diagnosis of chronic GVHD is made and at Day 100, Month 6, Month 12 and Month 24.
4EBV monitoring is recommended weekly from Day 0 to Day 100 (as institutional resources allow).
5Duration and frequency of CMV monitoring is according to institutional practice.
6
The Patient cGVHD Severity Scoring Table should be completed at the time a diagnosis of chronic GVHD is
made and at Day 100, Month 6, Month 12 and Month 24.
2Lymphoid
Page 87 of 112
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
Thymoglobulin® to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Appendix 4
Registration and Randomization (Minimization) Form
Confirmation of Eligibility / Change in Eligibility Form
SECTION 1: REGISTRATION & ASSESSMENT OF ELIGIBILITY
Fax completed form to CBMTG 0801 Project Management Office at: 604-875-5584
1.1 Participant Screening Number (assigned by the site): |__|__|__|__|
1.2 Alphanumeric Code (assigned by the Project Management Office): |__|__|__|__|__|__|
1.3 Participant’s Date of Birth: |__|__||__|__|__| |__|__|__|__|
DD
MMM
1.4 Participating Centre (please circle one):
Vancouver – VGH
London – LHS
Ottawa – OH
Quebec City - EJ
Montreal – HMR
Quebec City – HD
YYYY
Toronto – PMH
Winnipeg – CCMB
Montreal – McGill
Halifax – QEII
Hamilton – HHS
1.5 Assessment of Eligibility: (Tick all boxes that apply.)
Participant must:
Be between 16 and 70 years old
Have a hematologic malignancy as
follows:
- Acute leukemia, myeloid, lymphoid, or biphenotypic, in 1st or 2nd remission or be in early
relapse (no chemotherapy within three months and blasts <10% and with previous remission
having been longer than 3 months)
- Chronic myeloid leukemia, in chronic or stable accelerated phase
- Chronic lymphocytic leukemia
- Lymphoma
- Myelodysplastic syndrome
- Myeloproliferative disorder
Page 88 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
- Other
Be
scheduled to receive an unrelated donor hematopoietic progenitor cell transplant
receiving a preparative regimen approved by the clinical study chair
Have an unrelated donor who with high resolution typing is either fully MHC matched at HLA-A, B, C
and DRB1 with the participant or is 1-antigen or 1–allele mismatched at A, B, C or DRB1 loci
Meet the transplant centre’s criteria for HPCT
Be able to give informed consent
Have a Karnofsky Performance Status of greater or equal to 60%
Not be positive for the HIV antibody
Not have a hypersensitivity to rabbit proteins or Thymoglobulin® pharmaceutical excipients, glycine or
mannitol
Not have an active or chronic infection (i.e. infection requiring oral or IV therapy)
Be
1.6 Does the participant fulfill all of the eligibility criteria?
|__| Yes – Please complete SECTION 2: RANDOMIZATION
|__| No – DO NOT RANDOMIZE
SECTION 2: RANDOMIZATION (MINIMIZATION)
Participant Screening Number (assigned by the site):
|__|__|__|
Alphanumeric Code (assigned by the Project Management Office): |__|__|__|__|__|__|
(Project Management Office to complete)
2.1. Participant Diagnosis (please circle one disease and if applicable one sub type):
Please consult with the Project Manager in situations where it is unclear how to classify the participant’s
disease. This is important for the statistical analysis of the data.
Chronic Myeloid Leukemia (CML)
First Chronic Phase
Second Chronic Phase
Accelerated Phase
Acute Myeloid Leukemia (AML)
First Complete Remission
Second Complete Remission
Acute Lymphoblastic Leukemia (ALL)
First Complete Remission
Second Complete Remission
Myelodysplastic Syndrome (MDS)
Refractory Anemia
Refractory Anemia with Ringed Sideroblasts
Refractory Anemia with Excess Blasts-I
Page 89 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Refractory Anemia with Excess Blasts-II
Chronic Lymphocytic Leukemia (CLL)
Chemotherapy-sensitive disease
Most recent relapse interval > 6 months
Most recent relapse interval < 6 months
Lymphoma
Chemotherapy-sensitive disease
Most recent relapse interval > 6 months
Most recent relapse interval < 6 months
Other
List disease: ______________________
2.2. Is the malignancy “de novo”, “therapy related” or “secondary”?
De novo1
Therapy Related2
Secondary3
1De novo: A hematologic malignancy that has arisen without
2Therapy Related: A hematologic malignancy
(documented) prior history of a previous neoplasm/leukemia.
preceded by another cancer that was treated with chemotherapy and/or
radiation
3Secondary: AML preceded by MDS or other hematologic malignancy.
Page 90 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Participant Screening Number (assigned by the site):
|__|__|__|__|
Alphanumeric Code (assigned by the Project Management Office): |__|__|__|__|__|__|
SECTION 2: RANDOMIZATION (continued)
Participant Disease Stage (Early, Late or Other)
Please identify whether the patient has “early stage disease”, “late stage disease” or “other”:
Early Stage Disease: First chronic phase CML, de novo AML in first remission, de novo ALL in first remission,
refractory anemia, refractory anemia with ringed sideroblasts only, CLL and lymphoma with chemotherapysensitive disease OR most recent relapse free interval greater than six months.
Late Stage Disease: Accelerated phase CML, second chronic phase CML, secondary AML in first remission,
therapy-related AML in first remission, AML in second remission, therapy related ALL in first remission, ALL in
second remission, refractory anemia with excess blasts-I, refractory anemia with excess blasts-II, CLL and
lymphoma with disease that is not considered chemotherapy-sensitive OR most recent relapse interval is 6
months or less.
Other: Diagnoses not listed in the “early” or “late” categories.
2.3. Participant has (please circle one only):
Early Stage Disease
Late Stage Disease
Other
2.4. Gender match (circle one):
Female donor-male recipient
Other
2.5. The preparative regimen is (circle one only):
Myeloablative
Non-myeloablative (RIC)
2.6. Has the planned preparative regimen been submitted to the Project Management Office and approved
by the Study Chair?
Yes
No
2.7. Please circle all agents that will be used for GVHD prophylaxis:
Cyclosporine
Tacrolimus
Methotrexate
Mycophenolic acid
Other: ____________________
Page 91 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 4, 15-Jan-2011
Participant Screening Number (assigned by the site):
|__|__|__|__|
Alphanumeric Code (assigned by the Project Management Office): |__|__|__|__|__|__|
SECTION 2: RANDOMIZATION (continued)
2.8.
