Maternal-Neonatal Health (MNH) and Poverty
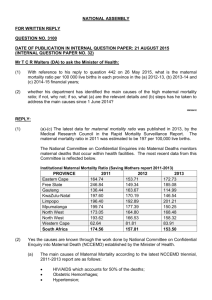
advertisement

February 2005 Maternal-Neonatal Health (MNH) and Poverty: Factors Beyond Care that Affect MNH Outcomes1 Thomas W. Merrick World Bank Institute Washington, DC 1 Background paper for Maternal-Newborn Health and Poverty (MNHP) Working Area 4: Making health systems respond to the health needs of mothers and their children, especially the poor and marginalized, during pregnancy, childbirth and the postpartum period. Review 4.f: Other reproductive health matters and inter-sectoral concerns. Table of Contents Introduction ..................................................................................................................................... 3 The Pathways Framework........................................................................................................... 3 Data on MNH and Poverty ............................................................................................................. 6 Data and Measurement Issues ..................................................................................................... 6 Regional and Cross-National Differences .................................................................................. 6 Table 1: Comparison of 1995 and 2000 Regional and Global Totals..................................... 7 Table 2: 2001 Global and Regional Estimates of Neonatal Mortality .................................... 7 Poverty Linkages ........................................................................................................................ 8 Table 3: Attendance at Delivery by a Medically Trained Person by Wealth Quintile ........... 8 Table 4: Averages of Pathways Indicators for Countries Grouped by MMR Level .............. 9 Linkages with Other Factors ....................................................................................................... 9 Table 5: Pathways Indicators for Large Countries ............................................................... 10 Table 6: Pathways Indicators for Countries with Highest MMRs ........................................ 11 Cross-National Analyses. .......................................................................................................... 11 Table 7: Correlations between Pathways Variables and MMRs .......................................... 11 Table 8: Averages of Pathways Indicators for Countries Grouped by Neonatal Mortality Rate ....................................................................................................................................... 12 Review of Evidence on Pathways Variables ................................................................................ 15 Other Reproductive Health Risk Factors .................................................................................. 15 Table 9: Total Fertility Rates by Wealth Quintile and Region ............................................. 15 Table 10: Contraceptive Prevalence by Wealth Quintile and Region .................................. 16 Table 11: Adolescent Fertility Rates by Wealth Quintile and Region.................................. 16 Table 12: Selected Findings on Other Reproductive Health Risks....................................... 21 Household and Community Factors.......................................................................................... 21 Health System Failures ............................................................................................................. 25 Table 13: Selected Findings on Health System Issues.......................................................... 28 Other Sectors ............................................................................................................................. 29 Table 14: Selected Findings on Transport Interventions ...................................................... 31 Table 15: Low Body-Mass in Reproductive-Age Women by Wealth Quintile and Region 33 Table 16: Child Malnutrition by Wealth Quintile and Region ............................................. 33 Public Policy and Governance: ................................................................................................. 33 Table 17: Governance Indicators for Countries Grouped by MMR Level ........................... 34 Addressing Obstacles and Information Gaps ................................................................................ 34 Policy and Program Actions ..................................................................................................... 34 Table 18: Actions to Address Obstacles ............................................................................... 35 Strengthening the Evidence Base.............................................................................................. 36 Table 19: Estimates for Burden of Disease for sub-Saharan Africa, 2002 ........................... 36 Table 20: Longitudinal Survey Programs ............................................................................. 38 Conclusion .................................................................................................................................... 39 Annex 1: Maternal Mortality in India ........................................................................................... 40 Annex Table 1: MMRs and Other Indicators for Indian States ............................................ 41 Annex 2: Country-Level Data Table............................................................................................. 42 References ..................................................................................................................................... 46 2 Introduction Every year more than half a million maternal deaths and around four million perinatal deaths occur in low and middle-income countries, mostly among the poorest groups within these countries. There is an even larger toll of morbidities (more than 8 million each year according to Koblinsky et al., 1993) resulting from non-fatal complications of delivery. Most of these deaths and disabilities are preventable, and the interventions required to prevent them are known. The sad reality is that in many instances these interventions are either not available to poor women or so poor in quality that they are ineffective. Other reports in this series address the “what” and “how to” of health care interventions to prevent maternal and neonatal mortality and morbidity. This paper focuses on the obstacles that prevent poor women from benefiting from the knowledge and technical expertise that is available, and on the factors beyond care that shape maternal and neonatal health (MNH) outcomes. It employs an adapted version of the “Pathways” framework from the World Bank’s guidelines for Poverty Reduction Strategy Papers to link factors at various levels—from individuals, households and communities to government policies in health and other sectors— that directly or indirectly affect MNH outcomes. The paper begins with an explanation of what the Pathways framework is and how it will be used to guide this discussion. That is followed by a brief discussion of measurement issues and by a review of cross-national evidence about linkages between factors identified in the Pathways framework and MNH outcomes. More detailed country-level evidence on factors at each of the levels (households and communities, health and other sectors, policy) will then be reviewed, leading to recommendations for actions that could be taken to address obstacles at each of these levels as well as research needed to strengthen the evidence base to assess the impact of these actions. In adapting the Pathways framework to MNH outcomes, the paper draws on other frameworks that have focused specifically on contextual factors affecting maternal health outcomes, for example the one developed by the Prevention of Maternal Mortality collaborators at Columbia University and in West Africa (McCarthy and Maine, 1993; Thaddeus and Maine, 1994; McCarthy, 1997) as well as broader frameworks that address a range of health outcomes (for example, Hanson et al., 2003). These frameworks address the role of household and communitylevel variables on outcomes.2 The Pathways Framework The chart below depicts a simple framework for assessing the impact of factors inside and outside the health system that influence health, including MNH, as shown in the left-hand column of the chart. These factors operate at three levels, shown in the other three columns of the chart: (1) households and communities, (2) the health system (including health care, health finance, health promotion) and sectors other than health such as education, infrastructure (water and sanitation, transport and communications) that indirectly influence health outcomes, and (3) 2 The framework for addressing obstacles to access to priority health interventions developed by Hanson et al. (2003) has five levels that parallel those in the Pathways framework used here: (1) communities and households; (2) health service delivery; (3) health sector policy and strategic management; (4) cross-cutting public policy; and (5) environmental and contextual characteristics. 3 public policies and actions that affect health systems and outcomes directly (health reforms, for example) or indirectly (macro-economic policies). Pathways to MNH Outcomes Health Outcomes MNH outcomes Households/ Communities Household behaviors & risk factors Household assets Community factors Health system & other sectors Government policies & actions Health care Health finance; health promotion Supply in related sectors Health policies Policies in other sectors Households and Communities: Good health is dependent not only on the provision of good medical services when required but also on healthy behavior. Healthy behavior means avoiding or minimizing risks (e.g. practicing family planning and safe sex) and requires knowledge about how to prevent disease and promote health and the ability to act on this information. Many health-promoting behaviors (for example dietary habits, sanitary practices, fertility regulation, childcare, and utilization of health services) take place within families. Such behaviors are often related to ‘household assets’ such as income, education, access to health services, roads and communication, membership in formal and informal support networks, as well as general knowledge and information. Health too is itself a household asset. Economists view these household-level determinants as demand-side factors, as opposed to the supply of health care (Ensor and Cooper, 2004). Economic research has tended to treat all members of a family, or household, as a single unit, assuming that whatever benefits one member will benefit the entire household. This is clearly not the case in reality, as it is widely acknowledged that intra-household differences in gender and age may significantly affect how decisions are made and whether a decision is beneficial for all members (Case and Deaton, 2002). Thus an understanding of household decision-making is critical to an understanding of how policy decisions affect the welfare of families as a unit or of individual members within them. Gender disparities in access to education, credit and political influence have considerable impact on how individual family members are valued and on the degree to which women as well as men 4 have a voice in household decision-making. Recognition of the importance of individuals and households in producing good (or poor) reproductive health outcomes should lead policy makers to focus on the constraints faced by vulnerable households and vulnerable members within those households. Household-level behaviors and risk factors are influenced and reinforced by conditions in the community (Tinker, 2000). Community factors include both the values and norms that shape household attitudes and behaviors and the physical and environmental conditions of the community, for example terrain and weather conditions that affect households’ capacity to produce better outcomes. Community factors that typically influence health outcomes are: Gender norms, which are influenced by social and cultural values that shape the roles of and relationships between men and women; Existence of effective community groups, social cohesion (sometimes called social capital) that support positive behaviors individuals and families or organize actions to improve health outcomes directly (community health insurance or pooling of resources to transport emergency cases) or indirectly (micro-credit programs); Community access to public services (inside and outside the health sector); and Environmental conditions (safe water, location—distance from a health facility, terrain, weather conditions). Health System and Other Sectors: The supply of health care and health information are key determinants of maternal and neonatal health outcomes for the poor. Since these interventions are covered in detail in other papers in the series, this paper will address two potential supplyside obstacles that may prevent poor women from benefiting from these services. These are: (1) financial obstacles including fees and/or coverage of critical services in insurance benefit packages; and (2) the organizational and institutional obstacles to scaling up effective interventions so that poor women can access them. Actions in other sectors also affect health outcomes, for example: Education, either formal education or training that enhance earnings capacity of household members as well as their capacity for effective health-seeking behaviors; Transport and infrastructure, for example the availability of services and the quality of roads that can affect travel time when a mother requires transport for management of an obstetric emergency; Energy and communications, for example coverage in a cell-phone network so that help can be sought it an emergency; Water and sanitation, important for avoiding infections; and Nutrition. Government Policies and Actions can affect both the health system and related factors in other sectors. Most countries have undertaken reform as a way to profoundly change the fundamentals of the health sector including changes in organization and accountability, revenue generation allocation and purchasing, as well as regulation. Government policies and actions in other sectors also affect health because of their influence on attitudes and behavior and the supply of related services such as education, transport, water and food security. Fees for schools and health services are examples of public policies that may have an indirect effect on MNH 5 outcomes. Taxation may also be a strong influence on health, for example “sin taxes” on tobacco or alcohol. Data on MNH and Poverty Data and Measurement Issues The paper utilizes cross-national estimates of maternal mortality from the WHO/UNICEF/UNFPA database prepared by AbouZahr and Wardlaw (2003). Estimates are provided for 172 countries and are derived from a variety of sources, including vital registration systems, direct and indirect estimating methods based on survey and census data, and statistical modeling for the 62 countries for which no national data on maternal mortality were available. This paper focuses on 142 countries in the World Bank's low and middle-income categories, and most of the 62 countries with estimated maternal mortality ratios (MMRs) are in those categories. The fact that statistical modeling was used to estimate MMRs creates some major limitations for the analysis of cross-country differences, because many of potential explanatory variables (fertility rates, GDP per capita, percentage of births assisted by a skilled attendant, and regional dummy variables) have been used to estimate the proportion of deaths that are considered “maternal” in country-level model life tables. The authors of the estimates emphasize that they should not be used for trend analysis and urge caution in cross-national comparisons for the reasons just stated. Cross-national data on neonatal mortality rates (NMRs : deaths of liveborns during the first 28 days of life per 1000 live births) are from a compilation published in the State of the World’s Newborns 2001 (Save the Children, 2002). Data for other cross-national indicators (per-capita income, poverty, education, transport, governance, etc) are taken from the World Bank’s World Development Indicators 2003, UNDP’s 2003 Human Development Report, and other sources (see Annex 2). In addition to cross-national comparisons and analysis, the paper will examine country-level tabulations of key indicators from the Demographic and Health Surveys that have been tabulated using a composite ‘household asset’ measure to show rich-poor differences in those indicators by wealth quintiles (Gwatkin et al, 2004). Additional evidence from country and topic-related studies will also be employed to fill out the picture of how factors beyond care may directly or indirectly impact on MNH outcomes for the poor. Regional and Cross-National Differences Global, regional and country-level estimates of maternal mortality (Table 1) show a clear connection between high maternal mortality ratios (MMRs) and poverty. More than 99 percent of maternal deaths occur in developing regions, and more than 85 percent occur in the poorest countries of Sub-Saharan Africa and South Central Asia. Country-level estimates show that more than a quarter of those deaths occurred in India, and that several other poor countries in these two regions (Bangladesh, Ethiopia, the Democratic Republic of Congo, Nigeria, Pakistan, Tanzania) account for another quarter of them. The highest maternal mortality ratios are found in poor countries in Sub-Saharan Africa. With the exception of Afghanistan, all of the countries having maternal mortality ratios of 1000 or higher are found in Africa. 