Chapter 23 Notes - Las Positas College
advertisement
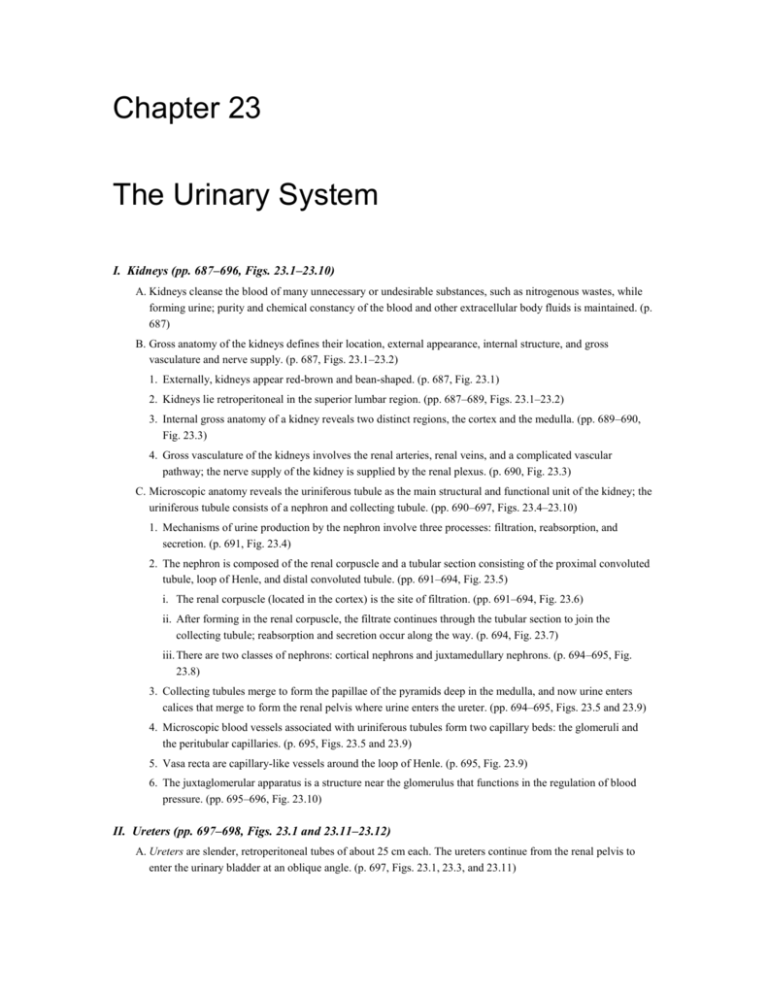
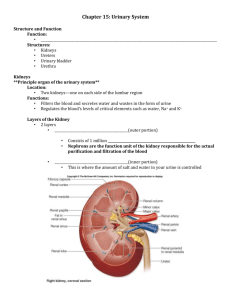
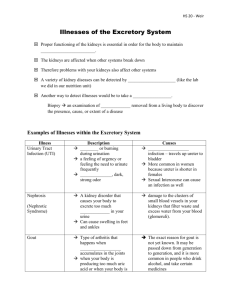
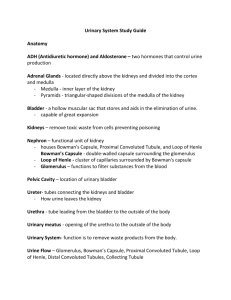
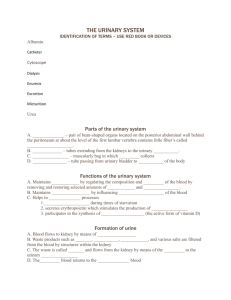
Chapter 23 The Urinary System I. Kidneys (pp. 687–696, Figs. 23.1–23.10) A. Kidneys cleanse the blood of many unnecessary or undesirable substances, such as nitrogenous wastes, while forming urine; purity and chemical constancy of the blood and other extracellular body fluids is maintained. (p. 687) B. Gross anatomy of the kidneys defines their location, external appearance, internal structure, and gross vasculature and nerve supply. (p. 687, Figs. 23.1–23.2) 1. Externally, kidneys appear red-brown and bean-shaped. (p. 687, Fig. 23.1) 2. Kidneys lie retroperitoneal in the superior lumbar region. (pp. 687–689, Figs. 23.1–23.2) 3. Internal gross anatomy of a kidney reveals two distinct regions, the cortex and the medulla. (pp. 689–690, Fig. 23.3) 4. Gross vasculature of the kidneys involves the renal arteries, renal veins, and a complicated vascular pathway; the nerve supply of the kidney is supplied by the renal plexus. (p. 690, Fig. 23.3) C. Microscopic anatomy reveals the uriniferous tubule as the main structural and functional unit of the kidney; the uriniferous tubule consists of a nephron and collecting tubule. (pp. 690–697, Figs. 23.4–23.10) 1. Mechanisms of urine production by the nephron involve three processes: filtration, reabsorption, and secretion. (p. 691, Fig. 23.4) 2. The nephron is composed of the renal corpuscle and a tubular section consisting of the proximal convoluted tubule, loop of Henle, and distal convoluted tubule. (pp. 691–694, Fig. 23.5) i. The renal corpuscle (located in the cortex) is the site of filtration. (pp. 691–694, Fig. 23.6) ii. After forming in the renal corpuscle, the filtrate continues through the tubular section to join the collecting tubule; reabsorption and secretion occur along the way. (p. 694, Fig. 23.7) iii. There are two classes of nephrons: cortical nephrons and juxtamedullary nephrons. (p. 694–695, Fig. 23.8) 3. Collecting tubules merge to form the papillae of the pyramids deep in the medulla, and now urine enters calices that merge to form the renal pelvis where urine enters the ureter. (pp. 694–695, Figs. 23.5 and 23.9) 4. Microscopic blood vessels associated with uriniferous tubules form two capillary beds: the glomeruli and the peritubular capillaries. (p. 695, Figs. 23.5 and 23.9) 5. Vasa recta are capillary-like vessels around the loop of Henle. (p. 695, Fig. 23.9) 6. The juxtaglomerular apparatus is a structure near the glomerulus that functions in the regulation of blood pressure. (pp. 695–696, Fig. 23.10) II. Ureters (pp. 697–698, Figs. 23.1 and 23.11–23.12) A. Ureters are slender, retroperitoneal tubes of about 25 cm each. The ureters continue from the renal pelvis to enter the urinary bladder at an oblique angle. (p. 697, Figs. 23.1, 23.3, and 23.11) B. Microscopic anatomy of the ureter reveals walls composed of mucosa, muscularis, and adventitia. The epithelium of the mucosa is transitional epithelium. The muscularis of the ureter is unlike the digestive tract because the inner layer is longitudinal and the external layer is circular. The inferior one-third of the ureter contains an additional external layer of muscularis, which is longitudinal. (p. 698, Fig. 23.12) III. Urinary Bladder (pp. 698–700, Figs. 23.13–23.16) A. The urinary bladder is a collapsible, muscular sac that stores and expels urine. It lies on the pelvic floor inferior to the peritoneal cavity. (pp. 698–700, Figs. 23.13–23.16) 1. An empty urinary