Acute (Fulminant) Liver Failure and Acetaminophen Overdose
advertisement

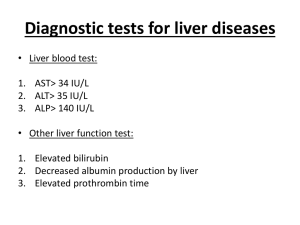
Facilitator Version Module # 15 Acute Liver Failure Created by Jens Langsjoen 4/14 Objectives: 1. 2. 3. 4. Learn the causes of acute liver failure. Recognize the presenting history, exam and lab findings of acute liver failure. Learn the basic work-up and management of acute liver failure. Identify patients who will require urgent transfer to a liver transplant center. CASE 1 60 yo female presents with 2 week history of worsening abdominal discomfort, nausea, lethargy, yellowing of skin, dark urine, and pale stools. What additional history would you like to obtain from this patient? Review of systems: GI: as above, plus reports mild nausea, denies vomiting, denies diarrhea or black/bloody stools HEENT: denies changes in vision or hearing, denies sore throat or headache. Pulmonary: denies shortness of breath or cough Cardiac: denies chest pain or palpatations. Denies syncope Psychiatric: denies any depression. Skin: as above. Otherwise denies rashes or lesions. Neurological: reports a slight occasional tremor for 2 weeks. Musculoskeletal: denies muscle weakness or joint pains Genitourinary: denies pain or difficulty urinating. Heme/lymph: reports easy bruising. Denies bleeding. Allergies: denies any allergic history or seasonal rhinitis. Endocrine: denies hot/cold intolerance Past medical history: patient denies any medical problems in the past other than a history of recurrent UTIs. Medications: Her only prescription medication is nitrofurantoin which she has been taking for years. She reports taking occasional OTC Tylenol but is unsure of the amount. She denies using any herbs/supplements or other over the counter medications. Social history: She reports occasional alcohol use but is vague in quantifying intake, remote history of IVDA. She does not and has never smoked or used recreational drugs; she is a retired high school teacher. She has no recent travel history, she lives with her husband in Albuquerque, and she has 3 healthy children. She denies eating any wild mushrooms. Family history: She reports having an uncle who had “liver problems”. What will you look for on physical exam? Vital signs all within normal limits. General: She is oriented to person and place but not to time. She has slurred speech and seems somewhat confused. Skin: She has significant jaundice and scleral icterus. A two 2-3inch diameter bruises are visible on the upper arms bilaterally. She has no spider angiomata, caput medusa, or temporal wasting. CV/Pulm: within normal limits Abdomen: a tender non-enlarged liver edge, no evidence of ascites, or splenomegaly. Extremities: mild pitting edema of bilateral lower extremities. moves all extremities well. Neuro: She has asterixis of the hands. Otherwise nonfocal and CN II-XII grossly intact. What is your differential based on the results of your history and physical exam? Learners should identify that the patient appears to have acute liver failure based on history and physical exam. The consistent findings include signs of hepatic encephalopathy (asterixis, AMS, slurred speech), and signs of hyperbilirubinemia (jaundice, pale stools, dark urine), and the tender liver. The relative acuity may be deduced based on rapid (2 week) onset, and lack of signs for chronic liver failure (spider angiomata, caput medusa, or temporal wasting). Differential diagnosis list for the acute liver failure should be broad at this point, including viral hepatitis (history of IVDA) (A, B, C, D), Tylenol toxicity (unclear how much she uses), alcoholic hepatitis (she drinks), Wilsons (family history), autoimmune hepatitis (nitrofurantoin is associated with this), other drug/mushroom toxicity, vascular hepatitis (budd chiari, PV thrombosis). What labs/studies would you like to order? Test results show: INR 2.7, AST: 1200, ALT: 1500, TBili: 6.5 (direct: 4, indirect: 2.5), Alk Phos: 227, albumin 2.8, CBC and chem7 wnl, plts 195. negative serological testing for hep A, B, C, negative pregnancy test, negative DS-DNA and AMA. NH3: 97. +Anti-SM ab, +ANA (titer 1:320) Liver US shows unremarkable appearance of liver and biliary system, no CBD dilation, no gallstones. What is the suspected diagnosis, how will you confirm? Nitrofurantoin induced autoimmune hepatitis with acute liver failure is suspected, would need biopsy to confirm. How will you treat the patient? Treating with prednisone is an option for autoimmune hepatitis, however due to the severity of this patient’s liver failure you should probably refer her to a liver transplant center, they can if the patient is accepted for transfer they could initiate a trial of steroids there if urgent transplantation