Enter participant age (circle one):
16-30
31-50
Greater than 50
2.9. The progenitor cell source is (circle one only):
Peripheral Blood Progenitor Cells
Bone Marrow
2.10. Indicate HLA match (circle one):
Full match
(8/8 at HLA A, B, C & DRB1)
One antigen/allele mismatch
(7/8 at HLA A, B, C & DRB1)
2.11. Date participant signed informed consent:
|__|__| |__|__|__| |__|__|__|__|
DD
MMM
YYYY
2.12. Planned start date of preparative regimen: |__|__| |__|__|__| |__|__|__|__|
DD
2.13. Planned HPCT date:
YYYY
|__|__| |__|__|__| |__|__|__|__|
DD
2.14.
MMM
MMM
YYYY
I verify that this participant meets the eligibility criteria for this study and all other patient information
(pages 1- 3) is correct.
______________________________ _______________________________ __________________________
Investigator’s Signature
Investigator’s Printed Name
Date
To be completed by the Project Management Office:
2.15. Date of Randomization:
|__|__| |__|__|__| |__|__|__|__|
DD
MMM
YYYY
2.16. Treatment Arm Assigned:
Arm A - NO Thymoglobulin®
Arm B - Thymoglobulin®
___________________________________________
(Project Manager or delegate to sign)
SECTION 1A: CONFIRMATION OF ELIGIBILITY or CHANGE IN ELIGIBILITY
Complete this form:
When it is certain a delayed transplant is going ahead, but no sooner than 21 days prior to the
revised planned date of transplant, OR
Page 92 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
When it is certain the transplant has been cancelled, OR
When it is certain the participant no longer meets the eligibility criteria, but the transplant is still
scheduled to proceed.
Fax completed form to CBMTG 0801 Project Management Office at: 604-875-5584.
1.1A. Alphanumeric Code: |__|__|__|__|__|__|
1.2A. Participant’s Date of Birth: |__|__||__|__|__| |__|__|__|__|
DD
MMM
1.3A. Participating Centre (please circle one):
Vancouver – VGH
London – LHS
Ottawa – OH
Quebec City - EJ
Montreal – HMR
Quebec City – HD
YYYY
Toronto – PMH
Winnipeg – CCMB
Montreal – McGill
Halifax – QEII
Hamilton – HHS
1.4A. Assessment of Eligibility: (Tick all boxes that apply.)
Participant must:
Be between 16 and 70 years old
Have a hematologic malignancy as
follows:
- Acute leukemia, myeloid, lymphoid, or biphenotypic, in 1st or 2nd remission or be in
early relapse (no chemotherapy within three months and blasts <10% and with
previous remission having been longer than 3 months)
- Chronic myeloid leukemia, in chronic or stable accelerated phase
- Chronic lymphocytic leukemia
- Lymphoma
- Myelodysplastic syndrome
- Myeloproliferative disorder
- Other
Be scheduled to receive an unrelated donor hematopoietic progenitor cell transplant
Be receiving a preparative regimen approved by the clinical study chair
Have an unrelated donor who with high resolution typing is either fully MHC matched at HLAA, B, C and DRB1 with the participant or is 1-antigen or 1–allele mismatched at A, B, C or DRB1
loci
Meet the transplant centre’s criteria for HPCT
Be able to give informed consent
Have a Karnofsky Performance Status of greater or equal to 60%
Not be positive for the HIV antibody
Not have a hypersensitivity to rabbit proteins or Thymoglobulin® pharmaceutical excipients,
glycine or mannitol
Not have an active or chronic infection (i.e. infection requiring oral or IV therapy)
1.5A. Does the participant fulfill all of the eligibility criteria?
|__| Yes
|__| No
Alphanumeric Code: |__|__|__|__|__|__|
SECTION 1A: CONFIRMATION OF ELIGIBILITY or CHANGE IN ELIGIBILITY
Page 93 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
1.6A. Disease Stage (circle one only):
Early
1.7A. The preparative regimen is (circle one only):
Myeloablative
Late
Non-myeloablative (RIC)
Not Applicable (HPCT cancelled)
Site Investigator to Complete EITHER Box 1 or Box 2:
1.8A.
I verify that this participant meets the eligibility criteria for this study.
All participant information (pages 1- 2) is correct.
______________________________ _______________________________ __________________________
Investigator’s Signature
Investigator’s Printed Name
Date
1.9A.
I verify that this participant no longer meets the eligibility for this study.
All participant information (pages 1- 2) is correct.
______________________________ _______________________________ __________________________
Investigator’s Signature
Investigator’s Printed Name
Date
1.10A.
Original planned date of transplant: |__|__||__|__|__| |__|__|__|__|
DD
1.11A.
MMM
YYYY
Reason for delay/cancellation: ____________________________
N/A
1.12A. Is HPCT proceeding even though patient is now ineligible? If yes, provide an explanation:
_____________________________________________________________________________________
1.13A. New date of transplant: |__|__||__|__|__| |__|__|__|__|
DD
MMM
N/A (HPCT cancelled)
YYYY
1.14A. New start date of preparative regimen:
||__|__||__|__|__| |__|__|__|__|
DD
MMM
N/A (HPCT cancelled)
YYYY
To be completed by the Project Management Office:
1.15A. Response from Project Management Office:
__________________________________________________________________________________
_________________________________________
Signature of Project Manager (or delegate)
Page 94 of 112
_______________________________
Date
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
Appendix 5 - Suggested Orders for Administration of Thymoglobulin® 14
1. Rabbit anti-human immunoglobulin, (Thymoglobulin®, ATG) 0.5 mg/kg (actual body weight)
=__________mg, IVPB (IV Piggy Back) over 4-6 hours on _____________(day -2).
Provided in 500 mL NS. Pre-medication required, please see below.
2. Rabbit anti-human immunoglobulin, (Thymoglobulin®, ATG) 2.0 mg/kg (actual body weight)
=__________mg, IVPB (IV Piggy Back) over 4-6 hours on _____________ and
_____________(days -1 and Day +114).
Provided in 500 mL NS. Pre-medication required, please see below.
3. Premedications for each infusion of Thymoglobulin®
a. acetaminophen 1000 mg PO DAILY pre-ATG infusion
b. diphenhydramine 50 mg IVPB DAILY pre-ATG infusion
c. methylprednisolone sodium succinate 40 mg IVPB q12h x 6 doses; give first dose preATG infusion
4. Meperidine 25-50 mg IVPB q4h PRN for rigors with ATG-infusion
14
Courtesy of Dr James Russell, Director, Alberta Blood & Marrow Transplant Program, Tom Baker Cancer Centre.