bladder is shaped like an upside-down pyramid. At the anterior angle is a fibrous band called the urachus, which is the closed vestige of the allantois. (pp. 698–699, Figs. 23.13 and 23.14) 2. Arteries supplying the urinary bladder are branches of the internal iliac arteries. (p. 699) 3. The walls of the urinary bladder are composed of mucosa, a thick muscular layer, and adventitia. The epithelium of the mucosa is transitional epithelium. The muscular layer, called the detrusor muscle, is comprised of intermingled smooth muscle fibers arranged in inner and outer longitudinal layers and a middle circular layer. (pp. 699–700, Figs. 23.15 and 23.16) 4. A full adult urinary bladder can contain about 500 ml of urine. (p. 700) IV. Urethra (pp. 700–701, Fig. 23.16) A. The uretha is a thin-walled tube that drains urine from the urinary bladder and conveys it out of the body. B. In males, the smooth muscle layer of the urethra becomes very thin toward its distal end. The epithelium of the urethra in males changes from transitional epithelium to stratified and pseudostratified columnar, and finally stratified squamous epithelium at the urethra’s distal end. (pp. 700–701, Fig. 3.16) C. The internal urethral sphincter is a thickening of the detrusor muscle. This sphincter is an involuntary one, which prevents dribbling of urine between voiding. The external urethra sphincter is under voluntary control. (p. 701) D. The length and functions of the urethra differ in males and females. The female urethra is approximately 4 cm long, while in males the urethra is about 20 cm long. The male urethra has three named regions. From internal to external, the regions are prostatic urethra, membranous urethra, and spongy urethra. (p. 701) V. Micturition (pp. 701–702, Fig. 23.17) A. Micturition, also called urination or voiding, is the act of emptying the urinary bladder. VI. Disorders of the Urinary System (pp. 702–705) A. Examples of disorders of the urinary tract are urinary tract infections, renal calculi, polycystic kidney disease, and cancer of urinary organs. VII. The Urinary System Throughout Life (pp. 705–706, Fig. 23.18) A. Three sets of kidneys develop in sequence in the embryo: pronephric, mesonephric, and metanephric. (p. 705, Fig. 23.18) B. Kidneys of newborns cannot concentrate urine. (p. 706) C. Urinary infections are the most common problem through middle age; incontinence is a problem with the elderly. (p. 706) SUPPLEMENTAL STUDENT MATERIALS to Human Anatomy, Fifth Edition Chapter 23: The Urinary System To the Student Perhaps a nice, juicy steak is one of your favorite foods. Why mention food in a chapter titled “The Urinary System”? When your body processes food, metabolic wastes are produced. For example, a steak is meat, meat contains protein, protein is made of amino acids, amino acids contain nitrogen, and nitrogen-containing substances are poison to your cells if they accumulate in your tissues and blood. Kidneys filter organic wastes from the blood and help maintain the purity and chemical constancy of the blood with, of course, the production of urine as a vital excretory result. Thoroughly review all the functions of the kidneys because removal of nitrogenous waste is only one of many important functions. There is an excess of 1 million structural and functional units of the kidney called uriniferous tubules, consisting of nephrons plus collecting tubules. Collectively, in one kidney, uriniferous tubules are an estimated 85 miles long, and filter approximately 1200 ml (about 5 cups) of blood per minute. The number of uriniferous tubules is constant from birth, and new ones do not form in the event of injury or disease—hence, the