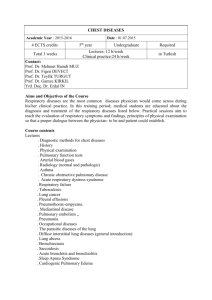
PULMONARY MCQ 2002 PAPER
PULMONARY MCQ 2002 PAPER
Q1 . ANSWER B / E
ANSWER contains info on WG and ANCA testing
-Question is on diagnosis of Wegners granulomatosis ( 2/3 of triad of upper airway disease(sinusitis, recurrent infections), lower airway disease ( pulm heam, hemoptysis), and GN)
Wegener's granulomatosis is a systemic vasculitis of the medium and small arteries, as well as the venules, arterioles, and occasionally large arteries . primarily involves the upper and lower respiratory tracts and the kidneys .
-90 percent of patients with Wegener's granulomatosis have upper or lower respiratory tract disease or both.
- major organs ELKS- Ent( 90%) , Lung, Kidney, Skin and systemically unwell
CXR changes in WG- unilateral (55%), bilateral (45%), infiltrates ( 65%), nodules
31%, infiltrates with cavitation 8%, nodules with cavitation 10%
Heamoptysis
– seen in 98% pts
ENT- nasal septal perforation, saddle nose deformity, sinusitis, rhinnorhea
Positive UA in 80% pts
Lab; Inc ESR rx: steroids + cyclophosphamide, bactrim ( helps prevent relapse)
ANCA-associated small-vessel vasculitis is the most common primary systemic small-vessel vasculitis in adults and includes three major categories: Wegener's granulomatosis , microscopic polyangiitis( kidney and lung) , and Churg –Strauss syndrome( asthma, system eosinophilia)
ANCA - ANCA as 2 stage procedure 1/ immunoflurescence
screening test ( similar to ANA), sensitive( % of pts with disease who have positive test) , 2/
ELISA for MPO PR3 antibodies ( specific- % of pts without disease who have a negative test), ie more specific confirmatory test.
C- ANCA -
ANCA is considered specific and sensitive for systemic WG ( present in gr 90%)
. if c-anca IF pos, 95% will be pr3 positive.
-C- anca spec for WG positive
-C-anca without clinical evidence disease does not establish diagnosis
-c anca can be +ve in other disease- HCV, polyangiitis, UC, RA, endocarditis sulfasalazine
-Good clinical picture + C-ANCA = 90% chance WG.
P-ANCA - positive in other vasculitis( polyangiitis, cutaneous vasculitis, small vx vasculitis)
P-Anca with spec for MPO small vx vasculitis.
UP TO DATE -ANCA antibodies — The diagnosis of WG is suggested from the clinical and laboratory findings and from the presence of circulating antineutrophil cytoplasmic antibodies (ANCA) that are usually directed against proteinase 3 (C-
ANCA).
Nearly all patients with active systemic Wegener's granulomatosis have a positive ANCA (range of 65 to over 90 percent)
- ANCA alone, including C-ANCA which is more specific for Wegener's granulomatosis, does not appear to be sufficiently accurate to make or exclude the diagnosis. As an example, the sensitivity of the C-ANCA may be as low as 65 to 70 percent in patients with limited WG( resp tract only) or inactive disease.
HARRISONS- The diagnosis of Wegener's granulomatosis is a clinicopathologic one made by the demonstration of necrotizing granulomatous vasculitis on biopsy of appropriate tissue in a patient with the clinical findings of upper and lower respiratory tract disease together with evidence of glomerulonephritis.
Pulmonary tissue, preferably obtained by open thoracotomy, offers the highest diagnostic yield, almost invariably revealing granulomatous vasculitis. Biopsy of upper airway tissue usually reveals granulomatous inflammation with necrosis but may not show vasculitis. Renal biopsy confirms the presence of glomerulonephritis.
The specificity of a positive c- ANCA titer for WG is very high, especially if active glomerulonephritis is present. However, the presence of c-ANCA should be adjunctive and, with very rare exceptions, should not substitute for a tissue diagnosis.
Even when clinical picture suggestive of ANCA associated disease and +ve MPO and PR3, tissue biopsy is recommended because possible false positive and toxic rx.
Therefore ANCA titre first- non invasive test before invasive test and helps corroborate diagnosis, but tissue biopsy needed for definitive diagnosis ( FNAB chest lesions best, but Nasopharyngeal lesion done first as less invasive)
Question 2
Answer A
–amiodarone induced pulm fibrosis
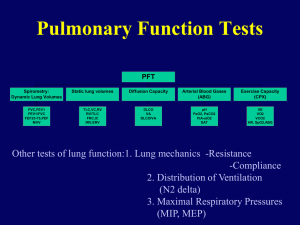
Issues- drugs causing pulm tox, DLCO interpretation, CXR changes of ILD, restrictive spirometry
A test of the diffusing capacity of the lungs for carbon monoxide (DLCO) is one of the most clinically valuable tests of lung function after spirometry. In Europe, the
DLCO is called the "transfer factor" for carbon monoxide, since it measures the ability of the lungs to transfer gas from inhaled air to the red blood cells in pulmonary capillaries
Obstructive disease
— Perhaps the most frequent use of DLCO is in the differential diagnosis of airways obstruction in current or former cigarette smokers:
• The DLCO is an excellent index of the degree of anatomic emphysema in smokers with airways obstruction. A low DLCO correlates highly (r > 0.85) with a low mean density of lung tissue on lung CT scan and with the degree of anatomic emphysema
• Smokers with airways obstruction but normal DLCO values usually have chronic "obstructive" bronchitis but not emphysema.
• Patients with airway obstruction from asthma have normal or high DLCO values [5].
