Mgmt. of Cercopithecine Herpesv
advertisement

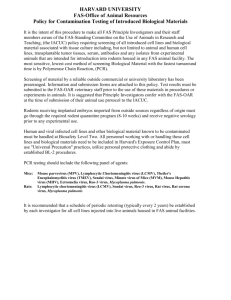
THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 1 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 I. PURPOSE To provide guidelines for the consistent management of employees potentially exposed to Cercopithecine herpesvirus 1 (formerly Herpesvirus simiae "B virus") through biohazardous injuries and exposures. This policy has been modified from a policy prepared by the University of Wisconsin-Madison which is used with their permission. II. POLICY A minimum of Biosafety Level 2 practices, containment equipment and facilities are recommended for all activities involving the use or manipulation of tissues, body fluids and primary tissue cultures from Macaca spp. (macaques) and other Old World monkeys. All personnel working with macaques and other Old World species or entering rooms housing these animals, should wear appropriate protective equipment (gloves, eyewear, masks, disposable coveralls). The Principal Investigator (PI) or animal care supervisor must provide all members of his/her research team or animal care workers the information on the dangers of B virus infection, including recognition of the modes of transmission, methods of protection from exposure, post-exposure follow-up, and symptoms of B virus infection. The Thomas Jefferson University Health Services shall be responsible for the appropriate assessment, treatment and follow-up of potentially exposed employees. Employees should report to the TJU Hospital emergency department during off hours or when University Health Services is not open. The Office of Animal Resources veterinarians are responsible for the assessment and follow-up of the involved monkey. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 2 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 III. BACKGROUND Cercopithecine Herpesvirus (also known as Herpesvirus simiae B virus) was first isolated by Sabin and Wright in 1932 from the brain and spinal cord of a researcher who died of meningoencephalitis following a bite from a macaque monkey. The virus has since been recognized to be endemic among Old World Macaca genus monkeys (macaques) and to cause minimal morbidity in its natural host. Humans who have contact with macaques or their products may be exposed to B virus through bites, scratches, contaminated needle sticks and other routes. No other Old World and no New World monkeys are known to naturally harbor B virus. The prevalence rate of B virus infection is low among immature animals but approaches 80-90% in adult populations. Chronically infected monkeys actively shed virus only intermittently (estimate prevalence rates 2-3%). Monkeys are more likely to shed B virus when they are ill, under stress, immunocompromised, or during breeding season. Potentially infectious fluids are ocular, oral and genital secretions from the monkey as well as primary cell cultures derived from macaque kidney cells, aerosol exposure, and exposure to cleaned monkey skull. The risk of infection is higher in certain types of exposures. Deep puncture wounds, inadequately cleansed wounds, and wounds to the face, neck or thorax are considered to be high risk. Exposure to peripheral blood has not been demonstrated to cause infections in humans. As of December, 1995, fewer than 40 human B virus infections have been described in the English literature, of which fewer than 30 are reported in detail. Twelve of those cases occurred in the 1950’s, concomitant with testing polio vaccines in macaques. Despite as many as several thousand annual monkey inflicted bites, scratches and other exposures, B virus infection has rarely been documented in humans and must be considered an uncommon result of biohazardous injury. Since the 1987 Florida cluster of human infections and the Centers for Disease Control and Prevention (CDC) and the National Institutes of Health (NIH) publication of recommendations for preventing B virus infections, thousands of specimens from bitten or scratched primate workers have been tested for B virus. Several hundred primate handlers have been empirically treated for B virus infection pending test results. Even with this intensive surveillance, only 6 confirmed human infections have been detected since January, 1993. The only reported human to human transmission of B virus infection occurred through direct, repeated inoculation of drainage from herpetiform lesions on to skin with contact dermatitis, possibly facilitated by the use of steroid cream. Although theoretically possible, no other instances of human to human transmission have been reported. There