6 Table 1: Comparison of 1995 and 2000 Regional and Global Totals Region 2000 Maternal Maternal Mortality Ratio deaths (000s) 400 529,000 20 2,500 28 2.2 440 527,000 830 251,000 130 4,600 920 247,000 330 253,000 55 11,000 520 207,000 210 25,000 190 9,800 190 22,000 240 530 WORLD TOTAL DEVELOPED REGIONS* Europe DEVELOPING REGIONS Africa Northern Africa Sub-Saharan Africa Asia Eastern Asia South-central Asia South-eastern Asia Western Asia Latin America & the Caribbean Oceania 1995 Maternal Maternal Mortality Ratio deaths (000s) 400 515,000 21 2,800 36 3.2 440 512,000 1,000 273,000 200 7,200 1,100 265,000 280 217,000 60 13,000 410 158,000 300 35,000 230 11,000 190 22,000 260 560 Includes Canada, United States of America, Japan, Australia and New Zealand, which are excluded from the regional averages. Data on neonatal mortality appear to be even scarcer than those for maternal mortality. Regional patterns for neonatal mortality (Table 2) are very similar to those for maternal mortality. Africa and South Asia account for over 93 percent of global deaths. Table 2: 2001 Global and Regional Estimates of Neonatal Mortality Region Number of live births (1000s) Neonatal deaths (1000s) Neonatal death rate (per 1000 live births) 42 34 46 21 17 Africa Asia* South-Central Asia Other Asia Latin America and the Caribbean Pacific Islands* Europe North America More Developed Countries Less Developed Countries Global 28,865 76,090 38,442 37,648 11,553 1,205 2,561 1,757 804 196 225 7,374 4,098 13,045 8 44 18 65 34 6 4 5 116,550 3,970 34 129,596 4.035 31 * Japan, Australia and New Zealand are included with the More Developed Countries but not in the regional sub-estimates. Source: Save the Children, 2002 Death rates are highest in the South Central Asia region, at 46 per thousand live births, followed by Africa, with 42. The rate is lower for the Other Asia group because China is included there and has a substantially lower neonatal death rate (23), compared to much higher rates for the large countries in South Asia—Bangladesh (48), India (43), and Pakistan (49). While the Pacific Islands account for a small proportion of neonatal deaths, their NNM rate is comparatively high. 7 Poverty Linkages Measuring maternal and neonatal mortality for sub-groups of the population within countries is even more challenging than country-level estimates. Graham and colleagues have developed a technique for estimating rich-poor differentials in maternal mortality using Demographic and Health Survey (DHS) data for 10 countries (Burkina Faso, Chad, Ethiopia, Indonesia, Kenya, Mali, Nepal, Peru, Philippines and Tanzania) with large sample sizes using wealth-quintile methodology developed at the World Bank (Graham et al, 2004; Gwatkin et al, 2004). In the country with the largest sample size and also with two surveys, Indonesia, they found that the poorest quintile accounted for one-third of all maternal deaths in both surveys, compared to fewer than 13 percent of deaths in the richest quintile. They also found a high level of association between the survival status of women and poverty status in all of the countries, and a highly significant correlation between education and survival status. Table 3: Attendance at Delivery by a Medically Trained Person by Wealth Quintile Region East Asia Europe/Central Asia L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average No. of countries 4 6 9 4 4 29 56 Regional average 53.6 94.9 66.0 52.5 21.5 43.5 51.6 Poorest quintile 26.6 88.4 43.2 33.6 7.0 24.2 32.7 Richest quintile 90.4 99.2 93.3 80.3 56.7 77.1 81.7 Poor/rich difference 63.8 10.8 50.1 46.7 49.7 53.4 49.1 Source: Gwatkin et al, 2004 It is also possible to get a sense of rich-poor differences for other countries (56 in all, including the 10 for which MMRs by wealth quintiles have been calculated) by using the same DHS data for countries on deliveries attended by medically trained persons. This indicator is known to be highly correlated with both maternal and neonatal mortality (and has, in fact, been used to estimate the proportion of maternal deaths in countries lacking other maternal mortality data). Table 3 shows a 49 percentage point difference in the proportion of skilled attendance between the richest and poorest quintiles for all 56 countries for which the tabulations have been made— with the poorest quintile averaging 32.7 percent compared to 81.7 percent for the richest quintile. Rich poor differences are greatest (64 percentage points) in East Asia, though only four countries are included in the tabulations (Cambodia, Indonesia, the Philippines, and Vietnam) and least (11 percentage points) for Europe/Central Asia (six countries: Armenia, Kazakhstan, the Kyrgyz Republic, Turkey, Turkmenistan, and Uzbekistan). That region also has the highest average level of attendance, 88 percent. South Asia (four countries: Bangladesh, India , Nepal and Pakistan) has the lowest overall level of skilled attendance, 21.5 percent and a 49.7 percentage point poor-rich differential. Latin America has the second highest overall level of skilled attendance (43 percent), but also a comparatively high (50 percentage point) differential between the rich and the poor. Sub-Saharan Africa has a higher overall average for attended deliveries (43.5 percent) than South Asia, which is puzzling given the MMR estimates for Africa. DHS data are available for 29 countries in Africa, suggesting that the issue may be poor quality of delivery care rather than under-representation of regional experience in the tabulations. Richpoor differences are in the middle range (53 percentage points) in Africa, though attendance for the poorest quintile (25 percent) is second lowest in the tabulations after South Asia. The Middle 8 East/North Africa (MENA) group (four countries: Egypt, Morocco, Jordan, Yemen) is in the middle of the range in terms of the regional average (52.5 percent) and rich-poor differential (46.7 percentage points). Another way of looking at the poverty link is to group countries by MMR level and then compare them to average levels of per-capita GNP and other indicators in the Pathways framework (female school enrollment, gender equality, paved roads, and governance).3 In Table 4, 142 low and middle-income countries are divided into five broad MMR groupings (0-30, 31100, 101-300, 301-1000, over 1000). GDP per capita for the group with the lowest MMRs exceeds $10,000 (dollars in purchasing power parity terms—PPP), compared to just over $1,000 for the countries with the highest MMR levels, a ratio of greater than ten to one. Public health expenditures per capita (also in PPP dollars) are more than ten times greater ($315) in the low MMR group compared to the countries with the highest MMRs ($23). Table 4: Averages of Pathways Indicators for Countries Grouped by MMR Level MMR Level Number of countries 0-30 31-100 100-300 301-1000 Over 1000 17 39 32 41 13 GDP per capita (PPP$) 10,629 6,952 4,760 1,610 1,025 Public health spending per capita (PPP$) 315 168 118 30 23 Female school enrollment % UNDP gender Index 72 74 70 43 31 .82 .79 .70 .48 .37 Paved Roads % 79 59 37 43 31 Effective governance 0.41 -0.07 -0.35 -0.37 -1.08 Source: See Annex 2 Linkages with Other Factors Large differences between the lowest and highest MMR groups are also seen for other indicators. Female enrollment rates4 for the lowest group are more than twice as high as for the highest group. The same is true for UNDP’s index of gender equality that combines a range of genderrelated indicators (where 1 is the top score). Countries with the lowest MMRs score more than twice as high as those with high MMRs. A difference in the patterns for female school enrollment and gender equality is that the first three MMR groups (those lower than 300) show little variation in the three indicators, while countries with MMRs greater than 300 have significantly lower levels. There are also large differences between the low and high MMR groups for the percentage of paved roads and effective governance scores. For the low MMR group, 79 percent of roads are paved, compared to 31 percent for the high group. There is not the clustering among the first three groups that was seen for school enrollment and gender equality. In the case of governance scores (which can range from 2.5 as the best score to –2.5,the worst) the low MMR group has the only positive average score (.41), while the high MMR group average –1.08.5 The table shows simple averages. When population weighted averages were calculated, large countries like 3 Data for all 142 countries are found in Annex 2. The indicator is the combined percentage of females in relevant age groups enrolled in primary, secondary and tertiary levels of schooling. Data from UNDP 2003. Simple averages of the three enrollment rates from the World Bank’s World Development Indicators were used for countries not included in the UNDP list. 5 Data and an explanation of the governance score can be found in Kaufmann, Kraay and Mastuzzi, 2003. 4 9 China and India significantly outweighed the other countries in their groups. Further, some interesting patterns emerge if we examine the indicators for these two countries, along with several other large countries. Table 5 shows indicators for the eight most populous countries. Table 5: Pathways Indicators for Large Countries Country China Russian Federation Indonesia Brazil Bangladesh Pakistan India Nigeria 56 GDP per capita PPP$ 3,600 Public health exp. per capita (PPP$) 18 67 230 260 380 500 540 800 7,700 2,900 6,500 1,570 2,000 2,200 950 193 21 206 32 16 11 10 MMR Female school enrollment 62 82 63 97 54 27 49 41 UNDP gender equity index 0.72 0.77 0.68 0.77 0.50 0.47 0.57 0.45 22 Effective governance 0.18 67 46 6 10 43 46 31 -0.40 -0.56 -0.22 -0.53 -0.50 -0.13 -1.12 Paved Roads Gini Coef. 40.3 45.6 30.3 59.1 31.8 33.0 37.8 50.6 Source: See Annex 2 Countries are ranked by MMR level, with China the lowest and Nigeria the highest. China ranks in the middle in terms of per capita GDP, health expenditures, and paved roads but at or near the top on gender equity and governance, and also on income distribution, which is measured using the Gini coefficient.6 India, which, per capita, spends on health nearly two-thirds the per capita level of China, has an MMR rate almost ten times that of China and ranks next to last in MMR level, while Brazil, which spends most on health, has an MMR higher than Indonesia, which spends only a fraction of what Brazil does on health. Brazil has comparatively high levels of female school enrollment and gender equality but has a low percentage of paved roads (an a very large area to cover) and high-income inequality. India has a more equal income distribution but worse gender indicators. Among the three South Asian countries (Bangladesh, India and Pakistan), Bangladesh has the lowest MMR (though the decline, as recorded in the country’s maternal health survey, is relatively recent). Nigeria, with the highest MMR, is near the bottom on all indicators. Averages for the large countries can mask considerable geographic variation within countries. Several of India's states have larger populations than quite a number of countries in the global comparisons, and state-level data reveal large differences in the MMRs between the poorer northern and northeastern states and the more prosperous western and southern ones (see Annex 1 on Maternal Mortality in India). When we look at the Pathways indicators of individual countries in the highest MMR grouping (above 1000), a similar picture emerges. In Table 6, all eight countries have per capita GDP of $1000 or less, and all have very low levels of per capita health expenditure. With the exception of Malawi, female school enrollment is low. The gender equity indicator is available for only five of the countries and is low for them, as are the percentages of paved roads and index of Gini data from the World Bank’s World Development Indicators, 2003. The Gini coefficient ranges from 0 - 100, with 100 indicating the worst inequality. Gini data were not available for many of the 142 countries in the larger list, so averages were not calculated for this indicator in the previous table. 6 10 government effectiveness. For the last indicator, income inequality, Sierra Leone has the highest level of income inequality and also the highest MMR, while the other countries on this list have low to middle levels of inequality. Table 6: Pathways Indicators for Countries with Highest MMRs Country MMR Mali Rwanda Tanzania Niger Angola Malawi Afghanistan Sierra Leone 1,200 1,400 1,500 1,600 1,700 1,800 1,900 2,000 Source: See Annex 2. GDP per capita (PPP$) 850 900 710 1,000 1,000 900 800 510 Public health exp. per cap. (PPP$) 15 18 22 13 28 29 11 3 Female school enrollment 26 51 31 14 26 70 n.d. 44 UNDP gender equity index .33 .42 .40 .48 n.d. .38 n.d. n.d. Paved Roads 12 8 4 8 10 19 13 8 Effective governance -0.84 -0.82 -0.51 -0.79 -1.16 -0.68 -1.39 -1.54 Gini Coef. 50.5 28.9 38.2 50.5 n.d. 50.3 n.d 62.9 n.d. means no data available While these comparisons of countries by MMR groups show a general pattern of poor indicators for the high MMR group and good indicators for countries with low MMRs, they do not always show a smooth progression of indicators from the low to high groups – as illustrated by the roughly equal levels of female school enrollment in all three groups of countries with MMRs below 300 and by individual country comparisons such as India, with a higher MMR than China even though India has a higher ratio of paved roads. Cross-National Analyses. As noted earlier, statistical analysis of cross-national differences in MMRs is problematic because many of the measures that one would like to use to explain cross-country differences (per capita GDP, contraceptive prevalence, percent of deliveries with skilled attendant) have been used to compile the estimates, so that correlations with these variables would be high and reflect the estimating algorithm. However, correlations between MMRs and the Pathways variables in Table 7 (which are not embedded in the MMR estimates, though correlated with them) are also negative and highly significant. The strongest correlation is with public health expenditures, though there are also significant relationships with education and gender equality, government effectiveness, paved roads and safe water. Table 7: Correlations between Pathways Variables and MMRs Variable Per capita public health expenditures (log) Female school enrollment (percent of school age pop) Gender equality index (1=maximum) Number of observations 142 Mean 4.12 Correlation with MMR -.733 140 60.4 -.661 116 .64 -.878 11 Percentage of paved roads Government effectiveness Safe water (percent of households) 140 41.4 -.701 139 -.35 -.574 140 75.8 -.615 Source: See Annex 2; all correlations are significant at the .01 level. A similar pattern appears when neonatal mortality data are grouped by level (Table 8) for the indicators. These data are available for only 100 countries, with fewer richer countries as is clear when looking at the group with the lowest NNM rates (0-10), for which the average GDP per capita is $7,734 compared to an average of $10,629 for the lowest MMR group. Table 8: Averages of Pathways Indicators for Countries Grouped by Neonatal Mortality Rate NNM level Number of countries 0-10 11-20 21-30 31-40 Over 40 22 19 22 16 21 GDP per capita (PPP$) 7,534 5,461 5,116 1,458 1,365 Public health spending. per cap. (PPP$) 256 124 77 35 17 Female school enroll-ment 74 71 66 47 36 UNDP gender index .88 .73 .59 .46 .43 Paved Roads 62 43 48 25 18 Effective governance +.15 -.22 -.27 -.74 -.76 Source: See Annex 2 For the 21 countries with the highest NNM rates (over 40), average per capita GDP ($1,365) is less than one-fifth that of the low NNM group. Public health expenditure per capita falls off more steadily than GDP per capita. The education/NNM pattern is similar to the one for MMRs, with the first three groups having higher rates than the two lower groups, while the remaining three indicators decline steadily as the NNM levels rise. Overall, the relationships between the NNM groups and the Pathways indicators are quite similar to those for the MMR groups. Analytical work by World Bank researchers on what would be required to attain the Millennium Development Goals in health has focused on these relationships using multivariate regression techniques to study cross-national variation in the WHO’s 1995 maternal mortality estimates (Wagstaff and Claeson, 2004). One of their main findings is that if interventions that are known to be effective (skilled attendance at delivery, effective referral and management of obstetric emergencies) could be increased from current levels to 99 percent, nearly four-fifths of the 529,000 maternal deaths that occur each year might be averted. The authors and also address the question of how to ensure that these interventions are implemented, particularly in ways that benefit poor women whom they are not now reaching. A key question is whether additional government spending would help. One school of thought holds that added government spending is likely to have little effect because of corruption and the poor management of public services, but the authors of this study take the view that added government spending could make a difference provided it is combined with improvements in governance and is effectively targeted on the poor. They also call attention to the key role of households, both as consumers of health services and as producers of health outcomes, in ensuring that increases in delivery care will actually reduce maternal mortality and morbidity. 12 The study employed a simulation modeling process to project possible impacts of increased government spending and improvements in government effectiveness as well as changes beyond the health sector (added economic growth, increased education, improved water supply) on achievement of the maternal mortality reduction target of the Millennium Development Goals. The results are summarized in the chart below. For each of the World Bank’s regions (the same regional breakdown as shown in the DHS tabulations), the chart shows the rate of decline in MMRs from 1990 to 2000 (labeled “current” with darker shading at top of bars) and the added decline that could occur (lighter shading at bottom of each bar) if an additional 2.5 percentage points were added to the annual growth of government health spending as a percentage of GDP, provided that countries achieve a level of effectiveness in governance that is one standard deviation about the mean of cross-national scores in the World Bank’s Country Policy and Institutional Assessment (CPIA) data.7 The chart also shows (in the cross-hatched area in each bar) the potential contribution of “extra-sectoral contributions” - added economic growth, better roads, quicker growth in female secondary schooling, and improved access to drinking water. Finally, the chart shows the rates of decline between 1990-2015 required in order to meet the regional MDG goals for reduced maternal mortality (the black line across the graph–5.75 percent annually) and rates that would be required between 2000 and 2015 for regions whose declines were below the required level during 1990-2000 in order to catch up and reach the 2015 goal (the small black squares in the bar). Comparing the simulated results by region, the chart shows that only one region (the Middle East and North Africa) experienced declines in the MMR during the 1990s at a rate that would enable 7 The model is based on cross-national regression analyses MMRs with the percentage of GDP expanded on health, along with other variable including government effectiveness, female education and water supply. The methodology and regression analyses are explained in Annex 2 of Wagstaff and Claeson, 2003. 