CENTRAL NURSERY: STANDING NURSING ORDERS
advertisement
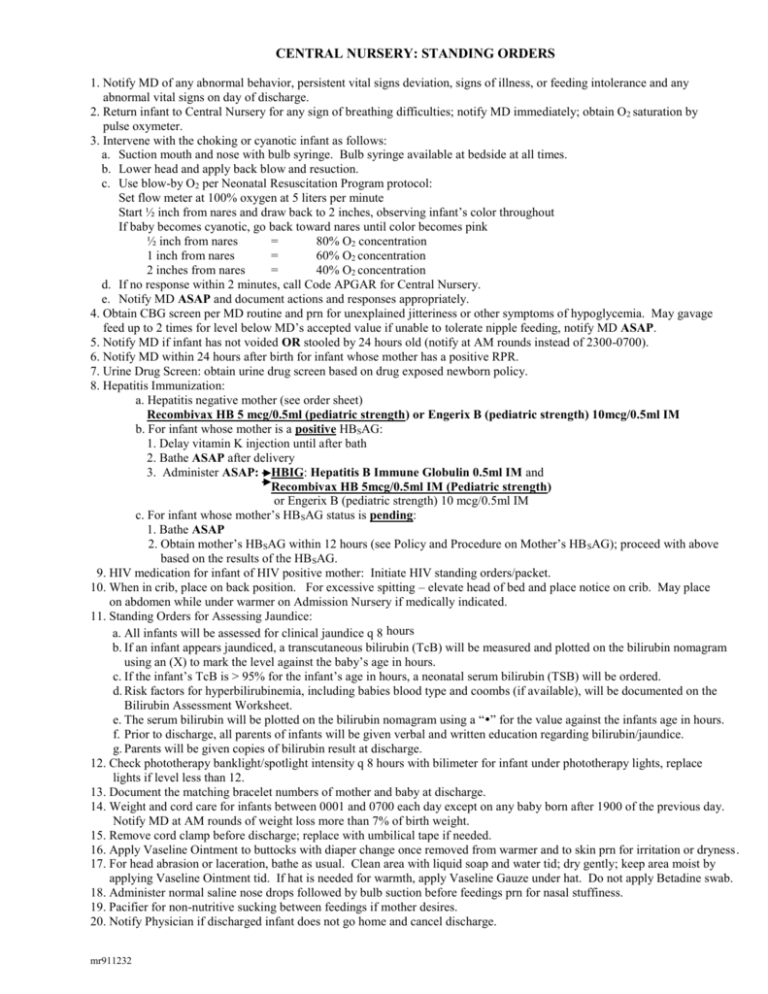
CENTRAL NURSERY: STANDING ORDERS 1. Notify MD of any abnormal behavior, persistent vital signs deviation, signs of illness, or feeding intolerance and any abnormal vital signs on day of discharge. 2. Return infant to Central Nursery for any sign of breathing difficulties; notify MD immediately; obtain O2 saturation by pulse oxymeter. 3. Intervene with the choking or cyanotic infant as follows: a. Suction mouth and nose with bulb syringe. Bulb syringe available at bedside at all times. b. Lower head and apply back blow and resuction. c. Use blow-by O2 per Neonatal Resuscitation Program protocol: Set flow meter at 100% oxygen at 5 liters per minute Start ½ inch from nares and draw back to 2 inches, observing infant’s color throughout If baby becomes cyanotic, go back toward nares until color becomes pink ½ inch from nares = 80% O2 concentration 1 inch from nares = 60% O2 concentration 2 inches from nares = 40% O2 concentration d. If no response within 2 minutes, call Code APGAR for Central Nursery. e. Notify MD ASAP and document actions and responses appropriately. 4. Obtain CBG screen per MD routine and prn for unexplained jitteriness or other symptoms of hypoglycemia. May gavage feed up to 2 times for level below MD’s accepted value if unable to tolerate nipple feeding, notify MD ASAP. 5. Notify MD if infant has not voided OR stooled by 24 hours old (notify at AM rounds instead of 2300-0700). 6. Notify MD within 24 hours after birth for infant whose mother has a positive RPR. 7. Urine Drug Screen: obtain urine drug screen based on drug exposed newborn policy. 8. Hepatitis Immunization: a. Hepatitis negative mother (see order sheet) Recombivax HB 5 mcg/0.5ml (pediatric strength) or Engerix B (pediatric strength) 10mcg/0.5ml IM b. For infant whose mother is a positive HBSAG: 1. Delay vitamin K injection until after bath 2. Bathe ASAP after delivery 3. Administer ASAP: HBIG: Hepatitis B Immune Globulin 0.5ml IM and Recombivax HB 5mcg/0.5ml IM (Pediatric strength) or Engerix B (pediatric strength) 10 mcg/0.5ml IM c. For infant whose mother’s HBSAG status is pending: 1. Bathe ASAP 2. Obtain mother’s HBSAG within 12 hours (see Policy and Procedure on Mother’s HB SAG); proceed with above based on the results of the HBSAG. 9. HIV medication for infant of HIV positive mother: Initiate HIV standing orders/packet. 10. When in crib, place on back position. For excessive spitting – elevate head of bed and place notice on crib. May place on abdomen while under warmer on Admission Nursery if medically indicated. 11. Standing Orders for Assessing Jaundice: a. All infants will be assessed for clinical jaundice q 8 hours b. If an infant appears jaundiced, a transcutaneous bilirubin (TcB) will be measured and plotted on the bilirubin nomagram using an (X) to mark the level against the baby’s age in hours. c. If the infant’s TcB is > 95% for the infant’s age in hours, a neonatal serum bilirubin (TSB) will be ordered. d. Risk factors for hyperbilirubinemia, including babies blood type and coombs (if available), will be documented on the Bilirubin Assessment Worksheet. e. The serum bilirubin will be plotted on the bilirubin nomagram using a “” for the value against the infants age in hours. f. Prior to discharge, all parents of infants will be given verbal and written education regarding bilirubin/jaundice. g. Parents will be given copies of bilirubin result at discharge. 12. Check phototherapy banklight/spotlight intensity q 8 hours with bilimeter for infant under phototherapy lights, replace lights if level less than 12. 13. Document the matching bracelet numbers of mother and baby at discharge. 14. Weight and cord care for infants between 0001 and 0700 each day except on any baby born after 1900 of the previous day. Notify MD at AM rounds of weight loss more than 7% of birth weight. 15. Remove cord clamp before discharge; replace with umbilical tape if needed. 16. Apply Vaseline Ointment to buttocks with diaper change once removed from warmer and to skin prn for irritation or dryness. 17. For head abrasion or laceration, bathe as usual. Clean area with liquid soap and water tid; dry gently; keep area moist by applying Vaseline Ointment tid. If hat is needed for warmth, apply Vaseline Gauze under hat. Do not apply Betadine swab. 18. Administer normal saline nose drops followed by bulb suction before feedings prn for nasal stuffiness. 19. Pacifier for non-nutritive sucking between feedings if mother desires. 20. Notify Physician if discharged infant does not go home and cancel discharge. mr911232