is no documented case of asymptomatic infection. In an attempt to formulate a rational approach to the management of B virus exposure in humans, the CDC sponsored a B Virus Working Group consisting of invited infectious disease specialists, primate and laboratory animal veterinarians and herpesvirus experts. These published guidelines are based upon limited information available from human cases, a small number of unpublished cases managed by Group members, knowledge of the herpes simplex virus (the closest human counterpart of B virus) and consensus opinion of the Group in the absence of hard data (1, 2). THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 3 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 6/06/01, 06/26/08, 05/24/11, 07/22/2014 _ IV. ROUTE OF EXPOSURE Transmission to humans occurs by exposure to contaminated Macaque saliva, secretions, or tissues. The most likely routes to transmission are bites and scratches or splashes. Exposure to peripheral blood from macaques has not been reported to cause infection in humans. However, all macaques and their tissues should be regarded as infected. There has been a report of person-to-person transmission. V. a.) Bite or scratch by a macaque that breaks the skin. b.) Laceration from contaminated instruments used during surgery or necropsy involving the central nervous system, eyes, mouth, or urogenital areas. c.) Laceration from dental instruments used on macaque, or glass containing macaque cell culture lines. d.) Needle stick from a contaminated needle used on macaque eyelid (TB syringe) or oropharynx; for aspirating skin or mucosal lesions; at any site on a macaque. e.) Splash of macaque oral secretions or aerosolized tissue into eyes or onto mucous membranes. f.) Fomites contaminated by ocular, oral or urogenital secretions or skin lesion/fluid from a macaque. g.) Low or no known risk of exposure would include any exposure to non-human primates other than macaques; exposure to non-human primate cell culture system, exposure to nonhuman primate blood. FORMS TJU forms are available from departmental secretaries as well as LAS Supervisor staff or the Workers Compensation - 1st floor Main building. • • Employee Accident Report: Electronic form on Jeffshare must be filled out. However, paper copy of Form No. 0155-10 should also be filled out and taken with you if you are going to the Emergency Department for treatment. See the University Veterinarian in regard to appropriate forms for diagnostic evaluation of the animals. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 4 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 ______ VI. PROCEDURE A. The Injured Employee’s Role Prevention 1.) Prevention of B virus infection must always be the first goal and can be achieved through the following measures: a.) All macaque monkeys and their tissue should be regarded as infected. Viral shedding is intermittent and can occur in the absence of visible lesions. b.) Handling of macaques should be minimized and should be done by trained personnel. c.) Transfer and squeeze-back cages and pole and collar transfer should be used to move monkeys whenever possible. d.) Ketamine sedation may be used to facilitate removal of monkeys from cages, particularly large or difficult animals. e.) Use appropriate personal protective gear (mask, goggles/face shields, long sleeved and long legged clothing, gloves) when handling animals or cleaning cages. f.) Do not recap needles or sharps! g.) Dispose of sharps (scalpel blades, contaminated sharp glass or needles) immediately after use in a designated, conveniently located puncture resistant sharps container. h.) Surfaces in contact with monkeys or their fluids should be disinfected after use. i.) Cages/equipment with potential for contamination from monkey fluids should be inspected for sharp edges that may cause injury to workers. j.) Always practice appropriate hand washing technique. k.) Routinely report biohazardous injuries. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 5 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 ______ First Aid 1.) If a biohazardous injury occurs, risk of infection can be reduced by immediate first aid. A bite kit can be found inside the 3rd floor primate procedure room, outside the 3rd and 4th floor primate housing rooms, and outside wash bay (6th floor JAH). The bite kit should have the following items: providone iodine scrub; brushes; sterile water; four viral culturettes (for using with the primates); timer; packet with orange cover sheet that contains this SOP I.D.09 which contains the intake sheet, consent for treatment sheet, and post-exposure education sheet; paper copy of the accident report (Rev. 08/09); monkey blood specimen and/or viral culturette sheet; B virus Exposure Mini-Protocol; and monkey serum shipment form. a.) Set timer for 15 minutes. Thoroughly cleanse/scrub/irrigate the wound with soap or topical antimicrobial agent (povidone iodine or chlorohexidine) for 15 minutes. If eyes, mouth, nose or other mucous membranes have been exposed, irrigate the site for 15 minutes with sterile saline or rapidly flowing tap water. b.) Culturing a wound prior to cleansing is not recommended due to the risk of further contamination with infected material. The cuturettes have been placed in the bite kit for the veterinary staff to use when obtaining samples from the monkey. c.) After cleansing the injury, cover the injury (sterile dressing if available) and proceed to University Health Services. If after hours, proceed to the Emergency Department. An accident report must be completed Form No. 0155-10 (Rev. 2/05). If you go to the Emergency Department as soon as practical, report the injury to your supervisor. d.) If possible, report the identification number of the involved animal. e.) If you go to the Emergency Department take a copy of the handouts with the orange cover sheet with you to the physician. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 6 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 Reporting 1.) AFTER the appropriate first aid measures have been completed, the employee should report the exposure to his/her supervisor. The on-line accident report should be completed by the employee and signed by the supervisor; if the employee is going to the Emergency Department the paper accident report is also filled out (form No. 0155-10). The supervisor will contact University Health Services (x 5-6835) to alert them that an exposure has occurred and will send the employee without delay. If the exposure occurs after 4:00 p.m. Monday through Friday or on weekends, the employee will report to the Emergency Department. A copy of this policy and the accident report will be sent with the employee who is seen in the Emergency Department. The supervisor will contact the University Veterinarian to report the exposure and to identify which animal was involved, if possible. PI must also be notified. In addition, the Biological Safety Officer (Sue Gotta at 503-7422) must be notified that an exposure has taken place. University Health Services will forward the accident report to the Department of Environmental Health and Safety. Injury Follow-Up 1.) The incubation for infection is 2 days to 5 weeks. Exposed employees will be seen in University Health Services for the original injury, 3 days post injury and again 4 weeks post injury. The early signs and symptoms suggesting B virus infection will be reviewed. Exposed employees will be advised to report as soon as possible for physician evaluation in UHS if any of the following signs or symptoms occurs. Among untreated humans, estimates of the mortality rate from B virus infection is approximately 80%. a.) Vesicular lesions near injury site b.) Localized numbness, itching, pain, tingling c.) Regional lymph node enlargement d.) Fever THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 7 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 2.) e.) Muscle weakness f.) Conjunctivitis g.) Stiff neck, headache, nausea, blurred vision The UHS nurse will see the exposed employee without delay and, despite prior first aid measures, may repeat the appropriate cleansing. The accident report will be reviewed to verify the time, date and place of the accident, the monkey identification and the circumstances leading to the accident. The employee will be seen next by the UHS nurse practitioner (CRNP) or physician. The CNRP/MD will review the following: 1. The employee’s wound or exposure site. 2. The employee’s current medical history including medications and allergies. 3. The date of the employee’s previous tetanus booster. 4. The primate’s history of B virus serology and current clinical status as well as the nature of the research involving the primate. The CRNP/MD will determine the testing to be done. This may include a culture of the exposed site and/or serologic testing. Serum will be separated from the blood sample in the Jefferson Clinical Laboratories and then forwarded to National B virus Resource Center B. The Role of Supervisor/PI: Prevention Train employees on the risk of B virus infection, the methods of preventing B virus infection, the need to clean wounds immediately, and the importance of reporting injuries and/or symptoms to supervisors. First Aid If present at the time of the injury, assist the injured employee to cleanse the wound for 15 + minutes. If wound is bleeding, take care not to directly contact employee’s blood without using standard precautions. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 8 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 Reporting If possible, identify the animal causing the injury and notify the staff veterinarian to review the animal’s record, examine the animal and collect specimens on the animal for appropriate laboratory tests. Complete the Supervisor section of the Employee Accident Report and call Environmental health and Safety at x 5 - 7233 for immediate reporting of the accident. If possible isolate the suspect animal and notify a veterinarian, a veterinary technician, a manager or the P.I. Refer the employee immediately to UHS or to the Emergency Department after hours. Call University Health Services or the Emergency Department prior to sending the employee. The employee will take the paper copy of the accident form to the Emergency Department when reporting the injury. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 9 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 C. The Role of the Attending Veterinarian If the non- the human primate can be identified samples should be collected. Procedure For Obtaining Samples From Non-human Primates. 1.) The animal identification number is determined if possible. 2.) The identified animal is anesthetized as soon as possible after the exposure for a physical examination and sample collection. A thorough examination by the attending veterinarian is performed with emphasis on mucosal membranes. 3.) Abnormalities are noted on the B virus submission form in the bite and scratch kit. 4.) Blood must be collected in serum separator tubes. A 5-7 ml sample of blood is collected as close as possible at the time of injury. Allow 15 minutes for clot to form. The attending veterinarian or qualified technician will centrifuge the sample. 1.0-2.0 ml of serum is needed. Transfer serum to a serum storage tube. Properly label the serum sample with the animal ID and serum collection date. Until the serum samples are shipped, store them at 2-6°C (samples are good for up to one week) or store them at 60 -80ºC (samples are good indefinitely). The serum is checked for herpes-B virus within 48 hours. 5.) If indicated, four sterile swabs for viral culture are collected: (1) buccal, (2) right conjunctiva, (3) left conjunctiva, and (4) genitalia. If a lesion suggestive of B virus infection is noted it should also be collected. Properly label sample tubes with the animal ID, swab collection date, and swab site. Until the viral swabs are shipped store, store them at 2-6°C (samples are good for up to one week) or store them at 60 -80ºC (samples are good indefinitely). Swabs are to be placed in commercially prepared viral transport media from Micro Test (division of Remel Products); 1-800-255-6730; www.remelinc.com 6.) Serum samples are collected again 14-21 days later. A second sample must be collected because paired samples are used to run diagnostic tests. 7.) Fill out National B Virus Resource Center Submission Form and include it with Shipment. Forms are located in bite kit and at www.gsu.edu/bvirus. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES I.D.09 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 D. 10 of 15 _ Sample Shipping: Nonhuman primate & human samples are sent to the same address. See B Virus Exposure Mini-Protocol. A copy should be kept in the bite kit. 1.) Contact the laboratory prior to shipping by: Telephone: 404-413-6550 (Dr. Julia K. Hilliard, Ph.D., Laboratory Director) Fax: 404-413-6556 Email: bvirus@gsu.edu 2.) Fill out the National B Virus Resource Center Shipping Form. A copy should be kept in the bite kit. This copy must be included with specimen shipment. Ship samples ASAP by overnight courier to National B Virus Resource Center Virology Immunology Center Georgia State University 161 Jesse Hill Jr. Drive Atlanta, GA 30303 3.) Label packages and air bills shipped on Friday for “Saturday Delivery”. Do not select the “Next Day Delivery” option (this is considered the next business day). Contact the National B Virus Resource Center with the air bill number for tracking missing packages on the weekends. 