13 them to reach the 2015 MDG goal. All of the others need higher rates of increase during 20002015 in order to catch up. In three regions (Europe/Central Asia, South and East Asia) a combination of extra-sectoral contributions and additional government health expenditures would bring the rate of decline up to the require level, but in two regions (Sub-Saharan Africa and Latin America/Caribbean) the combination would not bring the rate up to the required level. In the case of SSA, the projected impacts are just too weak to have an impact, and in LAC, the levels of extra-sectoral contributions are currently high enough that added change does not appear likely (though compared to other regions, MMR levels in LAC are already low). This pessimism about the prospects for SSA has been countered by Jeffrey Sachs and his colleagues at the Millennium Project, who recognize that governance issues have inhibited efforts to reduce poverty in Africa but argue that the region suffers from a "poverty trap" stemming from geopolitical and environmental problems. To escape from this trap, countries need substantially larger investments in physical and human capital (Sachs et al, 2004). The Millennium Project calls for massive increases in donor financial support to poor countries in Africa. Critics of this recommendation caution that the effort is likely to run into substantial bottlenecks in absorbing and effectively utilizing large increases in funding. The problems arising from shortages of health personnel to scale up HIV/AIDS treatment is a case in point (see Marchal et al, 2004). In making the case for increased health expenditures, the World Bank authors emphasize that they are talking not about across-the-board increases in expenditures but about targeted expenditures to increase the quality and accessibility of the key interventions needed to reduce the high maternal mortality ratios experienced by poor women. The report notes two promising approaches to such targeting. One of these is Marginal Budgeting for Bottlenecks (MBB), which targets added health expenditures on bottlenecks in health system performance. The second is financing through Social Funds, which are targeted on improving the demand and capacities of poor localities and households where these interventions need to occur. MBB was developed by UNICEF, the World Bank, and WHO in conjunction with efforts to ensure that funds created by debt relief actually benefit the poor (Soucat et al, 2004). It involves the formulation of national or provincial-level medium expenditure plans that allocate newly available resources to achieve an MDG like reduced MMR. MBB starts by using proxy indicators from Demographic and Health Surveys and other data sources to identify potential bottlenecks in five broad categories: (i) gaps in physical accessibility, (ii) human resource bottlenecks, (iii) constraints related to supplies and logistics, (iv) demand and utilization constraints, and (v) bottlenecks due to technical and organizational quality. In Mali, for example, the proportion of deliveries attended by trained staff was used as a performance measure and a costing and budgeting program was developed to reach an attended delivery “performance frontier.” An epidemiological model was calculated to measure and then monitor the impact of increased expenditures on reaching this frontier. Social Funds (SFs) are “agencies that finance small projects to benefit a country’s poor and vulnerable groups.” Projects are subject to specific eligibility criteria and are generated and managed by communities (Wagstaff and Claeson, 10). Evaluations of SFs in several countries have shown them to be effective mechanisms for channeling funding to poorer communities and improving both the demand for and quality of health services. In Bolivia, for example, it was reported that medicines and essential drugs were more available in SF facilities and, by going 14 beyond traditional approaches to investment in infrastructure, the SF raised the utilization of services and contributed to a reduction in under-five mortality rates in SF communities (Newman et. al, 2002). An evaluation of the impact of social funds on health in four countries (Bolivia, Honduras, Nicaragua and Zambia) found that social fund health interventions had a positive impact on infrastructure quality and on the availability of medical equipment, furniture, and essential drugs. This, in turn, increased utilization of these facilities for critical services, including maternal and child health (Rawlings et al, 2004). Review of Evidence on Pathways Variables Other Reproductive Health Risk Factors Fertility and Contraceptive Use: High fertility rates and low levels of contraceptive use are associated with poor maternal and neonatal health outcomes. Studies show that a woman’s chances of dying as a result of pregnancy and delivery are affected by her age and parity (Maine et al, 1994). Short birth intervals are associated with higher neonatal mortality (Population Reports, 2002). While data on these associations are widely available, the causal relationships underlying these linkages, both biological and social, have proved to be more difficult to untangle. Poor women generally have higher fertility and lower rates of contraceptive use than non-poor women. Tabulations by wealth quintiles of Demographic and Health Surveys data carried out during the late 1990s for 56 countries provide supporting evidence. Table 9 shows regional averages in poor/rich differentials in the total fertility rate (rates for the poorest and richest quintiles and the difference between the two) from these tabulations. Overall, women in the poorest quintiles average nearly 3 more children than women in the richest quintile, with the largest difference occurring in Latin America/the Caribbean and the lowest in the Europe/Central Asian region. Table 9: Total Fertility Rates by Wealth Quintile and Region Region East Asia Europe/Central Asia L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average No. of countries 4 6 9 4 4 29 56 Regional average 3.2 2.7 3.7 4.6 3.8 5.4 4.6 Poorest quintile 4.4 3.7 6.1 6.7 4.6 6.7 6.0 Richest quintile 2.0 1.8 2.2 3.9 2.6 3.9 3.2 Poor/rich difference 2.4 1.9 3.9 2.8 2.0 2.8 2.8 Source: Gwatkin et al, 2004 Poor/rich differences in fertility reflect similar patterns of differential use of modern contraception. Table 10 shows average rates of contraceptive use for women in the poorest and richest quintiles for the same regional groupings, along with the percentage point difference between those quintiles. The average difference between the contraceptive use rates for rich and 15 poor women is 18.6 percentage points for the 56 countries, with the largest differentials occurring in Latin America/Caribbean, South Asia, and the Middle East, while the smallest are in Europe/Central Asia and East Asia. Africa has the lowest overall prevalence and lower rates for most quintiles than the lowest quintile in other regions. Table 10: Contraceptive Prevalence by Wealth Quintile and Region Region East Asia Europe/Central Asia L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average No. of countries 4 4 9 4 4 29 56 Regional average 39.4 44.3 47.1 34.2 32.8 13.0 26.7 Poorest quintile 31.3 38.2 33.1 22.4 22.9 6.5 18.3 Richest quintile 41.8 48.1 56.8 45.0 45.8 25.1 36.9 Rich/poor difference 10.5 9.9 23.7 22.7 22.9 18.6 18.6 Source: Gwatkin et al, 2004 The two most commonly recognized factors linking fertility/contraceptive use and maternal/neonatal mortality rates are that risks are higher (1) when births occur at a very young age, and (2) when birth intervals are short. A third line of argument is that older, higher-parity women are more at risk. Rani and Lule (2004) analyzed DHS data for 12 poor countries and found young women from the poorest households were more likely than those from the richest ones to be married by age 18 and to have had at least one child by that age. These women were also more likely to have had a mistimed birth and were less likely to practice family planning, use maternal health services and have knowledge about prevention of sexually transmitted infections. Additional DHS tabulations of age-specific fertility rate for women aged 15-19 (Table 11) show that the rate for women in the poorest quintile is more than twice that of women in the richest group for 55 countries as a whole (Egypt was not included in this tabulation), and nearly five times greater for poor women in Latin America and the Caribbean. The poor/rich differential is lowest in the three MENA countries and in Europe/Central Asia and East Asia, which also have lower regional average rates. Table 11: Adolescent Fertility Rates by Wealth Quintile and Region Region East Asia Europe/Central Asia L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average No. of countries 4 4 9 3 4 29 55 Regional average 46.0 52.7 94.7 62.7 108.8 131.9 106.5 Poorest quintile 76.5 73.0 172.6 111.7 146.3 169.6 148.6 Richest quintile 15.8 31.3 36.9 99.0 56.0 79.5 62.6 Poor/rich difference 60.8 52.7 135.7 12.7 90.3 90.0 86.1 Source: Gwatkin et al, 2004 Research on the links between early childbearing and poor maternal and neonatal health outcomes have concluded that most of the adverse health consequences (delivery complications and maternal mortality, prematurity and higher perinatal death rates) of teen pregnancy are associated more with socioeconomic factors than with the biological effects of age (Makinson, 16 1985; Miller, 1991). These studies are for populations in richer countries. For developing countries, women aged 15-19 are twice as likely to die from childbearing as women in their 20s, and women under age 17 face especially higher risk. Young women who become pregnant are at risk of obstructed labor if they have not grown to their full height or pelvic size, and are also more likely to suffer from eclampsia, which threatens them and their babies (Upadhyay and Robey, 1999). In her review of research on the consequences of adolescent childbearing in India, Jejeebhoy (1996) reports that infants of adolescent mothers are more likely to suffer higher perinatal and neonatal mortality, that levels of anemia and complications of pregnancy are higher for adolescent mothers, but that they are less likely to obtain antenatal care and trained attendance at delivery than older mothers. Births that are too closely spaced are also associated with higher perinatal mortality, and may be a risk factor for maternal mortality (Miller, 1991). Infants whose births were spaced more than two years have been less likely to be premature or suffer from low birth weights. Analysis of DHS data for 18 countries (and encompassing more than 430,000 pregnancies) showed that children born three to five years after a previous birth are more likely to survive (Venugopal and Upadhyay, 2002). A cross-national study of 18 Latin American countries found that women with interpregnancy intervals of less than six months had a higher risk of maternal death and complications of delivery than those conceiving at 18 to 23 months, and also that intervals greater than 59 months were associated with higher risks of eclampsia (Conde-Agudelo and Belizan, 2000). The association between short birth intervals and poor maternal and neonatal health has been ascribed to the so-called “maternal depletion syndrome,” in which maternal nutrition plays a critical role (Winkvist et al, 1992; King, 2003). As the biological competition for nutrients increases during pregnancy, an inadequate supply contributes to poor fetal development and may also be factor in higher maternal mortality. King found that “maternal depletion of energy and protein resulting from short inter-pregnancy intervals or early pregnancies leads to a reduction in maternal nutritional status at conception and altered pregnancy outcomes” (King, 2003: 1735s). While there is a biological basis for the close associations between early or too closely spaced pregnancies and poor maternal and neonatal health, causal explanations need to address the possibility that other factors may influence both at the population level. In a study for rural Bangladesh on the relationship between childbearing and maternal survival, Menken and colleagues found no significant effects of early or closely spaced pregnancies on these outcomes once other factors (education, height) were controlled. But while there were no significant differences in the risk of dying during delivery between births that were early, closely spaced, or numerous, their findings do suggest that lifetime childbearing does affect a woman’s survival chances. “Each time a women has a child, she faces an increased risk of dying in the relatively short period (two to three years) after that birth. Thus a woman who bears seven children has seven chances of succumbing to this risk, whereas a woman who bears two children has only two chances” (Menken et al, 2003). The authors refer to this as “extended maternal risk”. Their findings complement earlier work by Ronsmans and Campbell (1998) who found no evidence that short birth-to-conception intervals affected the risk of maternal mortality. The interplay of biological and contextual factors is also emphasized by Zabin and Kiragu (1998) in their review of the health consequences of adolescent sexual and fertility behavior in SubSaharan Africa, in which they document the “immense reservoir of suffering cause by childhood 17 marriage and immediate post pubertal childbearing among girls given in marriage at ages as young as ten or 12.” They emphasize that analysis of the role of age in these adverse outcomes should also take into account other proximate causes and cite two examples: radical forms of circumcision and cephalopelvic disproportion, which is a factor in obstructed deliveries and which, if not adequately managed, can cause obstetric fistulae. Circumcision often leaves so much scar tissue that that the first child is lost - this health effect is related to age because teenagers are more likely to be primiparous than older women but could still occur if childbearing is delayed to a later age. Cephalopelvic disproportion occurs more frequently among malnourished young girls whose bone development is incomplete, leading the authors to conclude that “the root causes of this sort of tragic delivery are malnutrition and a lack of access to or use of professional care”. Unintended Pregnancies and Abortion: In addition to the risks associated with the number and spacing of births, there are those associated with unintended pregnancies, including those that are unwanted and those that are mistimed. While interpretation of data on pregnancy intentions continues to be debated, they have proved to be valuable in addressing pregnancy-related health risks. Women with unintended pregnancies are less likely to seek prenatal care, more likely to use alcohol and tobacco during pregnancy, and more likely to suffer physical abuse and violence (Santelli at al, 2003). Many unintended pregnancies end in abortion. Where abortion is safe, abortion-related mortality and morbidity are lower than birth-related mortality and morbidity. However, WHO estimates that 20 million unsafe abortions occur annually, mostly in developing countries. This means that one out of ten pregnancies is terminated by an unsafe abortion, with a ratio of one unsafe abortion per seven live births. South Central Asia accounts for the largest share of unsafe abortions, followed by Africa and Latin America (Ahman et al, 2003). Unsafe abortion is a significant cause of maternal mortality and morbidity. Nineteen million unsafe abortions are estimated to have taken place during the year 2000, 98 percent of them in developing countries. Over the period 1995-2000, an estimated 78,000 maternal deaths, approximately 13 percent of all maternal deaths, were attributable to unsafe abortion. AbouZahr and Ahman (1998) estimated that the abortion-related mortality risk was at least 15 times higher in developing areas and that in some regions it may be 40-50 times higher than in more developed regions. While unsafe abortion and abortion-related mortality risk are much greater in poor countries, comprehensive data on rich-poor differences in risk are not available. However, the fact that poor women have higher fertility and lower contraceptive use would imply that they are at much greater risk. There is also evidence, still incomplete, that the incidence of unsafe abortion and resulting mortality may be rising among unmarried adolescent women in urban areas of developing countries. Violence, Conflict and Refugee Settings: Mothers and children in conflict settings, including those who are refugees, are subject to greater risk of poor reproductive and neonatal health outcomes. UNFPA estimates that women and children account for 75-80 per cent of the world’s 37 million refugees and displaced persons at risk from war, famine, persecution and natural disaster; that 25 per cent of this population at risk are women of reproductive age, and that one in five is likely to be pregnant (UNFPA, 2001; Save the Children 2002). Maternal mortality for women in conflict zones of the Darfur region of the Sudan is higher than the already high national average of 1500 for the country as a whole (Collymore, 2004). 