is not immediately required. In the meantime provide supportive care, careful monitoring, nutritional support, treat the encephalopathy with lactulose. How can you better determine if this patient needs a liver transplant? Given that the progression to multi-organ failure can be rapid in patients with acute liver failure, determining their transplantation candidacy quickly is very important. There have been 3 different prognostic evaluation systems developed to help make this determination. Of these 3 scoring systems, the King’s College Criteria has been validated with meta-analyses determining good specificity although limited sensitivity. The scoring systems generally look at presence/absence of encephalopathy, and then Age, coagulopathy, and bilirubin levels. See appendix for specifics of the King’s College Criteria. What other organ system complications is this patient at risk of developing in the setting of acute liver failure? Cardiorespiratory dysfunction Hypotension/decreased effective volume/hypovolemic shock -etiology multifactorial, often combination of fluid losses from vomiting, decreased oral intake, vasodilation from liver failure -for shock treat similar to critically ill hypotensive patients, with initial volume restoration. If a pressor is necessary norepinephrine is preferred with or without vasopressin. Relative adrenal insufficiency: Beware in patients with cardiovascular instability, this can be associated with increased mortality. Respiratory failure: hypercarbic respiratory failure can occur in states of severe hepatic encephalopathy (hepatic coma). Severely encephalopathic patients are at risk of aspirating. Some patients may require intubation if they are not appropriately ventilating or become unable to protect their airway. Pneumonia (infection is a common cause of death in these populations as liver failure progresses). Renal dysfunction Renal dysfunction may occur in more than 50% of patients with acute liver failure. More common in elderly and patients with Tylenol induced liver failure. Associated with increased mortality. Renal replacement therapy may be required in anuric renal failure with fluid overload, for severe acid/base disturbances or severe hyperammonemic states. Neurological conditions Most common and problematic conditions include hepatic encephalopathy and cerebral edema. Hepatic encephalopathy can give a poor prognosis and lead to cerebral edema and coma if not appropriately prevented/treated. Intracranial hypertension from severe cerebral edema is a leading cause of death in acute liver failure. Etiology is thought to be related to systemic and local inflammation and circulatory neurotoxins, especially ammonia. Ampaired detoxification of ammonia in liver failure leads to increased circulation ammonia levels, which is closely correlated to the development of hepatic encephalopathy. Risk of intracranial hypertension is high with sustained ammonia levels of 150200 umol/l. Lactulose or rifaxamin therapy, while a mainstay of therapy for the prevention and treatment of hepatic encephalopathy in chronic or acute on chronic liver failure, may or may not be helpful in patients such as this with true acute liver failure. Mainstays of neurological care include careful monitoring, preventing infections, maintaining and cerebral perfusion. Treatment of cerebral edema can involve ICU level interventions including hypertonic saline, induced hypothermia, sedation, and sometimes intracranial pressure monitoring. What is the prognosis for this patient assuming she progresses to require and receives a liver transplant? What is she most likely to die of? The survival of ALF patients after liver transplantation is on average 79% at 1 year and 72% at 5 years. This patient’s risk of death is likely lower given her young age and lack of any significant comorbidities. Most deaths after liver transplantation occur during the first 3 post-operative months from infection. MKSAP 16 QUESTIONS Gastroenterology and Hepatology 82 (answer D, Wilson’s disease) 71 (answer D, when to refer for liver transplantation) 5 (answer A, Acute viral hepatitis) 91 (answer D, hepatic encephalopathy treatment) Pulmonary and critical care medicine 80 (answer B, Diagnostic paracentesis) Appendix EXTRA CASE CASE 2 A 22 y/o female presents with 3 week history of worsening nausea, occasional non-bloody vomiting, exertional fatigue, decreased appetite, yellowing of her skin and abdominal pain. What is on the differential? This sounds like Acute liver failure (!!!) (refer confused residents to title of module). Differential diagnoses should include viral hepatitis, toxins (mushrooms, TYLENOL), alcoholic hepatitis, autoimmune hepatitis, Wilson’s disease. What further history