4.) The box should be filled with an adequate amount of dry ice to ensure the sample arrives frozen. Use extra dry ice for Friday, weekend or holiday shipments 5.) Additional information can be obtained at www.gsu.edu/bvirus THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES I.D.09 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 E. 11 of 15 Immediate Management Strategy/Role of University Health Services/Thomas Jefferson University Hospital Emergency Department 1.) During normal working hours, all persons with exposure to B Virus should report to University Health Services (Suite 205, 833 Chestnut Street) after appropriate cleaning of the wound for 15 minutes. On weekends and after 4 p.m., persons with exposures should report to the TJUH Emergency Room. 2.) The UHS/ED clinical will document the details of the exposure and verify that the appropriate first aid measures were done. If not completed, the UHS/ED staff will clean the wound or wash the mucous membranes for 15 minutes. 3.) Cultures of the wound will be done where appropriate in UHS or the Emergency Department and sent to the National B Virus Resource Center. Blood must be collected in serum separator tubes. A 5-7 ml sample of blood is collected as close as possible at the time of injury. Serology for the exposed employee will be drawn in UHS. If the employee is seen in the ED on the day of the exposure, the employee will be referred to UHS as soon as possible for serology. 4.) The UHS/ED staff will evaluate and possibly prescribe the following for any potential exposure to B Virus: a. b. c. Antibiotic Prophylaxis: i Augmentin 875 mg by mouth every 12hrs considered with bites to the high risk areas, i.e. fingers and hands. Tetanus update: i. Tdap where possible. Antiviral Prophylaxis for prevention of the B virus: i. Drug of Choice - Valcyclovir l g by mouth every 8hrs fo 14 days. Alternative Choices ii. Famcyclovir 500 mg by mouth every 8hrs for 14 days; OR iii. Acyclovir 800 mg by mouth 5 times daily for 14 days. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES I.D.09 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 5.) 12 of 15 Each exposure will be evaluated for four major variables: a. Animal source i. Macaques are the only primates which transmit B virus. ii. Immunocompromised, ill, breeding, and stressed animals are more likely to transmit the virus. b. Timeliness/adequacy of first aid i. Wounds cleaned within the first few minutes of exposure are less likely to transmit the virus. ii. Inadequately cleaned wounds are more likely to transmit the virus. c. Type of wound iii. Wounds to head, neck or torso are considered high risk. iv. Deep wounds are more difficult to clean and are considered high risk. d. Type of materials involved in exposure v. Exposure to CNS fluid, fluids from eyelids or mucous membranes are considered high risk. vi. Blood exposure is considered low risk due to rare viremia in infected animals. 6.) Counseling - Person to person transmission of B virus disease occurred in one reported case of B virus disease that involved two people sharing a topical medication. Exposed employees will be advised to avoid exposing others to body fluids or skin lesions during the incubation period of 2-35 days, the side effects of the prophylaxis, and the follow up schedule. Discussion of potential risks and benefits associated with empiric therapy vs. close observation must be held with the patient. The UHS CRNP/MD will discuss the pros and cons of the postexposure prophylaxis and will review the most frequent reported side effects of nausea, headache, diarrhea and rash. Possible neurologic side effects and renal impairment has been associated with treatment with acyclovir. A consent for treatment will be signed by the exposed employee. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES I.D.09 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 13 of 15 Based on well documented human B virus exposures, clinical evidence of infection is most likely to develop between 5 and 30 days after exposure. In the event of suspected B virus disease, the patient will be thoroughly evaluated with attention specifically to any dermatologic symptoms and/or neurologic abnormalities. The evaluation may include cultures of skin lesions, conjunctiva, and oropharynx. Serologic testing will be ordered as well as routine chemical and hematologic studies. Treatment with intravenous anti-viral medication will necessitate an inpatient hospitalization. Consultation with an infectious diseases specialist will be made. Decisions regarding further testing and determination of which anti-viral medication will be done in accordance with the recommendations of the infectious disease specialist. vii. Discussion of potential risks and benefits associated with empiric therapy vs. close observation must be held with the patient. The veterinarians may also be reached for consultation. Dr. Judy Daviau is available by pager at 877-656-9759. If she cannot be reached, Dr. Cynthia Lang can be paged at 877-656-6428. It will be the responsibility or the veterinarians to assess the clinical status of the animal and to arrange for testing. viii. Follow up - Exposed employees will be seen in UHS or the ED according to the following time frame: a. Day of the exposure. b. 2-3 days post exposure. c. 4 weeks post exposure. d. 3 months post exposure if antiviral prophylaxis taken. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 14 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 VII. REFERENCES 1.) Adapted from University of Wisconsin - Madison, Policy for Management of Cercopithecine herpesvirus 1 - with permission. 2.) Cohen JI, Davenport DS, Stewert JA, et al. Recommendations for Prevention of and Therapy for Exposure to B Virus (Cercopithecine Herpesvirus 1) CID 2002; 35: 1191-1203. 3.) Holmes GP, Chapman LE, Stewart JA, et al. Guidelines for the prevention of Bvirus infections in exposed persons. Clin Inf Dis 1995; 20:431-439. 4.) Krugner-Higby L, Schultz KT. Herpesvirus simiae (Herpes B) and SIV as zoonoses. Lab Animal 1995; 24:24-31. THOMAS JEFFERSON UNIVERSITY ANIMAL RESOURCES STANDARD OPERATING PROCEDURES Section Page I.D.09 15 of 15 Title Date Issued/Revised Policy for the Management of Cercopithecine Herpesvirus 1 (formerly Herpesvirus Simiae or "B Virus") Exposures 04/06/98, 06/06/01, 06/26/08, 05/24/11, 07/22/2014 Signatures: Reviewed by: Name Title Date Name Title Date Name Title Date Reviewed by: Approved by: SUMMARY OF BIOHAZARDOUS INJURY PROTOCOL FOR THE POTENTIAL EXPOSURE TO CERCOPITHECINE HERPESVIRUS 1 (FORMERLY HERPESVIRUS SIMIAE OR “B VIRUS”) If a biohazards injury occurs, risk of infection can be reduced by immediate first aid. Monkey bite kits are available in monkey housing areas and laboratories. a.) Thoroughly cleanse/scrub/irrigate the wound with soap or topical antimicrobial agent (povidone iodine or chlorohexidine) for 15 minutes. Gentle washing of the wound is recommended. If eyes, mouth, nose or other mucous membranes have been exposed, irrigate the site for 15 minutes with sterile saline or rapidly flowing water. b.) After cleansing the injury, cover the injury (with a sterile dressing) and proceed to the University Health Services for further evaluation. Proceed to the Hospital emergency room during off hours. Employees reporting to the emergency room should bring a copy of this policy and standard operating procedure for the attending physician’s reference use. c.) As soon as practical, report the injury to your supervisor. If possible, report the identification number of the involved animal. d.) Your supervisor should contact the veterinarian responsible for the care of the involved animal and report the injury. e.) The veterinarian will examine and take animal cultures as per Guide for Post-exposure Sampling of Macaques (attached). f.) Supervisor will complete Section A. of the Thomas Jefferson University Accident Report (Form 0155-01) and comply with items 1 - 4 of the accident report. Important Phone Numbers: • University Health Services - x (5) 6835 • Emergency Department - x (5) 6840 • Environmental Health and Safety - x (5) 7233 • Biological Safety Officer - x (3) 7422 • Laboratory Animal Services - x (3) 6167 CONSENT FOR TREATMENT FOLLOWING A POTENTIAL EXPOSURE TO CERCOPITHECINE HERPES VIRUS 1, “MONKEY B VIRUS” I understand that I have had a potential occupational exposure to Cercopithecine herpes virus 1, also know simply as “B virus”. I have notified my supervisor and completed the proper paperwok according to department policy. I have had a chance to ask questions and have been advised of the risk of infection and the signs and symptoms of “B virus” disease. I understand that I am expected to return to University Health Services (UHS) for follow up and acknowledge receipt of the information sheet that gives me the specific dates for return. In addition, I understand that an antiviral medication noted below has been prescribed to me for fourteen days to prevent transmission of the “B virus”. The UHS/ER clinician has explained the pro’s and con’s of this post-exposure prophylaxis. I am aware of the possible side effects of this medication. I will report to UHS if I develop symptoms related to the medication or to a possible “B virus” infection. If I decide to discontinue the medication before fourteen days, I understand that I must contact UHS and advise them of my decision. My signature below indicates my willingness to take the prescribed medication. Medication Prescribed: ___ valacyclovir 1 g orally every 8 hours for 14 days ___ acyclovir 800 mg