18 Women and children living in such circumstances are exposed to a range of risk factors, including gender-related violence, rape, poor nutrition, psychological trauma, abuses in camp settings, and a lack of access to basic health care. One of the “collateral” effects of conflict is the destruction or breakdown of basic services. Conflict also creates obstacles for relief agencies, further exacerbating health problems and making it difficult to measure outcomes. Reviews of available information on the reproductive health in war-affected populations identified a range of risk factors that depend on what was going on in specific settings at specific times (McGinn, 2003). Numerous case studies have documented deterioration in maternal and neonatal health indicators for refugees in conflict settings, including Congo, Guatemala, Sierra Leone, and Afghanistan (Ward, 2002). A 1999-2000 study of maternal mortality among Afghan refugees in Pakistan, revealed a rate was 50 percent higher than the rate for Pakistan (291 vs. 200), though lower than the estimate for Afghanistan itself (820). Most of the maternal deaths in camps were preventable and resulted from lack of access to emergency services (Bartlett et al, 2002). However, research on reproductive health in refugee camps in a number of countries (Sudanese and Somalis in Ethiopia, Sudanese and Rwandans in Uganda, Burundians and Congolese in Tanzania) found better outcome indicators (including maternal and neonatal mortality) than for refugees’ home countries or their host countries, suggesting that once reproductive health services are established in camps they can have a positive impact (Hynes et al, 2002). Research on the links between gender violence and reproductive outcomes shows that women who experience violence have poorer outcomes, including more unintended pregnancies, low birth weight, fetal wastage and infant deaths (Nasir and Hyder, 2003; Heise et al, 1999). While none of these reviews distinguished between poor and non-poor women in these conditions, it is safe to assume that poor women represent a significant, if not substantial proportion of the total. Violence in pregnancy is another risk factor and is a cause of poor delivery outcomes. Heise and colleagues (1999) report that violence in pregnancy accounted for 16 percent of low birth weight deliveries in Nicaragua, and that violence may be responsible for a sizeable but under-recognized proportion of pregnancy-related deaths on the Indian subcontinent. The risk of pregnancyrelated deaths associated with violence was substantially higher for pregnant teenagers than for other age groups. Infections and Other Risk Factors: In addition to malnutrition, other risk factors may also trigger or exacerbate obstetric complications (Koblinsky, 1995; Tinker, 2000). In addition to poor nutrition and violence (discussed above) these include infections (sexually transmitted infections and HIV/AIDS, malaria, tuberculosis, hepatitis), substance abuse, and harmful practices such as female genital mutilation (FGM). A major gap in many programs aimed at prevention of the transmission of HIV infection from mothers to children is treatment for mothers after they have delivered, since most programs seek to save the life of the child but not the mother - ignoring evidence that survival chances for children are lower for those whose mothers have died, not to mention the basic ethical issues involved in such choices. Some of the world’s highest MMRs are found in countries where the practice of FGM is widespread. Among the long-term consequences of FGM are increased risk of obstructed labor, delayed delivery, and increased risk of stillbirths (PATH, 1997). Another consequence is increase vulnerability to sexually transmitted infections (STIs) and HIV/AIDS. STIs are known to affect delivery and pregnancy outcomes, including premature birth and intrauterine growth retardation (Haberland et al, 1999). The link between HIV/AIDS and maternal mortality has been recognized in the latest estimates of MMRs, which include HIV prevalence in the 19 estimating equation for the proportion of deaths in reproductive ages that are considered “maternal”. In South Africa, where the HIV prevalence rate is one of the highest in the world, AIDS-related respiratory infections (pulmonary TB and pneumonia) are important factors in pregnancy-related mortality (Kruger, 2003). Malarial infection is another cofactor in pregnancy-related deaths of mothers and newborns. Meremikwu (2003) notes that malaria is typically a more severe disease in pregnant women and is a major contributing factor to maternal mortality in malarial areas of Africa. Malaria is associated with maternal anemia, which is another cofactor in maternal death. Santosi (1997) adds that malaria is associated with chronic health problems that frequently become acute during pregnancy and are associated with higher rates of maternal mortality and morbidity in malarial areas. Etard and colleagues (2003) report that malaria is a probably cofactor in seasonal swings in maternal deaths in Senegal. One of the reasons why Malawi’s MMR remains so high despite a comparatively high rating on education is its high prevalence of malaria (55-80 percent during the rainy season) along with severe anemia in pregnant women. 20 Table 12: Selected Findings on Other Reproductive Health Risks Country, location Latin America Bangladesh Type of study Citation Cross-national analysis Conde-Agudelo and Belizan (2002) Matlab surveillance data Menken et al. (2003) Global Reviews Africa Review Refugee populations Reviews Africa Reviews Ronsmans and Campbell (1998) Santelli et al (2003) Ahman et al (2003) Zabin and Kiragu (1998) McGinn (2003), Ward (2002), Heise et al (1999) PATH (1997), Kruger (2003), Meremikwu (2003) Findings Women with interpregnancy intervals of 5 months or less had higher risks for maternal deaths and complications; women with intervals greater than 59 months had higher risk of eclampsia. No significant effects of early or closely spaced pregnancies once other factors (education, height) controlled; however, the overall number of deliveries affects survival chances No evidence that short birth-to-conception intervals increase maternal mortality Unwanted pregnancy and unsafe abortion contribute to high MMRs, even in countries where abortion is legal. Biological and contextual forces interact in determining the adverse effects of adolescent sexual and fertility behavior; malnutrition and lack of access to care exacerbate these problems, which affect both married and unmarried adolescents Refugees and women who experience violence experience worse MNH outcomes; RH services for refugee populations can mitigate these risks. Harmful practices (FGM) and infectious diseases (TB, malaria and HIV/AIDS) increase the risks of obstetric complications and higher MNM rates. Household and Community Factors As noted in the introduction to the Pathways framework, households and communities are important but often-neglected actors in the effort to improve maternal and neonatal health outcomes. Building on the Pathways framework, the World Bank analytical report on the achievement of MDGs described in the previous section looked at households both as consumers of health services and as producers of health outcomes. The report cited two main obstacles that accounted for underutilization of key health interventions by poor households: (1) the prices that households pay for those interventions; and (2) lack of knowledge about those interventions and their importance to the health of the household members. In addition, the Pathways framework recognizes that intra-household relationships, particularly gender relations, affect utilization patterns. Gender deserves special attention because of the inequity in social relationships that restricts the rights of women to make decisions for themselves or to have fair access to household assets; and the greater the inequity, the greater the obstacle to poor women’s access to life-saving interventions. In Indonesia, women’s control over assets, which were found to be highly correlated with education, positively affected their chances to get prenatal and delivery care (Beegle et al, 2001). The authors note that while the government has made progress in reducing price and distance barriers to obtaining care, the inequitable distribution of power in social relationships remains a significant obstacle. Another Indonesian study based on interviews about 21 the circumstances surrounding more than 100 maternal deaths found “many families whose personal poverty excludes them from even considering attempts to gain access to emergency obstetrical care” and characterized these women as “too poor to live” because families failed to take steps to seek care for complications because they feared the cost could be greater than they could bear (Islander et al, 1996: p. 80). The case study in Box 1 illustrates household and community level obstacles that prevent poor women from obtaining life-saving interventions when they suffer an obstetric complication. The case is taken from an oral autopsy that was conducted in Bangladesh during the early 1990s and which played an important role in shaping the development of a maternal health strategy for Bangladesh later in that decade (Blanchet, 1991). It describes the plight of a poor woman who died as a result of complications during her tenth delivery. While the midwife diagnosed her condition as “extreme anemia”, and the symptoms also suggest septicemia (once a leading cause of maternal deaths, but now rare in richer countries), the case reveals much more about the complex weave of causes of Safar Banu’s death. What we observe is a complex interplay of forces that undermined Safar Banu’s survival chances, as well as those of poor women around the world, in the face of life-threatening obstetric emergencies. These include: Her subordinate status in the household, and her willingness to endure this; The fact that she was not using contraception, and that she had no voice in this despite her concerns about having a tenth child; Her poor nutritional status (being the last and least fed in her household); The lack of prenatal care despite her experiencing swelling and dizziness; The fact that the household could not afford to pay for medicines; The husband’s reliance on the advice of the traditional healer, who failed to provide adequate care, and his refusal to listen to the midwife; The misinformation about her condition among those around her, which delayed treatment at the clinic; and Transport costs, for which the family had to sell land (creating a legacy of resentment) and which caused further delay in her treatment. No single factor was the “cause” of her death, but the combination of circumstances described in the case capture many of the household/community-level factors mentions earlier: gender relationships in the household, household behaviors relating to fertility regulation and nutrition, lack of information, and household poverty and inability to pay for care. Further discussion of the cost issue is found in the next section, which addresses health system failures. 22 Box 1: Why did Safar Ban Die? Safar Banu, age 43, never attended antenatal clinic. She said she had already given birth to nine children without the help of a clinic. Why should she need antenatal checkups now? She was too busy and had no time for such visits. When several months pregnant, she worked in the fields shredding jute fibers. Such work is usually performed only by the poorest women. Safar Banu did not use contraceptives. She wished to, but her husband forbade her and threatened to divorce her if she did. According to her mother, when Safar became pregnant for the tenth time, she was sorry and cried. The pregnancy itself did not present special problems, but during the last month, Safar complained of swollen feet and dizziness. A week before giving birth, she felt very weak and told her mother she feared she would not survive this birth. At the time, her anemic condition, which later became obvious, was not recognized by her family, and especially by her husband. The husband held a great deal of faith in Gopal Daktar (the local healer). GD was called at the onset of labor and gave two tablets to increase labor contractions. After the birth, he again gave medicine to reduce the pain. All of these tablets were just aspirin, which GD admitted when later interviewed. In the delivery hut, Safar’s mother was present with the dai (traditional birth attendant). The birth was difficult because Safar was so weak. After the birth, she was unable to get up for ten hours. The dai and her mother knew that something was seriously wrong. The husband did not realize that his wife’s condition had deteriorated. He became alarmed only on the fifth day, when Safar’s entire body became swollen. The women in her village explained Safar’s headaches by the blood that had risen from her womb to her head. They see this blood as polluted and so as extremely harmful. Also, blood that circulates in the lower limbs may kill if it goes to the head. It seems that Safar lost a considerable amount of blood after giving birth. This did not cause as much concern because she was considered not to have bled long enough. Thus, she did not completely eliminate the polluted and harmful blood that was believed to be the cause of her swelling. On the fifth day, Safar had a sensation of burning in her limbs and asked for water to be poured over her head for the entire day. She was sweating profusely, however she registered no fever. Two days before she died, a midwife from the MCH clinic was called. She recommended that Safar be transferred immediately to the district hospital. She diagnosed a case of extreme anemia and thought that a blood transfusion was necessary and urgent. The husband did not listen to the midwife. He had more confidence in Gopal Daktar, who tried various medications and injections but to no avail. GD later claimed that he gave no “good” (meaning expensive) medicines because the family was too poor to pay. GD was annoyed with them for wasting his time On the seventh day, Safar Banu became unconscious. Her mother had her carried to the MCH clinic to get treatment from the midwife. Safar’s condition had deteriorated considerably, and it was feared that she would not survive the night. Her pulse was extremely low and she had difficulty breathing. The clinic offered to pay for medicines, but transport to hospital was to be the family’s responsibility according to the official policy. At this point, the elder son and a cousin took charge of the affair. They organized and paid for the transport to the district hospital. Safar’s mother felt that it was probably too late and of little use. She attempted to discourage her grandson. Half a “kani” of land had to be sold to pay for these costs, and the husband is still bitter with the clinic for not having provided any financial help. The son gave his own blood to save his mother but it was of no avail. The husband, a sick man himself, never went to the hospital. Safar Banu died the following day. Safar Banu’s mother confirmed how late the husband became aware of his wife’s critical state. Mention was also made of how hard Safar worked and how little she ate after her husband and sons had been fed. She drank water when there was no rice. When she was ill in the past, she had returned to her mother, a poor woman herself, to get help and treatment. The husband only thought of his own illness and did not see his wife’s problems. Safar Banu knew how to bear her sorrows in silence. Her husband praised her because she was uncomplaining. This story is based on interviews with the persons mentioned above, except Safar Banu. 23 Gender relationships played a key role in that the traditional birth attendant and Safar’s mother knew that something was seriously wrong but would not go against the husband’s preference to rely on the local quack. They delayed consulting a midwife until it was too late, and even then the husband discounted the midwife’s advice. The case highlights the importance of community factors (the gender system, misinformation, lack of community support) and the potential of community mobilization to contribute to the reduction of maternal and neonatal mortality. A number of community mobilization initiatives are already proving themselves to be effective, including more involvement of community health workers to create awareness about complications of delivery and demand for effective management of emergencies (discussed in more detail in the section on the health workforce), community support for transport (see the transport section), and support for mothers during delivery. An example of the latter is the promotion of home-based life-saving skill training. This approach involves both families and their communities to support birth preparedness and involvement of key decision makers to take action when it is needed and reduce delays in reaching referral centers (Silbey et al, 2001). Community-level safe motherhood committees and local health volunteers can provide effective support for such initiatives, particularly when they are linked effectively to the health system. Community groups were mobilized to conduct maternal death audits in Malaysia, enabling them to identify and address the conditions that contributed to the death of a mother in their community (Koblinsky et al, 1999). A frequently cited strategy for reducing distance-related delays for women who live in remote areas is to bring all of them to delivery centers or maternity waiting homes prior to delivery. In her review of experience with this strategy, Figa-Talamanca (1996) cites the experience of Cuba, which reduced its maternal mortality rate from 118 to 29 per 100,000 between 1962 and 1989. To facilitate accessibility to facilities with capacity to manage obstetric emergences, Cuba located waiting homes near these hospitals for women who lived in remote areas. Community organizations were mobilized both to build and run the waiting homes and to encourage their utilization, for example by providing childcare for pregnant mothers during the time of delivery. Waiting homes were also a key factor in Honduras, where the MMR dropped 40 percent in seven years (from 182 to 108) after the introduction of a multi-pronged strategy that included upgrading of facilities and staff capacity as well as community organization and infrastructure development (Danel, 2003). Figa-Talamanca's review also identified a number of factors that need to be addressed in introducing waiting homes, including the acceptability of the practice in societies where home delivery is the norm, the question of selecting women at greater risk of complications (since any delivery has the potential for complications), and the range of services that such centers provide and their costs to families. Broader community efforts such as micro-enterprise and credit programs targeted at poor women can reduce