Unlike the FEV1, the DLCO does not correlate well with the degree of dyspnea in chronic obstructive pulmonary disease (COPD), and following such patients with serial DLCO tests has not been reported to have clinical value.
Restrictive disease
— Another common application of the DLCO is for detection of mild (early or preclinical) interstitial lung disease in high risk patients, such as those with:
• Stage one sarcoidosis.
• Extrinsic allergic alveolitis.
• Chest radiation
• Use of drugs known to have pulmonary toxicity (eg, amiodarone, bleomycin, nitrofurantoin)
• Lung or bone marrow transplants
• HIV-infection and high risk for Pneumocystis pneumonia].
The normal range for DLCO is wide; as a result, it is much more sensitive to obtain a baseline DLCO test prior to therapy and subsequently perform a followup examination.
The DLCO helps in the differential diagnosis of restriction, identified by reduced lung volumes (eg, TLC and VC):
• A low DLCO suggests interstitial lung disease (ILD)
• A normal DLCO is consistent with an extrapulmonary cause of the restriction, such as obesity, pleural effusion or thickening, neuromuscular weakness, or kyphoscoliosis.
QuickTime™ and a TIFF (Uncompressed) decompressor are needed to see this picture.
A/ Amiodarone induced interstitial lung disease
UP TO DATE- DIAGNOSIS — The diagnosis of amiodarone-induced pulmonary toxicity is one of exclusion. The differential diagnosis of pulmonary processes which may present similarly to amiodarone toxicity includes congestive heart failure, infectious pneumonia, pulmonary embolism, and malignancy.
Can occur one month up to 5 yrs.
The presence of three or more of the following suggests the "clinical diagnosis" of amiodarone pulmonary toxicity.
• New or worsening symptoms or signs
• New abnormalities on CXR
• A decline in total lung capacity (≥15 percent) or in DLCO (>20 percent)
• Presence of phospholipidosis in lung cells
• A marked CD8+ lymphocytosis in lavage fluid
• A lung biopsy that reveals diffuse alveolar damage, organizing pneumonia, interstitial pneumonitis, or fibrosis
• Improvement in lung manifestations following withdrawal of the drug (with or without steroid therapy)
Symptoms and signs —a nonproductive cough and dyspnea are present in 50 of
75 percent of individuals at presentation. Pleuritic pain, weight loss, fever (33 to
50 percent of cases), and malaise . physical examination - bilateral inspiratory crackles,no clubbing. R/o CCF
Laboratory studies — Peripheral blood findings are nonspecific but include elevations of the white blood cell count, the serum lactate dehydrogenase (LDH) level, and the erythrocyte sedimentation rate
Eosinophilia and antinuclear antibodies are not typically seen. Amiodarone levels are usually within the normal range and are not predictive or diagnostic of pulmonary toxicity - - BUT pulm toxicity more often occurs at doses gr
400mg/day. concentrations of KL-6, a mucin-like high molecular weight glycoprotein secreted by proliferating type II pneumocytes, shows promise as a marker of amiodarone pulmonary toxicity.
Chest imaging studies
— The chest x-ray in amiodarone pulmonary toxicity may reveal diffuse or localized interstitial, alveolar, or mixed opacities
Increased gallium uptake in the lung has been suggested as a sensitive marker of the presence of amiodarone pneumonitis.
Pulmonary function testing — As noted above, lung function studies are not diagnostic of pulmonary toxicity because they are frequently abnormal in patients taking amiodarone. However, a documented decline in the DLCO of greater than
20 percent is useful in suggesting the need for closer monitoring or for further diagnostic testing.
Cannot diagnose CFA unless amiodarone ceased and assessed to see effect.
B/ cryptogenic fibrosing alveolitis ( Idiopathic pulm fibrosis) - pulmonary fibrosis without cause.-- pulm fibrosis
CFA —elderly men, ? inhaled environ antigen, p/w dry cough , breathlessness- signs- cyanosis, clubbing, fine late insp cracks
Ix:- small volumes, restriction, dec DLCO, CXR- intersitial shadowing at bases and periph, ABG- type 1 resp failure. Lung biopsy confirms. Rx; steroids +/- other immunosuppression, not great response to rx
C/ pneumonia- unlikely, time course too long, no consolidation on CXR
D/ Cardiac failure- not charachteristic CXR, told in q no other signs heart failure
E/ Sarcoidosis
– multisystem granulomatous disease – effects eye in 30% ( lots of effects)
young adults
- granuloma- mulnitinucleate giant cells.
Acute- eythema nodosum and bilat hilar adenopathy = Sarcoidosis UPO
Chronic- insidious – multi organ involvement
Lungs-CXR -- BHL BHL + pulm infil diffuse pulm infiltrates
Pulmonary disese- nil to sob, dry cough, fever, malaise, weight loss
MID and UPPER ZONES most freq involved
Extra pulm disease- lymph nodes, splenomeg, eyes, subclinical liver( but diagnostic), SKIN- EN
Eyes- acute anterior uveitis
Uncommon- neuro( nerve palsies sec to infiltration, cardiac, bone cysts
Dx – biopsy ( transbronchial/endobronchial of nodes), Inc ACE levels, Inc calcium
Rx- steroids +/- steroid sparing agents- response unpredictable
Definite indication for hypercalceamia and hypercalciuria despite ca restriction
Approach to PT with diffuse interstitial lung disease
4 questions
1/ is disease acute or chronic
2/ does pt have underlying systemic disease or exposure or is it primary lung
3/ is pt immunosuppressed- r/o infection ( COMMUNITY OR OPPORTUNISTIC), drug toxicity
4/ does pt need hospital- fever, rr>35, sats less 90%, pa02 < 60