Please Note: The final dose of Thymoglobulin is given on day 0 at the Tom Baker Cancer Centre; however, in
the CBMTG 0801 trial, the final dose will be given on day +1.
Page 95 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
Appendix 6 - Regimen Related Toxicity: Bearman74 Toxicity Scale
Criteria Stomatitis (Mucositis)
Stomatitis
Toxicity
Grade I
Grade II
Grade III
Pain and/or
ulceration not
requiring a
continuous IV
narcotic drug
Pain and/or ulceration
requiring a continuous IV
narcotic (morphine drip)
Page 96 of 112
Severe ulceration and/or
mucositis requiring preventative
intubation
Severe ulceration – resulting in
documented aspiration
pneumonia with or without
intubation
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
Appendix 7 - Acute Graft Versus Host Disease Staging and Grading40
Step 1: Perform staging of individual organ systems for acute GVHD
a.
Skin Stage:
+1
Maculopapular eruption involving less than 25% of the body surface
+2
Maculopapular eruption involving 25%-50% of the body surface
+3
Maculopapular rash > 50% of the body surface
+4
Generalized erythoderma with bullous formation and often with desquamation
b.
Liver Stage*
+1
Bilirubin 35-50 µmol/L
+2
Bilirubin 51-100 µmol/L
+3
Bilirubin 101-255 µmol/L
+4
Bilirubin > 255 µmol/L
*If patient has documented GVHD of the liver and documented alternative cause of
hyperbilirubinemia (i.e. veno-occlusive disease) then downstage liver GVHD by 1 stage
c.
Gut Stage**
Severity is categorized according to volume of diarrhea (average of two consecutive days) or
the presence of nausea/vomiting
+1
Diarrhea volume = 500-900 mL/day or persistent nausea (+ vomiting) with
histological proof of GVHD within the gut
+2
Diarrhea volume = 1000-1500 mL/day
+3
Diarrhea volume > 1500 mL/day
+4
Severe abdominal pain or ileus
**If patient has documented GVHD of the gut and alternative cause of diarrhea (i.e. severe
mucositis, CMV enteritis, or C.difficile infection), then downstage gut by 1 stage
Step 2: Add organ staging together to determine overall clinical grade.
Clinical Grading of Severity of Acute Graft-Versus-Host Disease
GRADE
SKIN
LIVER
GUT
0 (none)
0
0
0
I (mild)
+1 to +2
0
0
II (moderate)
0 to +3*
+1 and/or
+1
III (severe)
-
+2 to +3
and/or
+2
to
+4
IV (life
+4
+4
threatening)**
*Skin stage 3 alone is also considered overall grade II
**Severe decrease in performance status due to GVHD should be
considered grade IV irrespective of the organ stages
Page 97 of 112
-
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
Appendix 8 - Sullivan1, 2 Criteria
1. Shulman HM, Sullivan KM, Weiden PL, et al. Chronic graft-versus-host syndrome in man: A long-term
clinicopathologic study of 20 seattle patients. Am J Med. 1980;69:204-217.
2. Sullivan KM. Graft-versus-host-disease. In: Thomas ED, Blume KG and Forman SJ, eds. Hematopoietic
Cell Transplantation. Boston, MA: Blackwell Science; 1999:515-536.
Limited Chronic GVHD
Either or both:
1.
Localized skin involvement
2.
Hepatic dysfunction
Extensive Chronic GVHD
Either:
1.
Generalized skin involvement or
2.
Generalized skin involvement and/or hepatic dysfunction plus
i.
Liver histology showing aggressive hepatitis, bridging necrosis or cirrhosis
or
ii.
Involvement of eye: Schirmer’s test with <5 mm wetting
or
iii.
Involvement of minor salivary glands or oral mucous demonstrated on labial biopsy
specimen
or
iv.
Involvement of any target organ e.g. esophageal abnormalities, polymyositis
Page 98 of 112
Thymoglobulin to Prevent Chronic Graft versus Host Disease
Study CBMTG 0801
Version 15-Jan-2011
Appendix 9
Chronic GvHD Assessment Form
Following pages
Page 99 of 112
Chronic GVHD Assessment Form
Participant Code: |__|__|__|__|__|__|
Circle Time Point (circle one):
Day 100
Month 6
Month 12
Month 24
Diagnosis of Chronic GVHD
Actual Date of Assessment: |__|__| |__|__|__| |__|__|__|__|
DD
MMM
YYYY
Tick box for each clinical feature that is present
Other information
SKIN
Clinical features:
Diagnositic:
Poikiloderma
Lichen planus-like features
Sclerotic features
Morphea-like features
Distinctive:
Depigmentation
Other:
Ichthyosis
Keratosis pilaris
Hyperpigmentation
Hypopigmentation
Papulsquamous lesions
0 No Symptoms
1
< 18% BSA with disease signs but NO sclerotic features
2 19-50% BSA OR involvement with superficial sclerotic features
“not hidebound” (able to pinch)
3 >50% BSA OR deep sclerotic features “hidebound” (unable to
pinch) OR impaired mobility, ulceration or severe pruritus
Was a biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings: _________________________________________
__________________________________________________
Common:
Erythema (erythroderma)
Pruritis
Maculopapular rash
NAILS
Clinical features:
Diagnostic: (none)
Distinctive:
Longitudinal ridging, splitting or
brittle features
Onycholysis
Pterygium unguis
Nail loss
(usually symmetric; affects most nails)
Other: (none)
Common: (none)
No symptoms
Symptoms present
(Biopsy not applicable)
SCALP AND BODY HAIR
Clinical features:
Diagnostic: (none)
Distinctive:
Date of Onset
No symptoms
Symptoms present
New onset of scarring or
nonscarring scalp alopecia
Scaling
Papulosquamous lesions
Other:
Thinning scalp hair, typically patchy,
coarse or dull
Premature gray hair
Common: (none)
(Biopsy not applicable)
Page 100 of 112
Participant Code: |__|__|__|__|__|__|
Time Point: _________
MOUTH
Clinical features:
0 No symptoms
Diagnostic:
Lichen-type features
Hyperkeratotic plaques
Restriction of mouth
opening from sclerosis
1 Mild symptoms with disease signs but not limiting oral intake
significantly
2 Moderate symptoms with disease signs with partial limitation of
oral intake
Distinctive:
Xerostomia
Mucocele
Mucosal atrophy
Pseudomembranes
Ulcers
3 Severe symptoms with disease signs on examination with major
limitation of oral intake
Was a biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings: ___________________________________________
____________________________________________________
Other: (none)
Common:
Gingivitis
Mucositis
Erythema
Pain
EYES
Clinical features:
0 No symptoms