the gender disparity by ensuring that women have control over the money they earn and ensuring that information and education networks reach beyond the traditional boundaries and restrictions faced by poor women. In Africa, social action programs targeted to poor households have simultaneously provided funding for family planning and reproductive health services and created paying jobs for women. An evaluation of one such program in Malawi found that it had directly improved women’s reproductive health outcomes and had indirectly improved their status in the family, through its woman-focused educational, credit and employment initiatives (Marc et al, 1995). In Bangladesh, women’s participation in rural credit programs impacted positively on their demand for health care (Nanda, 1999). Women’s 24 empowerment, including higher control over resources, was addressed in the design of these programs. Health System Failures It is widely recognized that improved maternal and neonatal health outcomes require a continuum of care, from the household and community through the referral process to an effectively functioning health system. Poor health system performance is one of the reasons why poor women do not get life-saving interventions when they experience an obstetric complication. In a cross-national review of health system failures that contribute to high maternal mortality, Sundari (1992) identified several critical problems: shortage of trained personnel, lack of equipment and facilities (including consumables such as blood products and antibiotics), and poor patient management. These problems are also pinpointed in the World Bank assessment of obstacles to the achievement of health-related MDGS. In addition to the cost issue mentioned above, the report also mentions the quality of care as reflected in health workforce performance, availability of medicines, as well as inadequate and ineffective public spending. On the last point, a review of the benefit-incidence of public spending on health care in Africa by CastroLeal and colleagues found that subsidies are poorly targeted on the poor and typically favor the better off, a phenomenon that is not limited to Africa. Costs to consumers include payments for care and transport as well as opportunity cost, for example lost wages or time that would have otherwise been spent in household production. Even when publicly provided care is nominally free, under-the-table or side payments may be required to obtain services or medicines. Evidence suggests that the poor already pay a lot out of pocket, particularly for medicines, and could get better care for their money if health system performance were improved (Nahar and Costello, 1998). Health reformers have argued that cost recovery could improve the sustainability, quality and equity of health services by bringing payments into the open, rationalizing the use of services (for example, through incentives to use the level of care appropriate for the treatment required), and by giving providers control over resources and the incentive to use resources to improve quality. If combined with effective exemption schemes for the poor, cost recovery could also redirect public subsidies that typically benefit the rich more than the poor. Evaluating the impact of cost recovery schemes on MNH outcomes for the poor is not an easy task because of the many contextual and institutional influences that shape their implementation. Gilson’s (1997) review of experiences with user fees in Africa, where many countries introduced them during the 1980s, reports that: By themselves, fees tend to dissuade the poor more than the rich from using services; Fees, especially for community managed schemes like the Bamako Initiative that focus on medicines, may be associated with quality improvements that offset some of that negative impact on utilization; The equity impact depends a lot on the nature of the payment mechanism—direct payments have a more negative effect; Fees did not appear to generate sufficient revenue to enable the hoped-for reallocation of public subsidies to the poor; Exemption schemes did not really protect the poor, and often helped other groups (e.g. public sector employees) more than the poor; 25 Differential geographic implementation of fee schedules may only exacerbate geographic inequalities in access to care; and There is very limited evidence on the impact of fees on the budgets of poor households and their demand for health care. Available research on the response of poor households to fees shows that there is a substantial drop in utilization immediately after their introduction, followed by a partial return to pre-fee levels, and that poor households are somewhat more sensitive to price changes. Kutzin (1995) reports on research findings from Zimbabwe showing that intensified enforcement of user charges contributed to a 30 percent decrease in maternal health services compared to the year before enforcement, and that the numbers of babies born before reaching hospital increased by 4 percent as a possible result of mothers seeking to avoid per diem hospital charges. Mwabu and colleagues (1995) found that attendance at public clinics in Kenya dropped by 50 percent during the period when cost recovery was enforced (which lead to a suspension of fees), while Newbrander and colleagues (2000) found that poor consumers delayed seeking care more than rich ones in order to avoid costs. This response is particularly troubling in the case of maternal and neonatal care since such delays contribute to higher mortality. That review also noted that poor consumers tended to be unaware of exemption schemes or about how to take advantage of them even when such schemes existed. Nanda (2002) reports that exemption schemes do not include all reproductive health services and that their implementation is vulnerable to subjectivity and distortion by providers. Removal of financial obstacles to care has been a key policy change in countries that have successfully reduced MMRs. Both Malaysia and Sri Lanka provided maternity care free to clients who could not pay for services (Pathmanathan et al, 2003). Care was provided in public facilities, whose quality was improved in terms of accessibility, health worker performance, and availability of medicines. Countries that still have higher MMRs are attempting to reduce financial barriers using alternative financing options, though their impact on maternal mortality has yet to be measured. Bolivia's National Maternal and Child Health Program has increased coverage of maternal and child health care, though in its initial phase the poorest quintile appeared not to benefit because location and social exclusion proved to be as serious an obstacle as cost, so that special outreach to them was added in a later phase (Seoane et al, 2003). A study of the comparative impact of user fees versus community-based financing on utilization of services in Niger found that the community schemes had a more positive effect (Diop et al, 2000), though attention to the coverage of maternity care in such schemes needs to be watched. In Rwanda, the evaluation of an experimental community insurance program found that women who are members of a prepayment scheme were three times more likely to deliver with professional assistance than nonmember women, who were more likely to delivery at home and alone (Schneider et al, 2001). Mexico's PROGRESA program targets cash payments to poor households for education, nutrition and preventive health care and has had a positive impact on the nutrition of pregnant women and reduced low birth weight in newborns (Gertler, 2000). PROGRESA is also reported to have given poor women more say in household decision making and control over household resources, as well as increased schooling for poor children (Skoufias and McClaferty, 2001). Poor health workforce performance is another critical obstacle to poor women’s access to lifesaving interventions, particularly in view of the key role that skilled attendance at delivery is 26 known to play in the reduction of maternal and neonatal mortality. The large rich-poor differentials in skilled attendance documented in Table 3 suggest that even when countries have skilled attendants in their health workforce, these attendants are not serving the poor. Sundari’s (1992) review noted both the scarcity of such workers, particularly in rural areas, as well as lack of training and incentives to motivate workers. Health workforce problems are further exacerbated by losses of staff who die from AIDS or emigrate. An effort to upgrade delivery care in rural areas of Bangladesh during the 1990s was hindered by the fact that attendants were not available in facilities even when they were posted to them. Professional care was provided in the case of scheduled normal deliveries, but not available for emergencies that could occur at any time. In their study of contextual determinants on maternal mortality, Midhet and colleagues (1998) found that lack of trained staff at peripheral health facilities and access to those facilities accounted for most of the variation in maternal mortality in sixteen rural districts of rural Pakistan. Kwast (1996) reviewed performance issues in several countries (Bolivia, Guatemala, Indonesia and Nigeria), and also found that appropriate training of front-line staff combined community outreach and empowerment of women to recognize the importance of their own reproductive, maternal and neonatal health problems was critical to the reduction of physical and financial obstacles to care. In its discussion of links between health systems problems and efforts to improve maternal and neonatal health outcomes, the interim report of the Millennium Project Task Force on Maternal and Child Health reports that deficiencies in health workforce capacity are a major bottleneck. It calls for development of health workforce strategies that expand the supply of critical skills, including skilled birth attendants (Freedman et al, 2004). The recommended approach includes more effective involvement of traditional healthcare workers (including traditional birth attendants—TBAs), on whom many poor women still rely for reasons of cost, convenience, services offered and trust. Up to now, TBA-based maternal care programs alone have failed to reduce MNM, in large part because TBAs were not linked to a functioning health system. Current thinking about building health workforce capacity calls for more effective involvement of TBAs in skill-attendant strategies, particularly strengthening their role as advocates for skilled care and linking them more effectively to a functioning referral system (WHO, 2004). Experience in Malaysia and Brazil has demonstrated that effective involvement of TBAs in community mobilization, awareness and demand creation, and referral of emergencies can be effective, particularly as countries move from situations in which delivery by a skilled attendant is rare toward fully functioning systems with deliveries by professional attendants in comprehensive obstetric care facilities (Koblinsky et al, 1999). Decentralization of health system management is another tool that health reformers have employed in an effort to improve quality and accountability of front-line services. The rationale for such reforms is that if local authorities, and the communities that they serve, have greater control over human and financial resources, the system should be more responsive to local needs. Evaluation of experience of the impact of decentralization on poor women’s access to maternal health care is not easy because many forces are at work. In many cases, local managers are responsible for managing care but do not have real control of people and money. Resource allocation algorithms typically rely on formulas based on such measures as the number of hospital beds in an area rather than health needs, and control over personnel decisions remains centralized, so that local managers end up with the worst of both worlds. Further, decentralization often weakens specialized technical units (in this case, maternal health units that 27 might have been providing critical technical leadership prior to decentralization) at the central ministry, and there is not enough expertise at the local level to pick up the slack. On the positive side, targeted strategies such as the Marginal Budgeting for Bottlenecks described earlier have focused on training and incentives to improve workforce performance. A few African countries have experimented with the use of funding freed up through debt relief to create special incentive funds to support the redeployment of health workers to where they are needed. For example, in Mauritania a MBB bottleneck-identification exercise found that a lack of nurses and midwives in rural areas was a key obstacles to achievement of better maternal and child health outcomes. In response funds that were freed up through debt relief were used to the create incentive mechanisms to get staff to work in rural areas (Soucat et al, 2002). A similar effort in Mali focused on geographic availability of care as well as staffing. Safe motherhood strategies in a number of countries are focusing resources on the training and deployment of skilled attendants in facilities that serve poor women. The lack of consumables and equipment in facilities is another bottleneck. Even when an emergency is recognized and the woman suffering it has been referred to a treatment facility, she may still die if, in the case of a hemorrhage, blood products are not available, or antibiotics in the case of infection. Facilities where poor women might go are chronically short of consumables in many countries, though in some cases targeted cost sharing arrangements such as the Bamako Initiative have been able to overcome this obstacle (Gilson, 1997). That model relies on community management to ensure that revenues are used to address quality constraints and ensure local accountability. Performance problems seldom occur in isolation from each other. McPake and colleagues (1999) have documented the behavioral responses of public health workers in Uganda to poor incentives, scarcity of drugs and lack of management capacity. The situation encouraged drug leakage, side payments to obtain drugs, and understaffing of public health centers. Quality of service might have improved for consumers who could afford to pay, but probably at the expense of poorer ones who had to rely on “free” publicly provided treatment. A summary of findings on financial barriers, costs and cost recovery is presented in Table 13. Table 13: Selected Findings on Health System Issues Country, location Global Type of study Review Citation Africa Review Newbrander et al (2000) Africa Review Gilson (1997) Zimbabwe Impact Assessment Reported in Kutzin (1995) Kutzin (1995) Finding Studies in many countries have shown that poor people are more likely to be put off by price increases; travel costs have a similar deterrent effect. There were significant inequalities in access to health care under the user fee systems studied. The poor delay and wait longer for care, and often pay the same fees as the nonpoor. Poor people reduce utilization more than the rich when fees introduced, but quality improvements can improve utilization; administrative costs often high relative to fees, and exemptions schemes are hard to manage. User charges brought 30 percent reduction in use of maternal health services and increased 28 Malaysia, Sri Lanka Case studies Pathmanathan et al (2003) Global Review Global Review Global Reviews Ensor and Witter (2000) Freedman et al (2004) Koblinsky et al (1999); WHO (2004) Africa Case study Soucat et al (2002) births outside of hospitals by 4 percent. Removal of financial barriers a key policy change in countries that have reduced maternal mortality Unofficial, under-the-table fees are charged even when services are nominally free Health workforce limitations are a critical bottleneck in efforts to improve MNH. TBAs can be effectively involved in skilledattendant strategies for community mobilization, demand creation, and as referral agents. MBB is an effective mechanism for targeting debt-relief funds to overcome health system obstacles. Other Sectors Transportation: Delays in reaching a treatment facility pose key life-threatening obstacles for women who experience an obstetric emergency. Such delays can be the result of physical accessibility factors such as distance to a facility, the availability and cost of transport, and the condition of roads, all of which affect the time required to get a mother to a facility once the decision to seek care has been made (Thaddeus and Maine, 1994). A number of countries with high MMRs (Afghanistan, Pakistan, Nepal) also have large segments of their population living in remote areas that have poor road links to facilities that can provide life-saving interventions. In Zimbabwe, unavailability of transport is reported to have been a factor in 28 percent of deaths in a rural area that was studied (Fawcus et al, 1996). In the case of hemorrhage, 50 percent of deaths were attributable to transport-related delays. Measurement of road networks is complicated by differences in geographic settings and population distribution. The index of road quality in Table 8 above and used in the World Bank's analytical work on attainment of MDGs standardizes the proportion of the country's roads that are paved by dividing that proportion by the area of the country. While the index provides an approximation of variability in road access across countries, caution is needed in interpreting it for countries with a large land area and whose populations (and roads) are concentrated along coasts or in a smaller segment of the total land area (China, India, Brazil, and Nigeria, for example). Though there are few studies that focus specifically on these factors, and hardly any that link poverty to adverse MNH outcomes for poor women, the available evidence suggests that transport is a factor in the delays that threaten the lives of poor women. In their review of healthseeking behavioral responses to cost recovery, Newbrander and colleagues (2000) found that poor people in Tanzania traveled an average of over 60 kilometers for care, whereas the nonpoor traveled only 15 kilometers. There were similar findings in Kenya. The authors mention several possible reasons, including the likelihood that the non-poor have their own transport and that the poor travel farther in order to