would you like to know? She works as a waitress. She denies any alcohol or IVDA history, has no tattoos, doesn’t eat or pick wild mushrooms, and has never had a blood transfusion. She has no documented PMH and takes no medications. She doesn’t even take Tylenol, not even ever. She never travels (Hep a, b risk). She doesn’t know her family history, she was adopted (hmm.. suspicious). Her friends tell her she has been talking funny for about a year, that words are out of place and occasionally too loud. She has also noticed that she has felt increasingly paranoid over the past 6 months. What will you look for on exam? Patient’s exam highlights: She appears unwell, slight reproducible RUQ abd pain, dysarthria, jaundice, resting tremor, no asterixis. Kayser Fleischer rings are not obviously visible. What is on the differential now that you have history and physical exam data? Alcoholic, viral, tylenol, or mushroom hepatitis all seem less likely given the history. Autoimmune hepatitis is still a possibility. Wilson’s disease is a possibility especially given the neuro-psychiatric symptoms found in the history (dysarthria, paranoia). What labs/studies do you want to sort out this new differential? Only give those results that are directly asked for by the residents. wbc: 6.5, Hgb: 9, plts: 160,000 MCV: 69, INR: 2.8, AST: 192, ALT: 89, Alk Phos: 22, TBili: 9 (Direct: 1.1), albumin: 3.5, Na: 137, Cr 0.8, BUN: 24, negative pregnancy test, NH3: 20, Hepatitis panel: negative. copper level 207 (nl 70-140), ceruloplasmin level 9 (nl 25-63), LDH: 1001 (nl 115-221), direct/indirect coombs tests: negative. AMA, Anti-SM ab negative. (note: the biliary pattern and LDH consistent with coombs negative hemolytic anemia, the AST/ALT ratio of 2:1, and the subnormal alkaline phosphotase, all concerning for Wilson’s disease!) studies: abdominal US: normal portal vein flow, normal biliary system, normal sized liver. If residents ask for a slit lamp exam, this can be done and will show Kayser Fleischer rings. Why is she anemic? The patient has evidence of hemolytic anemia on laboratory work up. While Total bilirubin elevation can occur from acute liver failure it would not be expected to be all indirect, which raises concerns for hemolysis. The elevated LDH of 1001 is also consistent with hemolysis. Once the residents determine that the patient has hemolytic anemia, they should ask for a direct/indirect coombs test, which is negative. This makes an autoimmune hemolytic anemia unlikely and should raise concern for another cause for hemolysis, in this setting something such as Wilson’s disease. What is the rough likelihood that she has Wilson’s disease? The Germans came up with a scoring system! ●Kayser-Fleischer rings (2 points) ●Neuropsychiatric symptoms suggestive of Wilson disease (2 points) ●Coombs-negative hemolytic anemia with high serum copper (1 point) ●Urinary copper in the absence of acute hepatitis •1 to 2 times the upper limit of normal (1 point) •>2 times the upper limit of normal (2 points) •Normal, but >5 times the upper limit of normal after challenge with two doses of 0.5 g D-penicillamine (2 points) ●Liver copper quantitative measurement •Normal (-1 point) •Up to 5 times the upper limit of normal (1 point) •>5 times the upper limit of normal (2 points) ●Rhodanine positive hepatocytes (if unable to obtain quantitative copper measurement) (1 point) ●Serum ceruloplasmin (based on using a nephelometric assay with a normal value >20 mg/dL) •Normal (0 points) •10 to 20 mg/dL (1 point) •<10 mg/dL (2 points) ●Mutation analysis •Disease causing mutations on both chromosomes (4 points) •Disease causing mutations on one chromosome (1 point) •No diseased causing mutation (0 points) If the score is ≥4, Wilson disease is highly likely; if it is 2 to 3, the diagnosis is probable, but more investigation is warranted (eg, obtaining a liver biopsy if not already done); if it is <2, Wilson disease is unlikely. This patient has a million points so she is very likely to have Wilson’s disease. She probably doesn’t need a liver biopsy to make the diagnosis but you should ask GI anyway. How will you treat this patient? This patient will most likely need a liver transplant. In the meantime you will need to carefully monitor and provide supportive care for her rapidly progressive liver failure and hemolytic anemia. Plasmaphoresis might be helpful (some studies) while awaiting transplantation. For long term management , ask GI, but tell them you are quite interested in chelating her serum copper ASAP with D-Penicillamine at a starting dose of 250mg-500mg/day with a goal of increasing urine copper excretion from a baseline of around 100mcg/day to closer to 2000mcg/day. What dietary recommendations