Diagnostic: (None)
1 Mild dry eye symptoms not affecting ADL (requiring < x per day)
OR asymptomatic signs of keratoconjunctivitis sicca
Distinctive:
New onset dry, gritty, or painful eyes
Cicatricial conjunctivitis
Keratoconjunctivitis sicca
Confluent areas of punctuate keratopathy
2 Moderate dry eye symptoms partially affecting ADL (requiring
drops > 3 x per day or punctual plugs), WITHOUT vision impairment
Other:
Photophobia
Periorbital hyperpigmentation
Blepharitis
(erythema of the eyelids with edema)
3 Severe dry eye symptoms significantly affecting ADL (special
eyeware to relieve pain) OR unable to work because of ocular symptoms
OR loss of vision caused by keratoconjunctivitis sicca
Common: (none)
Was the Schirmer test done? If yes, please complete:
Date of test: ___________________________________
Results of the mean tear test (mm):
> 10
6-10
GENITALIA (Females)
Clinical features:
Date of Onset
<5
0 No symptoms
Diagnostic:
Lichen planus-like features
Vaginal scarring or stenosis
1 Symptomatic with mild signs on exam AND no effect on coitus and
minimal discomfort with gynecologic exam
Distinctive:
Erosions
Fissures
Ulcers
2 Symptomatic with moderate signs on exam AND with mild
dyspareunia or discomfort with gynecologic exam
Other: (none)
Common: (none)
Not examined
3 Contractures WITH advanced signs (stricture, labial agglutination
or severe ulceration) AND severe pain with coitus or inability to insert
vaginal speculum
Was a biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings: ___________________________________________
Not applicable
Page 101 of 112
Participant Code: |__|__|__|__|__|__|
Time Point: _________
GI TRACT
Date of Onset
Clinical features:
Diagnostic:
Esophageal web
Strictures or stenosis in the upper
to mid third of the esophagus
Distinctive: (none)
Other:
Exocrine pancreatic insufficiency
Common:
Anorexia
Nausea
Vomiting
Diarrhea
Weight loss
0 No symptoms
1 Symptoms such as dysphagia, anorexia, nausea, vomiting,
abdominal pain or diarrhea without significant weight loss (< 5%)
2 Symptoms associated with mild to moderate weight loss (5-15%)
3 Symptoms associated with significant weight loss > 15%, requires
nutritional supplement for most calorie needs OR esophageal dilation
Was a biopsy done? If yes, enter date: ___________________
Findings: ___________________________________________
LIVER
Clinical features:
0 Normal LFT
Diagnostic: (none)
1 Elevated Bilirubin, AP, AST or ALT < 2 x ULN
Distinctive: (none)
2 Bilirubin > 3 mg/dl or Bilirubin, enzymes 2-5 x ULN
Other: (none)
Common:
Total bilirubin, alk phos >2x ULN
plus ALT or AST>2x ULN
Test Results (if done)
AST
________ U/L
Alk Phos ________ U/L
Total Bili _________ umol/L
ALT
_________ U/L
LDH
_________ U/L
Date
_____________
_____________
_____________
_____________
_____________
LUNG
Clinical features:
Diagnostic:
Bronchiolitis obliterans diagnosed with lung biopsy
Distinctive:
Bronchiolitis obliterans diagnosed with PFTs and radiology
Other: (none)
Common: (none)
Were PFT’s done? If yes, please complete:
Date of PFT’s: ______________________
DLCO (corrected for Hgb) __________
FEV1 % expected __________
VC % of expected__________
3 Bilirubin or enzymes > 5 x ULN
Was a biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings:____________________________________________
____________________________________________________
0 No symptoms
1 Mild symptoms (shortness of breath after climbing one flight of
steps)
2 Moderate symptoms (shortness of breath after walking on flat
ground)
3 Severe symptoms (shortness of breath at rest; requiring O2)
Was a lung biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings: ____________________________________________
Was a high resolution CT scan of the lungs done? If yes:
Date of scan: ___________________________
Findings: ___________________________________________
Other relevant test results:
Page 102 of 112
Participant Code: |__|__|__|__|__|__|
Time Point: _________
MUSCLE, FASCIA, JOINTS
Clinical features:
0 No symptoms
Date of Onset
1 Mild tightness of arms or legs, normal or mild decreased range of
motion (ROM) AND not affecting ADL
Diagnostic:
Fasciitis, joint stiffness or contractures
secondary to sclerosis
Distinctive:
Myositis or polymyositis
2 Tightness of arms or legs OR joint contractures, erythema thought
due to fascitis, moderate decrease ROM AND mild to moderate limitation
of ADL
Other:
Edema
Muscle cramps
Arthralgia or arthritis
3 Contractures WITH significant decrease of ROM AND significant
limitation of ADL (unable to tie shoes, button shirts, dress self, etc.)
Was a biopsy done? If yes, please complete:
Date of biopsy: _________________________
Findings:_____________________________________________
___________________________________________________
Common: (none)
HEMATOPOIETIC AND IMMUNE
Clinical features:
Diagnostic: (none)
Distinctive: (none)
Other:
Thrombocytopenia
Eosinophilia
Lymphopenia
Hypo or Hyper - gammaglobulinemia
Autoantibodies (AIHA and ITP)
Findings:
Date
WBC (lowest)
________ x109/L __________________
Platelets (lowest)
________ x109/L __________________
Neutrophils (lowest)
________ x109/L __________________
Lymphocytes (lowest) ________ x109/L __________________
Eosinophils (highest)
Common: (none)
________ x109/L __________________
Other indicators, clinical manifestations or complications related to chronic GVHD (check all that apply and assign a
score to its severity (0 – 3) based on its functional impact where applicable (none - 0; mild - 1; moderate - 2; severe - 3)
Esophageal stricture or web ___
Pericardial Effusion ___
Pleural Effusion(s) ___
Ascites (serositis) ___
Nephrotic Syndrome ___
Peripheral Neuropathy ___
Myasthenia Gravis ___
Cardiomyopathy ___
Coronary artery involvement ___
Polymyositis ___
Cardiac conduction defects ___
OTHERS: Specify: ______________________________________________________________________________
WEIGHT: _________________ KG
Page 103 of 112
Participant Code: |__|__|__|__|__|__|
Time Point: _____________________________
Acute Graft Versus Host Disease:
1. Has there been a diagnosis of acute GVHD between the date of the last assessment and today’s date?
Yes
No
2. If yes, circle the maximum grade of acute GVHD (according to Przepiorka Criteria):
None
Grade I
Grade II
Grade III
Grade IV
3. What is the grade of acute GVHD (according the Przepriorka Criteria) at this time point?
None
Grade I
Grade II
Grade III
Grade IV
Karnofsky Performance Status:
100% - normal, no complaints, no signs of disease
90% - capable of normal activity, few symptoms or signs of disease
80% - normal activity with some difficulty, some symptoms or signs
70% - caring for self, not capable of normal activity or work
60% - requiring some help, can take care of most personal requirements
50% - requires help often, requires frequent medical care
40% - disabled, requires special care and help
30% - severely disabled, hospital admission indicated but no risk of death
20% - very ill, urgently requiring admission, requires supportive measures or treatment
10% - moribund, rapidly progressive fatal disease processes
0% - death.
Immunosuppressive Therapy for Treatment of GVHD(list all therapies):
Name of Therapy
Dose
Route
Reason
1.
2.
3.
4.
THE REMAINING ITEMS ARE COMPLETED AT THE TIME OF DIAGNOSIS OF cGVHD ONLY.
Date of onset of first episode of chronic GVHD: |__|__| |__|__|__| |__|__|__|__|
DD
MMM
Not applicable
YYYY
List immunosuppressive therapy at the time of diagnosis of chronic GVHD but prior to start of or increase
in immunosuppressive therapy treat cGVHD
Name of Therapy
Dose
Route
Reason
1.
2.
3.
4.
Date of form completion: |__|__| |__|__|__| |__|__|__|__|
DD
MMM
YYYY
Person completing the form (print name):
Signature:
_________________________________________
________________________________
The data recorded in this form was collected from the following sources:
In-person assessment / interview
Clinic Notes
Telephone interview
Page 104 of 112
Diagnostic Reports
Appendix 10: Definitions and Weighted Scores of Co-Morbidities (HCT-CI)
Sorror M. et al. 1. Blood. 2007;110:4606-4613; 2. Blood. 2005;106:2912-2919; 3. Blood. 2008;111:446-452.
NOTE: Report final score only, not this form. See P.2 for explanation and formula for corrected DLCO.
Name: _________________________
Comorbidities
Arrhythmia
Cardiac
Inflammatory
bowel disease
Diabetes
Cerebrovascular
disease
Psychiatric
disturbance
Hepatic, mild
Obesity
Infection
Rheumatologic
Peptic ulcer
Moderate/severe
renal
Moderate
pulmonary
Prior solid
malignancy
Heart valve
disease
Severe
pulmonary
Moderate/severe
hepatic
Hospital ID #: ____________________
Definitions
HCT-CI
weighted
scores
1
Atrial fibrillation or flutter, sick sinus syndrome, or
ventricular arrhythmias
Coronary artery disease,* congestive heart failure,
myocardial infarction, or EF of ≤50%
Crohn's disease or ulcerative colitis
Patient
Score
1
1
Requiring treatment with insulin or oral hypoglycemic,
but not controlled with diet alone
Transient ischemic attacks or cerebrovascular accident
1
Depression/anxiety requiring psychiatric consult and/or
treatment at the time of HCT
Chronic hepatitis, bilirubin >ULN to 1.5x ULN, or
AST/ALT >ULN to 2.5x ULN
Patients with a BMI of >35 for adults or with BMI-forage percentile of ≥95th percentile for children
Documented infection or fever of unknown etiology
requiring antimicrobial treatment before, during, and
after the start of conditioning regimen
SLE, RA, polymyositis, mixed CTD, and polymyalgia
rheumatica
Requiring treatment
Serum creatinine >2 mg/dL†, on dialysis, or prior to
renal transplantation
*Corrected DLCO and/or FEV1 66%-80% or dyspnea
on slight activity
Treated at any time point in the patient's history,
excluding nonmelanoma skin cancer
Except asymptomatic mitral valve prolapse
1
*Corrected DLCO and/or FEV1 ≤65% or dyspnea at rest
or requiring oxygen
Liver cirrhosis, bilirubin >1.5x ULN, or AST/ALT >2.5x
ULN
3
1
1
1
1
2
2
2
2
3
3
3
Patient Total:
*DLCO may be affected by non-pulmonary factors, particularly smoking (COHb) and anemia. A correction factor for anemia
was used in the development of this index as follows:
Corrected DLCO (Dinakara method) = measured DLCO/(Hb x 0.007). Hb is in G/L.
Completed by: _______________________
Printed Name
_________________________
Signature & Designation
Page 105 of 112
_______________
date (yyyy-mm-dd)
Appendix 10 Page 2: Definitions and Weighted Scores of Co-Morbidities (HCT-CI)
Comments regarding patient suitability:
LEGEND and EXPLANATIONS:
EF indicates ejection fraction; ULN, upper limit of normal; AST, aspartate aminotransferase; ALT,
alanine aminotransferase; BMI, body mass index; SLE, systemic lupus erythematosus; RA,
rheumatoid arthritis; CTD, connective tissue disease; DLCO, diffusion capacity of carbon monoxide;
and FEV1, forced expiratory volume in one second.
*
One or more vessel-coronary artery stenoses, requiring medical treatment, stent, or bypass graft.
†To convert creatinine from milligrams per deciliter to micromoles per liter, multiply milligrams per
deciliter by 88.4
The predictive capacity of the HCT-CI (Table and Figures from Sorror 2005):
Index/comorbidity group Relapse
HR*
HCT-CI
Low = 0
NRM
P HR*
.01
Survival
P
HR*
<.00
<.00
1.0
1.0
1.0
Intermediate = 1 or 2 2.74
3.95
3.68
High >2
7.16
5.60
2.67
P
Page 106 of 112
Appendix 11 - References
1. Mielcarek M, Martin PJ, Leisenring W, et al. Graft-versus-host disease after nonmyeloablative versus
conventional hematopoietic stem cell transplantation. Blood. 2003;102:756-762.
2. Fraser CJ and Scott Baker K. The management and outcome of chronic graft-versus-host disease. Br J
Haematol. 2007;138:131-145.
3. Arora M, Burns LJ, Davies SM, et al. Chronic graft-versus-host disease: a prospective cohort study. Biology of
Blood & Marrow Transplantation. 2003;9:38-45.