attend a facility where fees would be waived. In their review of obstacles to health care, Ensor and Cooper (2004) found studies that reported transport accounting for 28 percent of all total patient costs in Burkina Faso, 25 percent in northeast Brazil, and 27 percent in the United Kingdom. In Bangladesh, transport was reported to be the second most expensive item for patients after medicines. To quote from one of the focus groups in that study: “The hospital is far away and it costs a lot to travel there. We can easily buy 29 medicines from the village doctors with this money. We spend money to go to the hospital but we don't even get medicines there, so why should we go to the hospital?” (CIET-Canada, 2001, p. 38). Country-level poverty analyses conducted by the World Bank have shown that the quality rural road networks is a factor in the social and economic isolation of the rural poor. Research on the impact of improved rural road networks has focused mainly on travel time. For example, a poverty assessment for Guatemala found that road closures were a major constraint on access to schools, work and markets, and that households in the poorest income quintiles were much more affected (45 vs. 12 percent) than the richest (World Bank, 2003). Villagers identified “giving birth” as a risk because mothers could not reach health centers due to inadequate road access, particularly during the rainy season. Improved roads cut farm-to-market travel time from more than 10 hours to 1-2 hours. While the impact on access to emergency obstetric care was not assessed in the research, these reductions in travel time have clear implications for reducing distance related obstacles to timely management of emergencies. An earlier study of the impact of roads on access to services in Morocco found similar patterns. The road project contributed to clear gains in women’s utilization of health services (World Bank, 1996). Similar results were shown for girls’ school attendance, which increased much more (40 % vs. 10%) than for boys, for whom lack of roads posed a lesser obstacle than for girls. The quality and availability of roads is only one facet of the transport obstacles. The availability, type and cost of transport is clearly another. Research conducted by African partners in the Prevention of Maternal Mortality Network also found that poor roads, lack of vehicles and high transport costs were major causes of delay in deciding to seek and in reaching emergency obstetric care (Samai and Sengeh, 1997). That study reports the positive impact of efforts to improve transport and communication, along with community support and education activities, on the numbers of women getting treatment for obstetric emergencies, with consequent reductions in maternal deaths in the project area. Similar results have been reported for Nigeria (Essien et al, 1997), Uganda (Lalonde et al, 2003), and northwestern Tanzania (Ahluwalia et al, 2003). These studies emphasize the role of community organization in planning for emergencies when they occur, including preparation of delivery plans, mobilizing resources through community funds, reducing transport costs, and strengthening the referral chain. Mention of the referral chain reminds us that improved roads and transport may in some cases be necessary to reduce delays in management of obstetric emergencies but their overall impact on outcomes depends on many other factors. This is illustrated by research in India over a ten-year period when improved roads and transport led to increases in the number of women reaching hospital but little reduction in case mortality rates: the improved roads made it possible for women living farther away to get to the hospital but they were already in a moribund condition. Poverty, social inequality and gender conditions (including very early marriage) in their villages eroded the positive impact of improvements in infrastructure and treatment facilities (Pendse, 1999). A summary of findings on obstacles relating to distance and transportation is presented in Table 14. 30 Table 14: Selected Findings on Transport Interventions Country, Location Global Type of study Review Citation Global Review Ensor and Cooper, 2004 Rural Guatemala Poverty study World Bank, 2003 Rural Morocco Road impact study World Bank 1998 Thaddeus and Maine, 1994 Finding Distance and road conditions an obstacle to emergency care; better roads can help, but financial obstacles also need to be addressed Community health insurance schemes that include transport costs in benefit package have contributed to better access to care Long travel time to health facilities when roads poor, contributing factor to why “giving birth” considered a health risk Upgraded road network contributed to increased use of health services by rural women Education: Education of women influences reproductive health through a variety of channels, including childbearing attitudes, health-seeking behaviors, and earning opportunities. Early gains in female literacy played an important role in MMR declines in Malaysia and Sri Lanka (Pathmanathan, 2003). In her review of linkages between women’s education, autonomy and reproductive behavior, Jejeebhoy (1995) notes that education enhances women’s knowledge about the outside world and makes them more aware than uneducated women of the importance of family health and hygiene as well as the treatment and prevention of illness. Another consequence that she notes is greater decision-making autonomy within the home. At the same time, she cautions that contextual factors influence the impact of education on women’s participation in household decision making, so that this participation is likely to be weaker in a society characterized by a high degree of gender stratification. Focusing specifically on maternal mortality, McCarthy (1997) has noted several possible channels though which women's education might impact maternal mortality: By reducing the number of pregnancies (and lifetime risk of complications) through later marriage and increased use of contraceptives; By enabling women to be better informed about symptoms of complications and more likely to make more timely decisions to seek treatment; By being healthier and less likely to suffer a complication; By having better physical access to treatment facilities (for example, because a higher proportion of educated women live in urban centers); and By being better off and more able to pay for care, or be well treated by care providers because of their status. None of these potential linkages guarantees that education will have the hypothesized impacts. As both McCarthy (1997) and Thaddeus and Maine (1994) note, the empirical evidence on linkages between maternal education and utilization of health services is not at all clear-cut. We are reminded that educated women are more likely to rely on self-care and self-medication and to postpone visits to a facility until after such methods fail. They also note that if education is associated with desire for fewer births and later marriage, there may be more unintended pregnancies and higher abortion rates, which would pose greater risk when access to safe abortion is limited. 31 Education is closely linked to gender status and the ways in which gender stratification affects access to household resources and utilization of health care services (Kunst and Houweling, 2001). In their work on intra-household bargaining power in Indonesia, Beegle and colleagues (2001) found that women who were more educated than their husbands were more likely to obtain prenatal care and, generally, that education enables a woman to make decisions regarding her reproductive health care. Education is also linked to several of the other factors that may enhance or limit access to life-saving interventions. Research on the impact of cost recovery on utilization of services has shown that educated women are more likely to understand and use exemption schemes (Newbrander et al, 2000), and the transport literature also highlights the links between education and access to and utilization of transport to get to health facilities. Water and sanitation: Provision of safe water has been cited has a factor in the declines of mortality in developed countries (Van Poppel and Van der Heijden, 1997), and lack of sanitation and safe water, along with poor personal hygiene, are known to be major factors in the wide prevalence of parasitic diseases in poor countries. Studies of the impact of safe water on infant and childhood mortality typically do not focus separately on neonatal mortality, but recognize that waterborne diseases can undermine the health of pregnant women because they cause anemia, a risk factor for mothers as well as their newborns (Santiso, 1997). Paul (1993) cites unsafe water supply as well as pollutants from fuels used in cooking as risk factors in the high MMRs of the African countries he studied. When comparing countries by the level of MMR, there is a sharp difference in the percent of households with safe water in the countries with MMRs under 30 (92 percent) compared to those with MMRs over 1000 (51 percent). The link between water supply and MMRs/NMRs involves both household and community factors. A household’s consumption of water may be constrained by prices, income and other household variables even if water is supplied at the community level. Jalan and Ravallion (2001) observed that health gains largely bypassed poor children when piped water was available in their community, particularly when the mother was poorly educated. Nutrition: Poor nutrition is another key co-factor in maternal and neonatal mortality. The section on birth spacing identified the close link between poor nutrition and closely spaced births and maternal and neonatal mortality. The discussion in the previous section on malaria during pregnancy also highlighted the role of anemia. Poor nutrition among pregnant women in a number of the very high MMR countries is a factor contributing to those high rates. In India, anemia is reported as an indirect factor in 64.4 percent of maternal deaths (Buckshee, 1997). As the Safar Banu case demonstrated, gender stratification and attitudes also contribute through household behaviors that deprive poor women of adequate nutrition, not only during pregnancy but also during their childhood and adolescence, which leads to small stature and higher risk of delivery complications. The DHS tabulations cited earlier also document major rich-poor differentials in maternal and child nutrition within countries, as shown in Tables 15 and 16. For the 36 countries that collected data on body mass for reproductive-age women, those in the poorest wealth quintile had an average of 14.5 percent of women with low body mass (LBM), compared to 7.7 percent in the highest wealth quintile. 32 Table 15: Low Body-Mass in Reproductive-Age Women by Wealth Quintile and Region Region East Asia Central Asia + Turkey L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average Source: Gwatkin et al, 2004 No. of countries 0 4 8 3 2 19 36 Regional average * 5.1 5.5 10.2 40.2 12.9 11.7 Poorest quintile * 6.9 7.3 16.0 45.1 15.8 14.5 Richest quintile * 4.1 3.5 5.1 27.0 8.5 7.7 Poor/rich difference * 2.8 3.8 10.9 18.1 7.3 6.8 *not all countries collected these data South Asia had both the highest overall average of LBM and the largest differential between rich and poor quintiles. Latin America and the Caribbean along with Turkey and the two CentralAsian countries had the lowest overall average and the lowest rich-poor differentials. SubSaharan Africa and the Middle East/North Africa fell in between. Table 16: Child Malnutrition by Wealth Quintile and Region Region East Asia Central Asia + Turkey L. America, Caribbean Middle East, N. Africa South Asia Sub-Saharan Africa All country average Source: Gwatkin et al, 2004 No. of countries 0 4 9 3 4 21 41 Regional average * 23.1 23.0 35.2 46.6 34.2 31.9 Poorest quintile * 35.1 36.0 45.1 56.6 40.7 41.0 Richest quintile * 13.1 6.5 21.1 29.8 22.6 18.7 Poor/rich difference * 22.0 29.5 24.0 26.8 18.1 22.7 *not all countries collected these data Somewhat different patterns are found in the data for childhood malnutrition. Overall, the poorest quintiles have more than twice the percentage of malnourished children than the richest quintile. South Asia has the highest overall average, but Latin America and the Caribbean have the largest rich-poor differential, echoing the high level of income inequality for that region (for example, in Table 5 Brazil’s Gini coefficient was .59). Public Policy and Governance: Earlier in the paper, the table with countries grouped by the level of MMR showed that those with lower MMRs had better governance than those with higher rates when they were compared using a “governance effectiveness” indicator. That indicator was one of six compiled by World Bank experts (Kaufmann et al, 2003) covering 199 countries using several hundred variables drown from 25 separate data sources. The six indicators include government effectiveness, voice and accountability, political stability, regulatory capacity, rule of law, and control of corruption. The indicators have a mean of zero and a standard deviation of one, so that virtually all scores fall between –2.5 and +2.5, with higher scores indicating better performance. In the countries in the MMR sample, few countries (Bahamas, Singapore) had scores greater than one, and most were below the mean of zero. In Table 17, tabulation of average scores by MMR group for each of the indicators in the table below shows consistent falloff in performance as MMRs rise, and that the group with MMRs greater than 1000 has an average score near or below one standard 33 deviation below the mean for all of the indicators. Political instability stands out as the indicator with the lowest average for this group, and the highest average for the countries with low MMRs. Table 17: Governance Indicators for Countries Grouped by MMR Level MMR Level 0-30 31-100 100-300 301-1000 Over 1000 Number of Effective countries governance 17 39 32 41 13 0.41 -0.07 -0.35 -0.37 -1.08 Voice & accountability Political stability Regulatory quality Rule of Law .29 -.24 -.23 -.35 -.86 .47 .04 -.20 -.37 -1.13 .51 -.07 -.27 -.34 -1.07 .35 -.12 -.36 -.38 -1.06 Control of corruption .41 -.16 -.40 -.36 -.94 Source: Kaufmann et al, 2003 Addressing Obstacles and Information Gaps Policy and Program Actions The strong negative correlation between MMRs and per-capita health expenditures suggests that more health spending is needed, but as the World Bank study on reaching the Millennium Development Goals in health reminds us, spending alone is not enough. The added health funding needs to be targeted on key obstacles that reduce poor women’s chances of accessing life-saving interventions when they are needed. It also has to be combined with improvements in government effectiveness and motivation of individuals and communities to make use of these interventions. Success stories like Sri Lanka and Malaysia demonstrate that sustained efforts to improve health system performance, increase women’s education, and improve infrastructure, along with targeted investments and policy change to establish a cadre of trained midwives to ensure safe delivery and effective management of emergencies do work (Pathmanathan et al, 2003). Other countries that have reduced maternal and neonatal mortality (Honduras, an example cited earlier, and the Indian state of Kerala8) have proved that a combination of targeted investments in life-saving interventions as well as social infrastructure can make a difference. The Marginal Budgeting for Bottlenecks approach described earlier suggests that increased public expenditures on health will have an even greater impact if they are targeted on key obstacles that prevent poor women from accessing life-saving interventions. The first step in the MBB approach is the identification of such obstacles. Using the Pathways framework outlined in the introduction, this paper has shown that obstacles are both inside and outside the health system, beginning with individuals, households and communities and including both health care and health financing as well as other sectors—education, transportation, water/sanitation, and nutrition. The relative importance of obstacles will vary by country and region, but a number of them appear to affect most of the countries that currently have high maternal and neonatal mortality. MBB also requires costing of interventions to address these obstacles and tracking of expenditures and performance of the interventions that are funded to ensure that the targeted spending is being used effectively and that the poor are benefiting. Kerala’s MMR of 87 is less than a sixth of India’s national average and less than eighth of the rate in Orissa in the country’s northern tier. 8 34 Table 18: Actions to Address Obstacles Obstacle/Pathways Level Other reproductive risks Unintended pregnancy & unsafe abortion Violence and refugee status Infectious diseases (TB, malaria, HIV/AIDS) Household level Poor hygiene Poor nutrition Women's lack of autonomy in decisions Community level Gender attitudes Community support Health system level Inadequate staffing; unsafe procedures, including unsafe abortion Lack of consumables and medicines Inadequate facilities Other sectors Education Transport Water & sanitation Nutrition Public policy Public health expenditures Good governance Action Indicator Increase access to FP and ensure abortion safety Improve RH services in refugee settings Link RH and infectious disease programs Unmet need for family planning Health education Micronutrients during pregnancy Ensure that credit schemes & social funds give decision power to poor women Hand washing Maternal anemia Leadership support of improved women's status Religious and community leaderships groups engaged in gender issues Community mobilization to ensure safe delivery and referral of emergencies Percent of communities that participate in life-saving skills training and implementation Targeted expenditures on training and deployment of midwives and key staff Percent of outreach or first referral points with trained midwives Involve TBAs and others in community in creating awareness and referrals Percent of TBAs who are engages as community agents Targeted expenditures to reduce gaps Targeted investments to upgrade facilities Percent of facilities with standard list available Percent of communities with delivery homes and access to referral