orally five times a day for 14 days ___ famcyclovir 500 mg orally every 8 hours for 14 days Possible side effects include: Nausea, headache, diarrhea and a rash Other: _________________________________ _______________________________________ Employee Signature _______________________________________ Date ______________________________________ UHS/ER Clinician ______________________________________ Date MACAQUE MONKEY EXPOSURE INTAKE FORM Date_________________ Exposure Date______________ Employee Name: ______________________________ DOB: ____________ TJU Veterinarians: Dr. Daviau (877) 656-9759 beeper; Dr. Cynthia Lang (877) 656-6428 beeper Monkey Information: Name: _________________ Health Status: _________________ Hx of B virus: _________________ Type of research: _________________ First Aid Measures in Department: ___________________________________ First Aid Performed in UHS/ER: _____________________________________ Physical Examination: Wound description: ________________________________________ Wound Culture done: _______ Serum Specimen drawn: ______ Assessment of Risk: _____________________________________ B virus Post Exposure Prophylaxis: ___ prophylaxis recommended ___ prophylaxis considered ___ prophylaxis not recommended Medication: ___ valacyclovir l g po q8h for 14 days ___ acyclovir 800 mg po 5 times per day for 14 days ___ famcyclovir 500 mg po q8h for 14 days ___ tetanus booster ___ Augumentin 825 mg BID for 5-7 days (for bites to hands) ___ other: ___________________________ Counseling: ___ side effects of medication reviewed ___ infection control during incubation period ___ signs and symptoms of B virus disease ___ follow up schedule reviewed ___ patient information sheet given/consent signed UHS/ER MD/CRNP SIGNATURE: _______________________________________ MACAQUE MONKEY POST-EXPOSURE PATIENT EDUCATION SHEET Today you have been seen after an occupational exposure to a monkey. You may have been exposed to a virus called Cercopithecine herpesvirus 1 or simply “B virus”. Although it is uncommon, there are cases of humans who have contracted this virus after a monkey scratch, bite, or splash to the eyes or mouth. The following is a list of dates for follow up in our office. Your supervisor will allow you to be seen as this is a Workers’ Compensation injury that must be followed closely. 1. Please return to UHS in Suite 205, 833 Chestnut St. on __________________ which is 3 days following your exposure. 2. Please return to UHS in Suite 205, 833 Chestnut St on __________________ which is 4 weeks following your exposure. 3. Please return to UHS in Suite 205, 833 Chestnut St on __________________ which is 3 months after your exposure. This appointment is only necessary if you were given medication to take after your exposure. You were given the following medication to take for 14 days: The most common side effects of this medication include headache, nausea, diarrhea and a rash. If you develop any of these symptoms, please call our office. If you develop any of the following symptoms prior to your scheduled return dates, please call us immediately at 955-6835: Blisters at the injured site Localized nunbness, itching pain and tingling at the injured site Lymph node enlargement Fever Muscle weakness in your arms or legs “Pink eye” symptoms Stiff neck with headache, nausea, blurred vision UNIVERSITY HEALTH SERVICES 833 Chestnut Street, Suite 205 (215) 955-6835 hours: Monday – Friday 7:30 am – 4:00 pm UNIVERSITY HEALTH SERVICES BLOOD SPECIMEN AND/OR VIRAL CULTURETTE FOR MONKEY B VIRUS EXPOSURE ATTENTION CENTRAL RECEIVING These specimens have been taken from an employee. Please separate the serum STAT and call University Health Services (5-6835) for pick up. If you receive these specimens from the Emergency Dept. after 5 PM or on the weekend, please save the serum and call University Health Services (5-6835) on the following business day. Our staff will collect these specimens. PLEASE DO NO OPEN THE CULTURETTE TUBE. THERE IS NO TESTING TO BE DONE ON THESE SPECIMENS BY THE CLINICAL LABORATORIES. DATE: ____________________________________________ PATIENT NAME: ___________________________________ DOB: ______________________________________________ DEPT: ______________________________________________ If you have any questions, please call our extension at 5-6835. You may leave a message on our voice mail. Thank you. Ellen M. O’Connor, MD Medical Director, University Health Services CHAIN OF CUSTODY FORM UHS PERSONNEL: Date Specimen Handled _______ Signature of RN ____________________ CLINICAL LAB PERSONNEL: Received by _____________________ Date: __________________________