4. Fraser C. J, Bhatia S, Ness K, et al. Impact of chronic graft-versus-host disease on the health status of
hematopoietic cell transplantation survivors: a report from the Bone Marrow Transplant Survivor Study.
Blood. 2006;108:2867-2873.
5. Wong F. L, Francisco L, Forman S. J, et al. Chronic Graft vs. Host Disease (cGVHD) Hinders Long-Term
Functional Recovery after Hematopoietic Cell Transplantation. ASH Annual Meeting Abstracts.
2007;110:634.
6. Rizzo J. D, Curtis R. E, Socie G, et al. Solid cancers after allogeneic hematopoietic cell transplantation. Blood.
2009;113:1175-1183.
7. Afessa B, Litzow MR, Tefferi A. Bronchiolitis obliterans and other late onset non-infectious pulmonary
complications in hematopoietic stem cell transplantation. Bone Marrow Transplant. 2001;28:425-434.
8. Rizzo JD, Wingard JR, Tichelli A, et al. Recommended Screening and Preventive Practices for Long-term
Survivors after Hematopoietic Cell Transplantation: Joint Recommendations of the European Group for
Blood and Marrow Transplantation, the Center for International Blood and Marrow Transplant Research,
and the American Society of Blood and Marrow Transplantation. Biology of Blood and Marrow
Transplantation. 2006/2;12:138-151.
9. Couriel D, Carpenter PA, Cutler C, et al. Ancillary Therapy and Supportive Care of Chronic Graft-versus-Host
Disease: National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in
Chronic Graft-versus-Host Disease: V. Ancillary Therapy and Supportive Care Working Group Report. Biology
of Blood and Marrow Transplantation,. 2006;12:375-396.
10. Filipovich AH, Weisdorf D, Pavletic S, et al. National Institutes of Health consensus development project on
criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report.
Biology of Blood & Marrow Transplantation. 2005;11:945-956.
11. Martin PJ, Weisdorf D, Przepiorka D, et al. National Institutes of Health Consensus Development Project on
Criteria for Clinical Trials in Chronic Graft-versus-Host Disease: VI. Design of Clinical Trials Working Group
report. Biology of Blood & Marrow Transplantation. 2006;12:491-505.
12. Pavletic SZ, Martin P, Lee SJ, et al. Measuring Therapeutic Response in Chronic Graft-versus-Host Disease:
National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graftversus-Host Disease: IV. Response Criteria Working Group Report. Biology of Blood and Marrow
Transplantation. 2006/3;12:252-266.
13. Schultz KR, Miklos DB, Fowler D, et al. Toward Biomarkers for Chronic Graft-versus-Host Disease: National
Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graft-versus-
Page 107 of 112
Host Disease: III. Biomarker Working Group Report. Biology of Blood and Marrow Transplantation.
2006/2;12:126-137.
14. Shulman HM, Kleiner D, Lee SJ, et al. Histopathologic Diagnosis of Chronic Graft-versus-Host Disease:
National Institutes of Health Consensus Development Project on Criteria for Clinical Trials in Chronic Graftversus-Host Disease: II. Pathology Working Group Report. Biology of Blood and Marrow Transplantation.
2006/1;12:31-47.
15. Pavletic S and Vogelsang G. National Institutes of Health Consensus Development Project on Criteria for
Clinical Trials in Chronic Graft-versus-Host Disease: Preface to the Series. Biology of Blood and Marrow
Transplantation. 2005/12;11:943-944.
16. Pavletic S and Vogelsand GB. Treatment of High-Risk Chronic GVHD. Biology of Blood and Marrow
Transplantation. 2008;14:1436-1437.
17. Ruiz-Arguelles GJ, Ruiz-Delgado GJ, Moreno-Ford V. Re: Alemtuzumab-Induced Resolution of Pulmonary
Noninfectious Complications in a Patient with Chronic Graft-versus-Host Disease. Biology of Blood and
Marrow Transplantation. 2008;14:1434-1435.
18. Couriel DR. Ancillary and supportive care in chronic graft-versus-host disease. Best Practice & Research
Clinical Haematology. 2008;21:291-307.
19. Flowers M. E. D, Apperley J. F, van Besien K, et al. A multicenter prospective phase 2 randomized study of
extracorporeal photopheresis for treatment of chronic graft-versus-host disease. Blood. 2008;112:26672674.
20. Bacigalupo A, Lamparelli T, Barisione G, et al. Thymoglobulin® Prevents Chronic Graft-versus-Host Disease,
Chronic Lung Dysfunction, and Late Transplant-Related Mortality: Long-Term Follow-Up of a Randomized
Trial in Patients Undergoing Unrelated Donor Transplantation. Biology of Blood & Marrow Transplantation.
2006;12:560-565.
21. Pavletic S. Z, Carter S. L, Kernan N. A, et al. Influence of T-cell depletion on chronic graft-versus-host
disease: results of a multicenter randomized trial in unrelated marrow donor transplantation. Blood.
2005;106:3308-3313.
22. Bacigalupo A, Lamparelli T, Bruzzi P, et al. Antithymocyte globulin for graft-versus-host disease prophylaxis
in transplants from unrelated donors: 2 randomized studies from Gruppo Italiano Trapianti Midollo Osseo
(GITMO). Blood. 2001;98:2942-2947.
23. Finke J, Bethge WA, Schmoor C, et al. Standard graft-versus-host disease prophylaxis with or without antiT-cell globulin in haematopoietic cell transplantation from matched unrelated donors: a randomised,
open-label, multicentre phase 3 trial. Lancet Oncology. 2009;10:855-864.
24. Bredeson CN, Zhang M, Agovi M, et al. Outcomes following HSCT Using Fludarabine, Busulfan, and
Thymoglobulin® : A Matched Comparison to Allogeneic Transplants Conditioned with Busulfan and
Cyclophosphamide. Biology of Blood and Marrow Transplantation,. 2008;14:993-1003.
25. Russell JA, Turner AR, Larratt L, et al. Adult Recipients of Matched Related Donor Blood Cell Transplants
Given Myeloablative Regimens Including Pretransplant Antithymocyte Globulin Have Lower Mortality
Related to Graft-versus-Host Disease: A Matched Pair Analysis. Biology of Blood and Marrow
Transplantation. 2007;13:299-306.
Page 108 of 112
26. Remberger M, Storer B, Ringden O, Anasetti C. Association between pretransplant Thymoglobulin® and
reduced non-relapse mortality rate after marrow transplantation from unrelated donors. Bone Marrow
Transplant. 2002;29:391-397.