facilities meeting service delivery norms Increase female enrollment Increase paved roads Improve access to safe water Nutrition supplementation Enrollment rates Percent of paved roads Percent of households with safe water Anemia rates Targeted increases in health spending Percent of public expenditures on health (identifying, if possible, those targeted on MMR and NNM) Implementation of effective budget tracking procedures Reforms in financial management and resource allocation MMRs in refugee camps HIV, TB and malaria treatment rates for pregnant women Women having control over money Table 18 summarizes obstacles described in the paper and identifies possible program and policy changes to address them. If the performance of targeted interventions is to going to be tracked effectively, then better information is needed on rich-poor differentials in mortality, and on the 35 morbidities that follow on poorly managed obstetric emergencies. Expenditure tracking also needs to be fine-tuned so that pro-poor expenditures on these investments can be monitored. Achievement of lower maternal and neonatal mortality for poor women is possible if the obstacles to their utilization of interventions that are known to be effective can be overcome. As noted above, the countries that have reduced mortality rates have done this through a combination of investments inside and outside the health system including improving the skills and deployment of midwives and other key staff, reducing financial obstacles to care, improving the quality of care and access to referral facilities, and mobilizing households and communities to ensure safe delivery and effective management of emergencies when they occur. Parallel investments in nutrition, malaria control, education, roads, and water/sanitation have also contributed in situations where low performance in those areas has undermined the reproductive health of poor women. Strengthening the Evidence Base While the tabulations of maternal and neonatal health-related indicators in Demographic and Health Surveys (DHS) for wealth quintiles have helped to advance our understanding of linkages between MNH and poverty, there are still significant gaps in the evidence base. Data on maternal and neonatal mortality and morbidities are generally scarce, and particularly so for studying rich-poor differences. Sample sizes in most DHS surveys are typically too small for calculating rich-poor differences in maternal mortality, though Graham and colleagues (2004) have developed methodology for calculating rich-poor differentials in maternal mortality from a subset of larger DHS surveys. Special DHS supplements like the recent Bangladesh Maternal Health Survey also offer an opportunity for gaining further insights into links between maternal mortality and poverty. If there are problems in addressing rich-poor differentials in maternal and neonatal mortality and their consequences, there is an even greater evidence gap concerning the life-long morbidities suffered by women who survive a poorly managed obstetric emergency. A comparison of estimates of the burden of disease for maternal conditions with BOD for TB, malaria and HIV/AIDS suggests that the impact of these morbidities is substantial. Table 19 shows estimates of years of life lost (YLL) and years lived with disability (YLD) for the population aged 15 and over for these four conditions for sub-Saharan Africa in 2002: Table 19: Estimates for Burden of Disease for sub-Saharan Africa, 2002 Condition TB Malaria HIV/AIDS Maternal conditions YLL (1000) 6,994 1,748 43,849 6,865 YLD (1000) 795 528 5,514 4,884 Ratio YLD/YLL .11 .30 .13 .71 Source: WHO, GBD Estimates, www3.WHO.int/whosis, accessed 12/04/04 While the number of years of life lost due to maternal causes is substantially lower than for HIV/AIDS (though about the same as for TB, a cause of death associated with HIV/AIDS, and larger than for malaria, where deaths are concentrated among children), the years lived with disability associated with maternal conditions is nearly as large as for HIV/AIDS. One of the 36 most poignant examples of this latter burden is that suffered by mostly young and poor African women who survive obstructed labor but live on with an obstetric fistula, which has terrible social and economic consequences. While fistulae and other obstetric morbidities can be treated, resources are often not allocated to them, and women who suffer them continue to endure their consequences as part of what may often be accepted as their normal lot. In an era in which allocation of health resources is increasingly being driven by such evidence-based algorithms as disability-adjusted life years, the combination of poorly measured and comparatively rare maternal mortality (compared to other causes, including major communicable diseases and noncommunicable diseases) plus poorly measured morbidities highlights the importance of improving the measurement of maternal morbidities, particularly for the poor in order to support the call for allocation of adequate resources to address these problems. Expenditure tracking is an important policy and advocacy tool in the health field and needs to be employed more effectively by the champions of maternal and neonatal health. Countries that are participating in debt-relief and/or poverty-reduction programs are required by the IMF and World Bank to prepare Poverty Reduction Strategies. These strategies include analyses of the causes and consequences of poverty as well as expenditure plans to address specific poverty issues. The Medium Term Expenditure Framework (MTEF) is both a prospective mechanism for allocating funding across key sectors that affect poverty and a retrospective tracking mechanism to ensure that planned allocations are actually made. While the level of detail in the typical MTEF is typically limited to the broad sectoral level (education, health, water and sanitation, etc), expenditure tracking through the MTEF process offers an important opportunity for champions of MNH to track key expenditures required to improve MNH (training and deployment of trained birth attendants, sustained funding of facilities and referral networks for the management of obstetric emergencies, etc.; see Reinikka and Svensson, 2002). A stronger evidence base is also needed on linkages between poverty and MNH outcomes and on the effectiveness of interventions inside and outside the health sector to address them. When research funding is scarce, one way to achieve this is to add special inquiries of maternal and neonatal health outcomes to on-going survey programs, particularly longitudinal surveys that track groups of respondents over time. These permit analyses that show both the consequences of poor MNH outcomes on the well-being, consumption and economic productivity of households and different income/wealth levels and the impact of interventions inside (e.g., increase in skilled attendance) and outside (credit programs, community mobilization) the health system on those outcomes. Survey initiatives in several countries (Indonesia, Kenya, Malawi, Mexico, and the Philippines; see Table 20) might be engaged in this task. 37 Table 20: Longitudinal Survey Programs Country Data set Population Type of Survey Mexico PROGRESA panel data www.ifpri.org PROGRESA program focuses on population in extreme poverty in rural areas. Program addresses poverty through monetary and in-kind benefits, and encouraging investments in education, health and nutrition. Longitudinal Philippines Cebu Longitudinal Health and Nutrition Survey www.cpc.unc.edu/pr ojects/cebu/ Longitudinal Indonesia Indonesian Family Life Survey www.rand.org/FLS/IF LS The Cebu Longitudinal Health and Nutrition Survey is part of an ongoing study of a cohort of Filipino women who gave birth between May 1, 1983 and April 30, 1984. The cohort of children born during that period, their mothers, other caretakers, and selected siblings have been followed through subsequent surveys conducted in 1991-2, 1994, and 1999. The Indonesian Family Life Survey (IFLS) is an ongoing longitudinal survey in Indonesia. The first wave of the IFLS (IFLS1) was conducted in 1993/94. IFLS2 and IFLS2+ were conducted in 1997 and 1998, respectively. IFLS2+ covered a 25% sub-sample of the IFLS households. IFLS3 was conducted in 2000 and covered the full sample. Kenya www.ssc.upenn.edu/ Social_Networks/Lev el%203/Kenya/level3 _kenya_data.htm The first survey of the Kenya Diffusion and Ideational Change Project (KDICP-1) was carried out in 1994-5, and interviewed 925 ever-married women of childbearing age and 859 men (of which 672 were husbands of the currently married women ). In 1996-7 and in 2000, respectively, the second and third round of the survey (KDICP-2 and KDICP-3) followed-up the same respondents (if eligible), and also interviewed any new spouse. All rounds of the KDICP were carried out in four sites in Nyanza Province, in south-west Kenya. Within each village, currently married women and their husbands were eligible respondents Cross-sectional, individual-level data The MDICP is a sister project of the Kenya project above also focuses on the role of social networks in changing attitudes and behavior regarding family size, family planning, and HIV/AIDS in Malawi. Cross-sectional, individual-level data for men and women; Malawi http://www.ssc.upen n.edu/Social_Networ ks/Level%203/Malaw i/level3_malawi_data .htm Longitudinal Longitudinal, individual-level data 38 Conclusion This paper has reviewed the evidence base on obstacles that poor women and newborns face when they suffer life-threatening obstetric complications. It has drawn on available crossnational comparisons and analyses of data, broken down where possible to show rich-poor differences in MNH outcomes, as well as on the extensive literature on factors within and beyond the healthcare system that affect MNH outcomes. The Pathways framework was used to organize the review of evidence. While it is not the only conceptual framework available, it has the advantage of being the one recommended for the planning of health expenditures at countrylevel in Poverty Reduction Strategies currently being implemented in poor countries where maternal and neonatal mortality rates are the highest. The evidence suggests that these obstacles can seriously undermine poor women’s chances of getting life-saving care when they need it, but that a combination of multi-sector efforts can overcome such obstacles. It has also shown that there are important knowledge gaps to be addressed by building a stronger evidence base on maternal and neonatal mortality and morbidities experienced by poor women, how well expenditure is targeted to address obstacles, and the effectiveness of interventions. 39 Annex 1: Maternal Mortality in India Of the estimated 529,000 maternal deaths estimated by WHO to have occurred globally during the year 2000, 136,000 were estimated to have occurred in India. This reflects both the high MMR for India (the MMR for year 2000 is estimated to have been 540) and India’s large population (over 1 billion). Only China has a larger population, though with its MMR of 56 it had fewer than one-tenth the number of maternal deaths (11,000 deaths). Data on MMR differences within India are limited. In its National Human Development Report 2001, India’s Planning Commission (2002) published MMRs for 15 large states for 1997-1998 based on the Sample Registration System (SRS). Bhat (2001) has applied indirect estimation techniques to those data to produce adjusted estimates. Bhat’s indirect method produced a national level MMR estimate of 479 for the period 1987-1996, compared to a figure of 407 from the SRS. Both estimates are lower than the WHO estimate for 2000, though Bhat’s figure is very close to the 1995 estimate of 470 produced by WHO/UNICEF/UNFPA. Both direct and indirect SRS estimates suggest substantial variation by state within India. The SRS data vary widely, and give rates that are implausibly low for Gujarat and Tamil Nadu and high for Kerala, suggesting that it would be better to use Bhat’s adjusted estimates. These are produced in column 2 of the table on the next page, along with other indicators from the Planning Commission that relate to the Pathways framework. In the table, states are ranked from the highest to lowest MMRs, with estimates ranging from over 700 in Assam, Uttar Pradesh and Madhya Pradesh to under 200 in Punjab, Tamil Nadu and Kerala. SRS estimates are used for Punjab and Kerala because Bhat reported that the rates in those two states were too low to estimate using indirect methods. Their SRS estimates may be high. The populations in many Indian states are larger than those of many countries for which WHO reports its MMR estimates. For example, Uttar Pradesh is as large as Brazil, the world’s fifth largest country. State-wise MMR differences are most closely correlated with the indicator for attended deliveries (r = .89), with a general pattern of low rates of attended delivery (20-30 percent) in the poorer northern tier states and higher rates (60-90 percent) in the more prosperous southern ones. The Planning Commission’s gender disparity index (female attainment relative to male in literacy, life expectancy and economic participation) ranges from 0.5 to 0.6 in the high MMR states to around 0.8 in the low MMR states. Data for other indicators used in cross-country comparisons (road density, public health expenditures) do not reveal clear relationships with MMR differentials. The high MMR states are generally the poorer ones, although Kerala has a much lower GDP per capita than Gujarat, but Gujarat’s MMR is three times that of Kerala. Prevalence of anemia is generally higher in the high MMR states than in the lower ones. The three low MMR states have the highest per capita public health expenditures, but Assam with the highest MMR spends nearly as much as most of the lower MMR states. The low level of attended deliveries in Assam reinforces the point that it is not just the amount of expenditure, but how it is spent. Clearly Assam, UP and other high MMR states are not spending enough to ensure that all deliveries have skilled attendants. 40 Annex Table 1: MMRs and Other Indicators for Indian States Assam Uttar Pradesh Madhya Pradesh Orissa Gujarat Rajasthan Bihar Karnataka Haryana West Bengal Maharashtra Andra Pradesh Punjab Tamil Nadu Kerala INDIA MMR Population (Mil) Att. Del. (%) Gender Index 984 737 26.6 174.5 21.5 23.0 .58 .52 Road Density (Km/ 100KM2) 87.2 86.8 Female Anemia (%) 700 597 596 580 513 480 472 458 380 81.1 36.7 50.6 56.5 109.8 52.7 21.1 80.2 96.8 30.1 33.7 53.5 36.2 23.5 59.2 42.0 44.5 59.7 .66 .64 .71 .69 .47 .75 .71 .63 .79 45.1 168.7 46.7 37.9 50.8 75.1 63.7 85.0 117.6 54.3 63.0 46.3 48.5 63.4 42.4 47.0 62.7 48.5 2.0 2.3 3.0 3.1 1.7 3.0 2.8 2.7 3.0 1922 1666 3918 2226 1126 2866 4025 2977 5032 283 199* 195 195* 75.7 24.3 62.1 31.8 65.1 62.7 84.1 94.1 .80 .71 .81 .83 64.7 127.7 158.6 374.9 49.8 41.4 56.5 22.7 2.5 3.7 3.6 4.0 2550 4389 3141 2490 479 1027.2 42.3 .68 74.9 51.8 2.3 2840 69.7 48.7 Publ. Health Exp/P in $ 3.1 2.2 Net State or National Prod/P 1675 1725 Sources: Bhat (2001) and GOI Planning Commission (2002); MMRs for Kerala and Punjab from SRS. Public health expenditures per capita and net state domestic product per capita in constant 1980-81 rupees. Health expenditure data from Peters et al. (2002). 41 Annex 2: Country-Level Data Table Country MMR Deaths/ 100,000 births (2000) UNDP status of women index Govern -ance index Combined female enrollment data Gini Coefficient Health Expend. Per capita Safe Water Paved (% of pop. roads as % with of total road access) KM MMU <30 Slovak Republic 3 0.834 0.4 74 25.8 574 100 86.7 Kuwait Croatia 5 8 0.813 0.802 0.16 0.19 57 69 29 605 410 100 76 80.6 84.6 Czech Republic Yugoslavia, FR (Serbia/Montenegro) 9 0.857 0.7 77 25.4 640 92 100 11 -0.73 53 127 83 62.3 Lithuania Poland 13 13 0.823 0.839 0.61 0.61 88 91 36.3 31.6 273 392 75 90 91.3 68.3 Uzbekistan Hungary 15 16 0.727 0.834 -1.1 0.78 74 36 26.8 24.4 109 372 85 99 87.3 43.4 Slovenia Korea, Rep. Of 17 20 0.879 0.873 0.82 0.84 85 84 28.4 31.6 996 862 100 92 100 74.5 Macedonia, FYR Saudi Arabia 23 23 70 57 28.2 0.743 -0.39 -0.05 141 332 71 95 63.8 30.1 Mauritius Uruguay 24 27 0.77 0.83 0.53 0.51 68 89 44.8 288 849 100 98 97 90 Bahrain Singapore 28 30 0.829 0.88 0.78 2.26 84 75 42.5 539 750 100 100 76.9 100 72 93 52.3 19.4 MMR 31-100 Bosnia and Herzegovina Chile 31 31 -0.9 1.19 51 71 57.5 145 581 Turkmenistan Bulgaria 31 32 -1.47 -0.06 81 79 40.8 31.9 90 193 61 100 81.2 94 Georgia Cuba 32 33 -0.77 -0.26 70 77 38.9 94 109 79 91 93.5 49 Belarus Ukraine 35 35 0.803 0.761 -1.03 -0.74 87 79 30.4 29 253 128 100 98 89 96.7 Moldova Brunei 36 37 0.697 0.867 -0.63 0.96 63 84 36.2 133 857 92 87 34.7 Jordan Malaysia 41 41 0.729 0.784 0.36 0.92 78 74 36.4 49.2 178 202 96 88 100 75.8 Latvia Costa Rica 42 43 0.81 0.821 0.67 0.37 91 66 32.4 45.9 246 489 93 95 38.6 22 Thailand Cyprus 44 47 0.766 0.886 0.28 1 69 75 43.2 327 731 84 100 97.5 57.4 Romania United Arab Emirates 49 54 0.771 -0.33 0.83 70 74 30.3 136 816 58 97 49.5 100 Albania 55 0.732 -0.47 70 63 97 39 Armenia 55 0.727 -0.42 63 37.9 152 73 96.3 China 56 0.718 0.18 62 40.3 74 75 22.4 0.794 42 Country MMR Deaths/ 100,000 births (2000) UNDP status of women index Govern -ance index Combined female enrollment data Gini Coefficient Health Expend. Per capita Safe Water Paved (% of pop. roads as % with of total road access) KM Bahamas, The Estonia 60 63 0.811 0.831 1.4 0.78 77 93 37.6 1230 346 97 77 57.4 20.1 Dem Rep of Korea Russian Federation 67 67 0.774 -1.78 -0.4 82 45.6 39 251 100 99 6.4 67.4 Turkey Fiji 70 75 0.726 0.743 -0.2 0.06 54 75 40 46 231 214 82 47 34 49.2 Iran, Islamic Rep. Argentina 76 82 0.702 0.839 -0.46 -0.49 63 94 43 200 823 92 71 56.3 29.5 Mexico Egypt, Arab Rep. 83 84 0.79 0.634 0.15 -0.32 74 72 51.9 34.4 421 118 88 97 32.8 78.1 Jamaica Oman 87 87 0.75 0.736 -0.07 0.69 71 56 37.9 212 334 92 39 70.1 30 Sri Lanka Azerbaijan 92 94 0.726 0.03 -0.96 64 69 34.4 36.5 77 48 77 78 11.1 92.3 Barbados Venezuela, RB 95 96 0.885 0.767 1.36 -1.14 94 70 46 49.1 814 298 100 83 98.6 33.6 Libya Botswana 97 100 0.611 -0.87 0.87 91 81 63 221 219 72 95 57.2 55 Tajikistan 100 0.673 -1.23 65 34.7 94 60 71.5 Honduras 110 0.656 -0.73 61 59 156 88 20.4 Kyrgyz Republic Mongolia 110 110 0.659 -0.81 -0.18 80 69 29 44 66 69 77 60 91.1 3.5 Suriname Tunisia 110 120 0.727 -0.16 0.65 79 76 41.7 257 239 73 80 26 64.8 Colombia Ecuador 130 130 0.774 0.716 -0.39 -0.96 72 71 57.1 43.7 507 