will you give to this patient? You will have to break the news that a few of the world’s most delicious and luxurious high copper foods will now be off limits. These, unfortunately, include the following: shellfish, nuts, chocolate, mushrooms, and organ meats. You can reassure her that if she doesn’t die and is real good and sticks with her chelation therapy she can try some foie gras next year. MKSAP QUESTIONS: King’s College Criteria Can be used as criteria to consider referral to a transplant center Differential for Acute Liver Failure Viral: hepatitis A, B, C, D, E, HSV, CMV, EBV, HVZ, adenovirus, hemorrhagic fever virus Drugs: Idiosyncratic: Halothane, most HIV meds, INH, rifampicin, valproate, NSAID’s, disulfuram, et al. Dose-related: Acetaminophen, sulfonamides, tetracycline, ecstasy, cocaine, meth, statins Toxins: Alcohol, Amanita phylloides, Bacillus cereus toxin, CCl4, yellow phosphorus. Herbs: Chaparral, germander, kava kava, ginseng, comfrey, Vascular: Right heart failure, Budd-Chiari syndrome, portal vein thrombosis, ischemic/hypoperfusion “shock liver”, septic shock, heat stroke. Metabolic: Wilson’s Disease, acute fatty liver of pregnancy, HELLP, Reye’s, adult Stills. Classic Acute Liver Failure Definition Acute liver injury Impaired synthetic function (INR>1.5) Hepatic encephalopathy (poor prognosis if present) Illness duration <26 weeks Presenting Symptoms Fatigue/malaise Nausea/vomiting RUQ pain Pruritis Jaundice Physical exam findings Hepatic encephalopathy o Grade 1: behavior change, mild confusion, slurred speech o Grade 2: lethargy, moderate confusion o Grade 3: Stupor, incoherent, sleeping o Grade 4: coma, unresponsive to pain Asterixis: (in grade 1-3 encephalopathy) Jaundice Vesicular skin lesions, fever (HSV) RUQ pain and hepatomegaly Ascites Orthostasis Lab abnormalities Typical o INR >1.5 o Transaminitis (often marked elevation) o High bilirubin o Low platelets <150,000 Disease specific abnormalities o Tylenol OD Transaminitis >3500, low Tbili, high INR o Ischemic Transaminitis >1000, high LDH o HBV Transaminitis 1000-2000, ALT>AST o Wilsons Transaminitis <2000, Coombs neg hemolytic anemia, AST/ALT ratio >2, normal Alk phos, ARF. o Alcoholic AST/ALT ratio 2:1 Workup: History o Toxins: medications, ETOH, mushrooms, occupational, chupacabra bite. o Ischemia risk factors: hypotension, CHF, hypercoag state, OCP, CA, NMFDS (New Mexico Found Down Syndrome). o Viral risk factors: immunosuppression, chronic HBV, IVDA, travel (A,E) o Family history (wilsons) Labs o Initial workup to consider INR, CBC, chem7, LFTs, Tylenol lvl, tox screen, viral serologies (A, B, C, HSV, VZV, E (if pregnant), pregnancy test, autoimmune (ANA, AMA, ASMA), NH3, lipase, ceruloplasmin. Imaging o Abd US with Doppler (Budd Chiari, Portal HTN, cirrhosis, steatosis) o Consider TTE if concern for ischemic hepatitis o Consider CT or MRI if concern for malignancy Consider Liver biopsy for o Unclear dx, malignant infiltration, autoimmune, wilsons, HSV Management Monitoring o Daily LFTs, INR, CBC, Chem7, Mg, Ph o Beware hypoglycemia, development of HRS, hyponatremia, bleeding, infection o Nutrition o Early nutritional support is vital o Don’t restrict protien o Use oralenteralparenteral as necessary Primum Nocure o Avoid sedating medications, especially narcotics and long acting benzos Disease specific management o Tylenol OD NAC (low threshold for use if suspected OD, especially if transaminitis or elevated Tylenol levels). o Mushroom poisoning: early activated charcoal o HBV: nucleoside analogue antiviral therapy o Acute Budd Chiari: TIPS vs surgical decompression vs thrombolysis o Alcoholic hepatitis: prednisone vs pentoxifyllin if DF>32. o Autoimmune hepatitis: consider prednisone with caution for sepsis Hepatic encephalopathy o Lactulose for 3 BMs/day. Consider Rifaxamin if not tolerating lactulose. Coagulopathy o FFP only if bleeding or prior to procedure. Post Module Evaluation Please place completed evaluation in an interdepartmental mail envelope and address to Dr. Wendy Gerstein, Department of Medicine, VAMC (111) or return to Dr. Patrick Rendon, Division of Hospital Medicine, UNM Hospital. 1) Topic of module:__________________________ 2) On a scale of 1-5, how effective was this module for learning this topic? _________ (1= not effective at all, 5 = extremely effective) 3) Were there any obvious errors, confusing data, or omissions? Please list/comment below: ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 4) Was the attending involved in the teaching of this module? Yes/no (please circle). 5) Please provide any further comments/feedback about this module, or the inpatient curriculum in general: 6) Please circle one: Attending Resident (R2/R3) Intern Medical student