27. Finke J, Bethge W. A, Schmoor C, et al. A Randomized Prospective Multicenter Phase III Trial Comparing
Standard GvHD Prophylaxis with Cyclosporine and Methotrexate with Additional Pretransplant ATG
Fresenius (ATG-F) in Allogeneic Stem Cell Transplantation from Matched Unrelated Donors. ASH Annual
Meeting Abstracts. 2008;112:57.
28. van Esser J. W. J, van der Holt B, Meijer E, et al. Epstein-Barr virus (EBV) reactivation is a frequent event
after allogeneic stem cell transplantation (SCT) and quantitatively predicts EBV-lymphoproliferative disease
following T-cell-depleted SCT. Blood. 2001;98:972-978.
29. Dominietto A, Tedone E, Soracco M, et al. et al. Epstein−Barr virus reactivation after allogeneic
hematopoietic stem cell transplant based on molecular monitoring is predictive of lymphoproliferative
disease. Bone Marrow Transplantation. 2004;33:S192.
30. Bacigalupo A. Antilymphocyte/thymocyte globulin for graft versus host disease prophylaxis: efficacy and
side effects. Bone Marrow Transplant. 2005;35:225-231.
31. Bacigalupo A, Lamparelli T, Barisione G, et al. Thymoglobulin® Prevents Chronic Graft-versus-Host Disease,
Chronic Lung Dysfunction, and Late Transplant-Related Mortality: Long-Term Follow-Up of a Randomized
Trial in Patients Undergoing Unrelated Donor Transplantation. Biology of Blood and Marrow
Transplantation. 2006/5;12:560-565.
32. Kalpoe J, van Tol M, Bredius R, et al. Pre-emptive treatment with rituximab efficiently prevents
EBV lymphoproliferative disease (EBV-LPD) in paediatric
allogeneic stem cell recipients. Bone Marrow Transplantation. 2004;33:S192.
33. Slavin S, Nagler A, Naparstek E, et al. Nonmyeloablative Stem Cell Transplantation and Cell Therapy as an
Alternative to Conventional Bone Marrow Transplantation With Lethal Cytoreduction for the Treatment of
Malignant and Nonmalignant Hematologic Diseases. Blood. 1998;91:756-763.
34. McSweeney PA, Niederwieser D, Shizuru JA, et al. Hematopoietic cell transplantation in older patients with
hematologic malignancies: replacing high-dose cytotoxic therapy with graft-versus-tumor effects. Blood.
2001;97:3390-3400.
35. Giralt S, Thall PF, Khouri I, et al. Melphalan and purine analog-containing preparative regimens: reducedintensity conditioning for patients with hematologic malignancies undergoing allogeneic progenitor cell
transplantation. Blood. 2001;97:631-637.
36. Giralt S, Ballen K, Rizzo D, et al. Reduced-intensity conditioning regimen workshop: defining the dose
spectrum. Report of a workshop convened by the center for international blood and marrow transplant
research. Biology of Blood & Marrow Transplantation. 2009;15:367-369.
37. Banna GL, Aversa S, Sileni VC, Favaretto A, Ghiotto C, Monfardini S. Nonmyeloablative allogeneic stem cell
transplantation (NST) after truly nonmyeloablative and reduced intensity conditioning regimens. Critical
Reviews in Oncology-Hematology. 2004;51:171-189.
38. Lazarus HM, Kan F, Tarima S, et al. Rapid transport and infusion of hematopoietic cells is associated with
improved outcome after myeloablative therapy and unrelated donor transplant. Biology of Blood &
Marrow Transplantation. 2009;15:589-596.
Page 109 of 112
39. Dominietto A, Van Lint MT, Gualandi Fea. Is timing of anti-thymocyte globulin (ATG) – pre and post
hemopoietic stem cell transplants (HSCT) – relevant for graft vs host disease (GvHD)?[abstract]. Blood.
2003;102:242a (abstr 851).
40. Przepiorka D, Weisdorf D, Martin P, et al. Consensus conference on acute GVHD grading. Bone Marrow
Transplant. 1995;15:825-828.
41. Sullivan KM, Agura E, Anasetti C, et al. Chronic graft-versus-host disease and other late complications of
bone marrow transplantation. Semin Hematol. 1991;28:250-259.
42. Styczynski J, Reusser P, Einsele H, et al. Management of HSV, VZV and EBV infections in patients with
hematological malignancies and after SCT: guidelines from the Second European Conference on Infections
in Leukemia. Bone Marrow Transplant. 2009;43:757-770.
43. Tomblyn M, Chiller T, Einsele H, et al. Guidelines for Preventing Infectious Complications among
Hematopoietic Cell Transplantation Recipients: A Global Perspective. Biol Blood Marrow Transplant.
2009;15:1143-1238.
44. Bradburn NM and Noll CE. The Structure of Psychological Well-Being. Chicago, Aldine Pub. Co.; 1969.
45. Radloff LS. The CES-D Scale: A Self-Report Depression Scale for Research in the General Population. Applied
Psychological Measurement. 1977;1:385-401.
46. Devins GM. Illness intrusiveness and the psychosocial impact of lifestyle disruptions in chronic lifethreatening disease. Adv Ren Replace Ther. 1994;1:251-263.
47. McQuellon RP, Russell GB, Cella DF, et al. Quality of life measurement in bone marrow transplantation:
development of the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale.
Bone Marrow Transplant. 1997;19:357-368.
48. Devlin N, Hansen P, Herbison P, Macran S. A "new and improved" EQ-5D valuation questionnaire? Results
from a pilot study. European Journal of Health Economics. 2005;6:73-82.
49. McQuellon RP, Russell GB, Rambo TD, et al. Quality of life and psychological distress of bone marrow
transplant recipients: the 'time trajectory' to recovery over the first year. Bone Marrow Transplant.
1998;21:477-486.
50. Cella D. Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System
Version 4. 1997.
51. Lee S, Cook EF, Soiffer R, Antin JH. Development and validation of a scale to measure symptoms of chronic
graft-versus-host disease. Biology of Blood & Marrow Transplantation. 2002;8:444-452.
52. Couban S, Simpson DR, Barnett MJ, et al. A randomized multicenter comparison of bone marrow and
peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood.
2002;100:1525-1531.
53. MacHin D and Campbell MJ. Statistical Tables for the Design of Clinical Studies. WileyBlackwell; 1987.
54. Proschan MA, Lan KKG, Wittes JT eds. Statistical Monitoring of Clinical Trials: A Unified Approach. Springer
New York; 2006:.