significance of kidney transplants and artificial kidney machines. Step 1: Describe the gross structure and function of the kidneys. - List all functions accomplished by kidneys during the formation of urine. - Identify all organs associated with the transport and storage of urine. - Describe the external gross anatomy of kidneys, including location and hili. - Name the structures that enter and leave the kidney through the renal hilus. - Distinguish between perirenal fat and pararenal fat, commenting on their functions. - Distinguish between the renal capsule and renal fascia, commenting on their functions. - Describe the internal gross anatomy of the kidney, defining renal cortex, renal medulla, renal pyramids, renal pelvis, renal sinus, and major and minor calyces. - Explain the nerve supply to the kidneys. - Draw a flowchart representing the vascular pathway through a kidney, beginning with the renal artery and ending with the renal vein. (Hint: Refer to Figure 23.8 and 23.9, if needed.) Step 2: Describe the microscopic anatomy of the kidneys and urine formation. - Identify the main structural and functional unit of the kidney, naming its two major parts, and explain their orientation within the kidney. - Define basic kidney functions during urine production: filtration, reabsorption, and secretion. - Name the parts and explain how each part of the uriniferous tubule contributes to urine formation. - Identify the part of the filtration barrier that prevents the passage of red blood cells into the capsular space. (Hint: Refer to Figure 23.6c.) - Explain how the unique structure of podocytes contributes to filtration. - Draw a single, generalized uriniferous tubule, showing its basic relationship to blood vessels and sites of filtration, reabsorption, and secretion. (Hint: Refer to Figure 23.4.) - Explain how the kidney acts to conserve water and prevent dehydration. - Identify two major categories of nephrons, pointing out their major differences. - Describe the association of microscopic blood vessels and the uriniferous tubule, being very observant with the interlobar and interlobular vessels. - Name specific beds of capillaries and identify their roles in urine production. - Explain the structure and function of the juxtaglomerular apparatus and describe its location with respect to the gross structure of the kidney. - Define and describe renal interstitium. Step 3: Describe the gross structure and microscopic structure of the other organs of the urinary system: ureters, urinary bladder, and urethra. - Describe the location and function of the ureters. - Explain the histological structure of the ureteral (ureteric) wall. - Explain how urine moves through the ureter. - Describe the location of the urinary bladder, explaining positions and shapes of full and empty urinary bladders. - Define urachus, indicating its embryonic origin. - Define trigone, explaining the relationship of openings located there. - Describe the histological structure of the urinary bladder, explaining why distensibility is unique for this organ. - Describe the location and function of the urethra, including the sphincters. - Explain the gross anatomical differences of the urethra between males and females. - Explain how urine moves through the urethra. - Define micturition. Step 4: Describe disorders of the urinary system and changes that occur with aging. - List basic symptoms and features of specific disorders such as urinary tract infections, kidney stones, polycystic kidney disease, and cancer of the urinary bladder or kidney. - Trace the embryonic origin of the organs of the urinary tract. - List several effects of aging on the organs of the urinary tract.