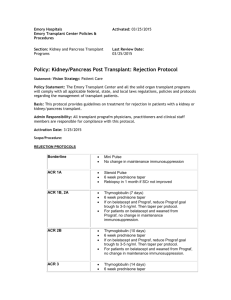
ATGAM

THYMOGLOBULIN (Rabbit Anti-Thymocyte Globulin)
POST-HEART TRANSPLANT
Indications
Refractory rejection
Induction therapy if serum creatinine level > 1.8 or an estimated GFR of
<65ml/min (Renal Sparing Protocol)
Induction therapy if pre-transplant PRA levels > 10% or other high risk candidate
(African American or re-transplant)
Plan/Management
Post-operative moderate to severe rejection accompanied by significant hemodynamic compromise/clinical signs or symptoms, or induction therapy for those patients deemed to be high risk.
Laboratory
Prior to first-dose of thymoglobulin therapy and as indicated during thymoglobulin therapy, each patient should receive the following labs as necessary:
CBC with differential & Platelet Count daily during therapy (Monitor for leukopenia &
thrombocytopenia)
CMP, PO
4
, LDH, Magnesium, Uric Acid daily
Flow cytometry for T-cell subsets (immunodeficient/transplant) x 1. During ATG therapy, the T-cell count should fall to < 10 cells/mm
3
.
If female patient, Beta HCG blood x 1 prior to Thymoglobulin.
Endomyocardial biopsy, Right heart catheterization, CXR, Echocardiogram prior to
ATG therapy. These should then be repeated 7-14 days after ATG therapy completed
(Timing at discretion of cardiology and cardiac surgery team).
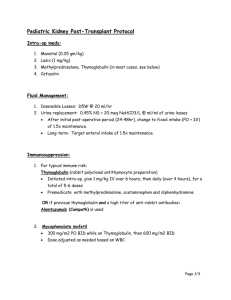
Dose/Administration
Thymoglobulin (rabbit) 1.5 mg/kg IV, (round to the nearest 25 mg) daily for 3-14 days or doses depending on indication:
--INDUCTION: POD #0 (given in the OR), POD#1, and POD#2 (3 total doses)
--REJECTION: Give 7-14 days, based on response
Run via central line using a 0.2 micron inline filter
Saline infusion to run over 6 hours for the first dose & then IF TOLERATED to run over
4 hours for all subsequent doses.
Prior to administering the first three doses of thymoglobulin therapy pre-medication with
Solu-Medrol, Tylenol, and Benedryl is required. See pre-medication specifics below.
No test dose required prior to first dose of Thymoglobulin (rabbit)
Pre-medication
For the first three doses of Thymoglobulin (Rabbit), the following medications should be given 30 minutes prior to administration:
Methylprednisolone per protocol (250mg POD#1, 125mg POD#2)
Acetaminophen 650 mg po/pr, then every 6 hours thereafter for fever as necessary
Diphenhydramine 50 mg IV
Order Bedside Anaphylaxis Emergency Kit – contents listed below for use in suspected anaphylactic reaction to ATG and how to administer
Solucortef 100 mg IV (to be given over 30 seconds)
Epinephrine 1:1000, 3 vials (0.5mg SQ)
Diphenhydramine 50 mg IV (give 25mg over 1 minute)
Albuterol inhaler (give 2 puffs for anaphylaxis)
Three 3cc syringes
Ambu bag, Face Mask and Oral Airway
Anti-infective Prophylaxis
The following prophylaxis should be started at time of tx or during rejection therapy
Nystatin swish and swallow 5 cc po QID
Acyclovir 400mg po every 12 hours (if CMV
Valcyte 900mg daily (if CMV, MODERATE
LOW
or risk category)
HIGH
Bactrim DS 1 tablet twice daily on Monday for PCP px
risk)
Admit to ICU
For the treatment of rejection, patients should be admitted to the ICU for first dose of
Thymoglobulin (rabbit). This is to ensure the patient does not have a reaction to the antibody. The remaining doses may be given on step-down unit or possibly in outpatient setting, once hemodynamic stability achieved and Thymoglobulin (rabbit) therapy is well tolerated by the patient.
Reference:
Thymoglobulin [Package Insert]. Cambridge (MA): Genzyme Corp; 2009.
Revised 6/03/09