55. Carlens S, Ringden O, Remberger M, et al. Risk factors for chronic graft-versus-host disease after bone
marrow transplantation: A retrospective single centre analysis. Bone Marrow Transplant. 1998;22:755-761.
56. Kollman C, Howe C. W. S, Anasetti C, et al. Donor characteristics as risk factors in recipients after
transplantation of bone marrow from unrelated donors: the effect of donor age. Blood. 2001;98:20432051.
Page 110 of 112
57. Flowers ME, Storer BE, Lee SJ, et al. Risk Factors for the Development of Acute and National Institute of
Health (NIH) Chronic Graft-Versus-Host Disease (GVHD). Blood. 2009;114 (abstr 345).
58. Nademanee A, Schmidt G, Parker P, et al. The outcome of matched unrelated donor bone marrow
transplantation in patients with hematologic malignancies using molecular typing for donor selection and
graft-versus-host disease prophylaxis regimen of cyclosporine, methotrexate, and prednisone. Blood.
1995;86:1228-1234.
59. Stem Cell T. Allogeneic Peripheral Blood Stem-Cell Compared With Bone Marrow Transplantation in the
Management of Hematologic Malignancies: An Individual Patient Data Meta-Analysis of Nine Randomized
Trials. J Clin Oncol. 2005;23:5074-5087.
60. Lee S. J, Klein J, Haagenson M, et al. High-resolution donor-recipient HLA matching contributes to the
success of unrelated donor marrow transplantation. Blood. 2007;110:4576-4583.
61. Sullivan KM, Agura E, Anasetti C, et al. Chronic graft-versus-host disease and other late complications of
bone marrow transplantation. Semin Hematol. 1991;28:250-259.
62. Socie G, Loiseau P, Tamouza R, et al. Both genetic and clinical factors predict the development of graftversus-host disease after allogeneic hematopoietic stem cell transplantation. Transplantation.
2001;72:699-706.
63. Sorror M. L, Storer B. E, Maloney D. G, Sandmaier B. M, Martin P. J, Storb R. Outcomes after allogeneic
hematopoietic cell transplantation with nonmyeloablative or myeloablative conditioning regimens for
treatment of lymphoma and chronic lymphocytic leukemia. Blood. 2008;111:446-452.
64. Sorror M. L, Giralt S, Sandmaier B. M, et al. Hematopoietic cell transplantation specific comorbidity index as
an outcome predictor for patients with acute myeloid leukemia in first remission: combined FHCRC and
MDACC experiences. Blood. 2007;110:4606-4613.
65. Sorror M. L, Maris M. B, Storb R, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index:
a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912-2919.
66. Therneau TM. How many stratification factors are "too many" to use in a randomization plan?. Control Clin
Trials. 1993;14:98-108.
67. Moher D, Schulz K. F, Altman D. G, for the CONSORT G. The CONSORT Statement: Revised
Recommendations for Improving the Quality of Reports of Parallel-Group Randomized Trials. Ann Intern
Med. 2001;134:657-662.
68. Altman D. G, Schulz K. F, Moher D, et al. The Revised CONSORT Statement for Reporting Randomized Trials:
Explanation and Elaboration. Ann Intern Med. 2001;134:663-694.
69. Tu D, Shalay K, Pater P. Adjustment of Treatment Effect for Covariates in Clinical Trials: Statistical and
Regulatory Issues. Drug Information Journal. 2000;34:511-523.
70. Kalbfleisch JD and Prentice RL. The Analysis of Failure Time Data. Wiley, New York; 1980.
71. Fairclough DL. Design and Analysis of Quality of Life Studies in Clinical Trials. Quality of Life Research.
2004;13:275-277.
72. Lewis JA. Statistical principles for clinical trials (ICH E9): an introductory note on an international guideline.
Stat Med. 1999;18:1903-1942.
73. Karnofsky DA and Burchenal JH. The Clinical Evaluation of Chemotherapeutic Agents in Cancer. In: MacLeod
CM, ed. Columbia Univ Press.; 1949:196.
74. Bearman SI, Appelbaum FR, Buckner CD, et al. Regimen-related toxicity in patients undergoing bone
marrow transplantation. Journal of Clinical Oncology. 1988;6:1562-1568.
Page 111 of 112
75. Shulman HM, Sullivan KM, Weiden PL, et al. Chronic graft-versus-host syndrome in man. A long-term
clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204-217.
76. Greenberg P, Cox C, LeBeau MM, et al. International scoring system for evaluating prognosis in
myelodysplastic syndromes. Blood. 1997;89:2079-2088.
77. Malcovati L, Germing U, Kuendgen A, et al. Time-dependent prognostic scoring system for predicting
survival and leukemic evolution in myelodysplastic syndromes. Journal of Clinical Oncology. 2007;25:35033510.
78 Ugarte-Torres A, Hoegh-Petersen M, Liu Y, et al. Donor Serostatus Impacts Cytomegalovirus-Specific
Immunity, Cytomegaloviral Disease Incidence, and Survival in Seropositive Hematopoietic Cell Transplant
Recipients
79 Bacigalupo A, Lamparelli T, Milone G, Sormani MP, Ciceri F, Peccatori J, et al. Pre-emptive treatment of
acute GVHD: a randomized multicenter trial of rabbit anti-thymocyte globulin, given on day +7 after
alternative donor transplants. Bone Marrow Transplantation 45(2): 385-91, 2010 Feb.
80 Antin J, Childs R, Filipovich, A, Giralt S, Mackinnon S, Spitzer T, Weisdorf D. Establishment of Complete and
Mixed Donor Chimerism After Allogeneic Lymphohematopoietic Transplantation: Recommendations From
a Workshop at the 2001 Tandem Meetings. Biology of Blood and Marrow Transplantation. 2001; 7:473485.
81 Vardiman J, Thiele J, Arber D, Brunning R, et al. Perspective: The 2008 revision of the World Health
Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important
changes. Blood. 2009; 5: 937-951.
82 Chen W, Wang E, Lu Y, Gaal K, et al. Therapy-Related Acute Lymphoblastic Leukemia Without 11q23
Abnormality Report of Six Cases and a Literture Review. American Journal for Clinical Pathology. 2010;
133: 75-82.
83 Litzow MR, Tarima S, Pérez WS, Bolwell BJ, Cairo MS, et al. Allogeneic transplantation for therapy related
myelodysplastic syndrome and acute myeloid leukemia. Blood. 2010; 115: 1850-1857.
Page 112 of 112