186 91 85 14.3 18.9 Vietnam Algeria 130 140 0.687 0.687 -0.27 -0.59 61 69 36.1 35.3 65 122 77 89 25.1 68.9 Belize Qatar 140 140 0.756 -0.06 0.69 68 85 212 1105 92 100 17 53.1 Cape Verde Dominican Republic 150 150 0.719 0.727 -0.2 -0.41 79 77 60 202 74 86 78 49.4 El Salvador Lebanon 150 150 0.707 0.737 -0.53 -0.41 63 77 50.8 228 563 77 100 19.8 84.9 Panama Syrian Arab Republic 160 160 0.781 0.668 -0.14 -0.57 78 61 48.5 449 109 90 80 34.6 23.1 Trinidad and Tobago Guyana 160 170 0.796 0.73 0.47 -0.32 68 84 40.3 44.6 325 130 90 94 51.1 7.4 Paraguay Philippines 170 200 0.739 0.748 -1.29 -0.06 64 81 57.7 46.1 246 100 78 86 9.5 21 Kazakhstan Morocco 210 220 0.763 0.590 -0.8 0.07 78 46 31.2 39.5 127 159 91 80 94.7 56.4 MMR 101-300 47.4 43 Country MMR Deaths/ 100,000 births (2000) UNDP status of women index Govern -ance index Combined female enrollment data Gini Coefficient Health Expend. Per capita Safe Water Paved (% of pop. roads as % with of total road access) KM Indonesia Nicaragua 230 230 0.677 0.636 -0.56 -0.87 63 66 30.3 60.3 56 150 78 77 46.3 11 South Africa Guatemala 230 240 0.678 0.638 0.52 -0.61 78 54 59.3 55.8 396 87 86 92 20.3 34.5 Iraq Brazil 250 260 0.77 -1.64 -0.22 40 97 60.7 110 428 85 87 84.3 5.5 Namibia Papua New Guinea 300 300 0.622 0.544 0.18 -0.78 75 39 70.7 50.9 312 77 77 42 13.6 3.5 Myanmar Swaziland 360 370 -1.29 -0.44 47 75 60.9 78 118 72 0.536 12.2 55 Bangladesh Peru 380 410 0.495 0.734 -0.53 -0.47 54 78 31.8 46.2 70 246 97 80 9.5 12.8 Bhutan Bolivia 420 420 0.663 0.93 -0.53 80 44.7 82 153 62 83 60.7 6.5 Gabon Cambodia 420 450 0.551 -0.45 -0.56 81 49 40.4 196 73 86 30 9.9 16.2 Comoros Pakistan 480 500 0.521 0.469 -0.84 -0.5 36 27 33 47 71 96 90 76.5 43 Congo, Rep. Gambia, The 510 540 0.496 0.457 -1.25 -0.81 53 43 47.8 101 52 51 62 9.7 35.4 Ghana India 540 540 0.564 0.574 0.01 -0.13 42 49 39.6 37.8 45 84 73 84 29.6 45.7 Lesotho Madagascar 550 550 0.497 0.467 -0.26 -0.38 65 43 56 46 100 18 78 47 18.3 11.6 Togo Yemen, Rep. 570 570 0.483 0.424 -1.17 -0.87 53 34 33.4 34 33 54 69 31.6 11.5 Sudan Eritrea 590 630 0.483 0.434 -1.11 -0.44 32 29 43 24 74 46 36.3 22.1 Lao PDR Haiti 650 680 0.518 0.462 -0.8 -1.56 51 51 37 53 55 37 46 5 24.3 Cote d'Ivoire Senegal 690 690 0.376 0.42 -0.18 31 34 36.7 41.3 57 71 81 78 9.7 29.3 Cameroon Djibouti 730 730 0.488 -0.62 -0.88 43 19 47.7 38.6 86 48 58 100 12.5 12.6 Guinea Nepal 740 740 -0.78 -0.51 26 57 40.3 36.7 52 41 48 88 16.5 30.8 Zambia Liberia 750 760 0.376 -0.93 -1.51 43 43 52.6 64 33 64 46 16 6.2 Nigeria Benin 800 850 0.45 0.395 -1.12 -0.62 41 38 50.6 35 39 62 63 30.9 20 Ethiopia Equatorial Guinea 850 880 0.347 -0.89 -1.37 27 49 48.6 20 89 24 44 12 21.8 MMR 301-1000 0.479 44 Country Uganda Dem Rep of Congo MMR Deaths/ 100,000 births (2000) UNDP status of women index Govern -ance index Combined female enrollment data Gini Coefficient Health Expend. Per capita Safe Water Paved (% of pop. roads as % with of total road access) KM 880 990 0.483 0.353 -0.41 -1.6 66 24 37.4 44 22 52 45 6.7 0.5 Burkina Faso Burundi 1000 1000 0.317 0.331 -0.69 -1.46 18 28 48.2 33.3 37 26 42 78 16 7.1 Kenya Mauritania 1000 1000 0.488 0.445 -0.85 -0.16 52 40 44.5 37.3 58 73 57 37 12.1 11.3 Mozambique 1000 0.341 -0.41 32 39.6 50 57 18.7 Central African Republic 1100 0.352 -1.43 20 61.3 34 70 2.7 Chad Guinea-Bissau 1100 1100 0.366 0.353 -0.75 -1.35 24 34 47 35 54 27 56 0.8 10.3 Somalia Zimbabwe 1100 1100 0.489 -1.97 -0.8 7 58 56.8 11 130 26 83 11.8 47.4 Mali Rwanda 1200 1400 0.327 0.416 -0.84 -0.82 26 51 50.5 28.9 34 35 65 41 12.1 8.3 Tanzania Niger 1500 1600 0.396 0.279 -0.51 -0.79 31 14 38.2 50.5 36 27 68 59 4.2 7.9 Angola Malawi 1700 1800 0.378 -1.16 -0.68 26 70 50.3 47 49 38 57 10.4 18.5 Afghanistan Sierra Leone 1900 2000 62.9 28 31 13 57 13.3 7.9 MMR>1000 -1.39 -1.54 44 Sources (cells are empty when no data were available): Maternal Mortality in 2000: Estimates Developed by WHO, UNICEF and UNFPA Status of women: Human Development Indicators, Human Development Report 2003 Indicators (http://www.undp.org/hdr2003/indicator/indic_197_1_1.html) Governance index (government effectiveness): Governance Indicators 1996-2002, World Bank, (http://info.worldbank.org/governance/kkz2002/tables.asp) Female Enrollment: World Bank, http://devdata.worldbank.org/genderstats/home.asp and UNDP, Human Development Report, 2003. Gini coefficients: World Bank, World Development Indicators and UNDP, Human Development Report, 2003 Female Enrollment: World Bank, http://devdata.worldbank.org/genderstats/home.asp and UNDP, Human Development Report, 2003. Health Expenditures per capita: Human Development Report 2003 Indicators (http://www.undp.org/hdr2003/indicator/indic_59_1_1.html) Safe Water: UNDP, Human Development Report, 2003 Roads: http://millenniumindicators.un.org/unsd/mi/mi_goals.asp and other sources 45 References AbouZahr, C. and E. Ahman (1998). Unsafe abortion and ectopic pregnancy. Health Dimensions of Sex and Reproduction: The Global burden of Sexually Transmitted Diseases, HIV, Maternal Condition, Perinatal Disorders, and Congenital Anomalies. C. J. L. Murray and A. D. Lopez. Geneva, World Health Organization: 267-296. AbouZahr, C. and T. Wardlaw (2004). Maternal Mortality in 2000: Estimates Developed by WHO, UNICEF and UNFPA. Geneva, World Health Organization. Ahluwalia, I. B., T. Schmidt, et al. (2003). "An evaluation of a community-based approach to safe motherhood in northwestern Tanzania." International Journal of Gynecology and Obstetrics 82: 231-240. Ahman, E., C. Dolea, et al. (2003). The global burden of unsafe abortions in the year 2000. Geneva, Department of Reproductive Health and Research, WHO, Geneva. Anandalakshmy, P., P. Talwar, et al. (1993). "Demographic, socio-economic and medical factors affecting maternal mortality--an Indian experience." Journal of Family Welfare 39: 1-4. Bartlett, L. A., D. J. Jamieson, et al. (2002). "Maternal mortality among Afghan refugees in Pakistan, 1999-2000." The Lancet 359: 643-649. Becker, C. M., D. I. Bibosuonova, et al. (1998). "Maternal care vs. economic wealth and the health of newborns: Bishkek, Kyrgyz Republic and Kansas City, USA." World Development 23(11): 2057-72. Beegle, K., E. Frankenburg, et al. (2001). "Bargaining power within couples and use of prenatal and delivery care in Indonesia." Studies in Family Planning 32(11): 130-146. Bennett, S. (2004). "The role of community-based health insurance within the health care financing system: a framework for analysis." Health Policy and Planning 19(3): 147-158. Berer, M. (2002). "Making abortions safe: a matter of good public health policy and practice." Reproductive Health Matters 10(9): 31-44. Bhat, P. N. M. (2001). Maternal Mortality in India: An Update. Delhi, Institute of Economic Growth. Bhat, P. N. M. (2004). "Commentary: On reappraisal of adult mortality." International Journal of Epidemiology 33: 717-718. Birdsall, N., A. J. Ibrahim, et al. (2004). Task Force 3 Interim Report on Gender Equality. New York, Millennium Project. Blanchet, T. (1991). Maternal Health in Rural Bangladesh. Dhaka, UNICEF Bangladesh Country Office. Buckshee, K. (1997). "Impact of roles of women on health in India." International Journal of Gynecology and Obstetrics 58: 35-42. Calvo, C. M. (1994). "Case study on the role of women in rural transport: access of women to domestic facilities." Case, A. and A. Deaton (2002). Consumption, health, gender and poverty. Princeton, NJ, Research Program in Development Studies, Princeton University. Castro-Leal, F., J. Dayton, et al. (1999). "Public social spending in Africa: do the poor benefit?" The World Bank Research Observer 14(1): 49-72. Child Health Research Project (1999). Reducing perinatal and neonatal mortality. Child Health Research Project Special Report. Baltimore, Johns Hopkins University. CIET-Canada (2001). Health and population sector programme, 1998-2003. Service Delivery Survey, Second Cycle. Dhaka, Ministry of Health and Family Welfare. Collymore, Y. (2004). Conflict chips away at living conditions in Sudan. Washington, DC, The Population Reference Bureau. 46 Conde-Agudelo, A. and J. M. Belizan (2000). "Maternal morbidity and mortality associated with interpregnancy interval: cross sectional study." British Medical Journal 321(1): 255-259. Danel, I. (2003). Honduras, 1990-1997. Reducing Maternal Mortality: Lessons from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe. M. A. Koblinsky. Washington, DC, Human Development Network, The world Bank: 51-62. De Brouwere, V., R. Tonglet, et al. (1998). "Strategies for reducing maternal mortality in developing countries: what can we learn from the history of the industrialized West?" Tropical Medicine and International Health 3(10): 771-782. De Brouwere, V. and W. Van Lerberghe (2001). "Reducing maternal mortality in a context of poverty." Safe Motherhood Strategies: a Review of Evidence, Studies in Health Services and Organisation and Policy 17: 1-33. Diop, F., A. Yazbeck, et al. (1995). "The impact of alternative cost recovery schemes on access and equity in Niger." Health Policy and Planning 10: 223-240. Dmytraczenko, T. and S. Scribner (1999). Reducing Maternal and Child Mortality in Bolivia. Executive Summary Series. Washington, DC, Partnerships for Health Reform. Ensor, T. and S. Cooper (2004). "Overcoming barriers to health service access: influencing the demand side." Health Policy and Planning 19(2): 69-79. Essien, E., D. Ifenne, et al. (1997). "Community loan funds and transport services for obstetric emergencies in northern Nigeria." International Journal of Gynecology and Obstetrics 69 Suppl. (2): S237-S244. Etard, J. F., B. Kodio, et al. (2003). "Seasonal variation in direct obstetric mortality in rural Senegal: role of malaria?" American Journal of Tropical Medical Hygiene 68(4): 503504. Farooq, S. (2003). Maternal-Newborn Health and Poverty (MNHP): A Global review of the evidence base, London School of Tropical Medicine, Health Policy Unit. Fawcus, S., M. Mbviso, et al. (1996). "A community-based investigation of avoidable factors for maternal mortality in Zimbabwe." Studies in Family Planning 27(6): 319-327. Figa'-Talamanca, I. (1996). "Maternal Mortality and the problem of accessibility to obstetric care: the strategy of maternity waiting homes." Social Science and Medicine 42(10): 1381-1390. Filmer, D. and L. Pritchett (1999). "The impact of public spending on health: does money matter?" Social Science and Medicine 49: 1309-1323. Fofana, P., O. Samai, et al. (1997). "Promoting the use of obstetric services through community loan funds, Bo, Sierra Leone." International Journal of Gynecology and Obstetrics 59 (Suppl.2): S225-S230. Freedman, L., M. Wirth, et al. (2004). Millennium Project Taskforce 4 Interim Report, Child Health and Maternal Health. New York, Mailman School of Public Health, Columbia University. Gelband, H., J. Liljestrand, et al. (2002). The evidence base for interventions to reduce maternal and neonatal mortality in low and middle-income countries. Working Paper Series 5. Geneva, WHO Commission of Macroeconomics and Health. Gertler, P. J. (2000). Final Report: The Impact of PROGRESA on Health. Washington, International Food Policy Research Institute. Gilson, L. (1997). "The lessons of user fee experience in Africa: review paper." Health Policy and Planning 12(4): 273-285. Government of India-Planning Commission (2002). National Human Development Report, 2001. New Delhi, Government of India Planning Commission. Graham, W. J., A. E. Fitzmaurice, et al. (2004). "The familial technique for linking maternal 47 death with poverty." The Lancet 363: 23-27. Gwatkin, D. (2002). Who Would Gain Most from Efforts to Reach Millennium Development Goals for Health? HNP Discussion Paper. Washington, DC, Human Development Network, The World Bank. Gwatkin, D., S. Rutstein, et al. (2004). Initial Country level Information About Socio-Economic Differences in Health, Nutrition and Population. Washington D.C, The World Bank. 2nd Edition. Gwatkin, D., S. Rutstein, et al. (2004). Socio-Economic Differences in Health, Nutrition and Population. Washington, DC, The World Bank. Haberland, N., B. Winnikoff, et al. (1999). Case Finding and Case Management of Chlamydia and Gonorrhea Infections Among Women: What We Do and What We Don't Know. New York, The Population Council. Hanson, K., M. K. Ranson, et al. (2003). "Expanding access to priority health interventions: a framework for understanding the constraints to scaling-up." Journal Of International Development 15(1): 1-14. Heise, L., M. Ellsberg, et al. (1999). Ending Violence against Women. Population Reports, Series L, Number 13. Baltimore, Johns Hopkins School of Public Health, Population Information Program. Hill, K., C. AbouZahr, et al. (2001). "Estimates of maternal mortality for 1995." Bulletin of the World Health Organization 79(3): 182-193. Hilton, P. (2003). "Vesico-vaginal fistulas in developing countries." International Journal of Gynecology and Obstetrics 82: 285-295. Hynes, M., M. Sheik, et al. (2002). "Reproductive health indicators and outcomes among refugee and internally displaced persons in postemergency phase camps." JAMA 288(5): 595603. International Road Federation (2004). World Road Statistics. Geneva, International Road Federation. Iskander, M., B. Utomo, et al. (1996). Unraveling the Mysteries of Maternal Death in West Java: Reexamining the Witnesses. Indonesia, Depok, Center for Health Research, University of Indonesia. Jalan, J. and M. Ravallion (2001). Does piped water reduce diarrhea for children in rural India? Washington, DC, The World Bank. Jejeebhoy, S. (1995). Women's Education, Autonomy, and Reproductive Behaviour: Experience from Developing Countries. Oxford, Clarendon Press. Jejeebhoy, S., M. A. Koenig, et al. (2003). Reproductive Tract Infections and other Gynaecological Disorders: Research into Prevalence, Correlates, and Consequences. Cambridge, Cambridge University Press. Kabira, W. M., E. W. Gachukia, et al. (1997). "The effect of women's role on health." International Journal of Gynecology and Obstetrics 58: 23-34. Kamara, A. (1997). "Lessons learned from the PMM Network experience." International Journal of Gynecology and Obstetrics 59(Suppl. 2): S253-S258. Kaufmann, D., A. Kraay, et al. (2003). Government Matters III: Governance Indicators for 19962002. Washington, DC, The World Bank. King, J. C. (2003). "The risk of maternal nutritional depletion and poor outcomes increases in early or closely spaced pregnancies." Journal of Nutrition 133: 1732s-1736s. Koblinsky, M. A. (1995). "Beyond maternal mortality: magnitude, interrelationship, and consequences of women's health, pregnancy-related complications and nutritional status on pregnancy outcomes." International Journal of Gynecology and Obstetrics 48 (suppl.): 48 S21-32. Koblinsky, M. A. (1999). "Organizing delivery care: what works for safe motherhood?" Bulletin of the World Health Organization 77(5): 399-406. Koblinsky, M. A. (2003). "Reducing Maternal Mortality: Learning from Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe." Koblinsky, M. A., O. R. Campbell, et al. (1993). Mother and more: a broader perspective on women's health. The health of Women: A Global Perspective. M. A. Koblinsky, J. Tyman and J. Gay. Boulder, CO, Westview Press. Koenig, M. A., V. Fauveau, et al. (1988). "Maternal Mortality in Matlab, Bangladesh:1976-85." Studies in Family Planning 19(2): 69-80. Kruger, A. M. and S. Bhagwanjee (2003). "HIV/AIDS: Impact on maternal mortality at the Johannesburg Hospital, South Africa, 1995-2000." International Journal of Obstetric Anesthesia 12(165-168). Kunst, A. E. and T. Houweling (2001). "A global picture of poor-rich differences in the utilization of delivery care." Studies in Health Services and Organisation and Policy 17(293-311). Kutzin, J. (1993). Obstacles to Women's Access: Issues and Options for More Effective Interventions to Improve Women's Health. HRO Working Paper, No. 13. Washington, DC, Human Resources Development and Operations Policy, The World Bank. Kutzin, J. (1995). Experience with organizational and financing reform of the health sector, WHO, Geneva, Division Of Strengthening of Health Services. Kwast, B. (1996). "Reduction of maternal and perinatal mortality in rural and peri-urban settings: what works?" European Journal of Obstetrics and Gynecology and Reproductive Biology 69: 47-53. Lalonde, A. B., P. Okong, et al. (2003). "The FIGO Save the Mothers Initiative: Uganda- Canada collaboration." International Journal of Gynecology and Obstetrics 80(204-212). Lloyd, T., H. M. Lin, et al. (2002). "Adolescent Caucasian mothers have reduced adult hip bone density." Fertility and Sterility 77(1): 136-140. Loudon, I. (1992). Death in Childbirth: An International Study of Maternal Care and Maternal Mortality 1800-1950. Oxford, Clarendon Press. Maine, D. A., L. Freedman, et al. (1994). Risk, Reproduction and Rights: the Uses of Reproductive Health Data. Population and Development: Old debates, New Conclusions. R. e. a. Cassen. NJ, Transaction Publishers: 203-227. Makinson, C. (1985). "The health consequences of teenage fertility." Family Planning Perspectives 17(3): 132-139. Marc, A., C. Graham, et al. (1995). Social Action Programs and Social Funds: A Review of Design and Implementation in Sub-Saharan Africa. Washington, DC, World Bank. Marchal, K., G. Kegel, et al. (2004). "Human resources in scaling up HIV/AIDS programmes: just a killer assumption or in need of new paradigms." AIDS 18(15): 2103-2104. Marston, C. and J. Cleland (2003). "Relationship between contraception and abortion: a review of evidence." International Family Planning Perspectives 28(2): 6-13. McCarthy, J. (1997). "The conceptual framework of the PMM Network." International Journal of Gynecology and Obstetrics 59 Suppl.: S15-S21. McCarthy, J. and D. Maine (1992). "A framework for analyzing the determinants of maternal mortality." Studies in Family Planning 23(1): 23-33. McGinn, T. (2000). "Reproductive health of war -affected populations." International Family Planning Perspectives 26(4): 174-180. McPake, B., D. Asiimew, et al. (1999). "Informal economic activities of public health workers in 49 Uganda: implications for quality and accessibility of care." Social Science and Medicine 47(7): 849-865. Mella, P. P. (2003). "Major factors that impact on women's health in Tanzania." Health Care for Women International 24: 712-722. Menken, J., L. Duffy, et al. (2003). "Childbearing and women's survival: new evidence from rural Bangladesh." Population and Development Review 29(3): 405-426. Meremikwu, W. (2003). Malaria in Children and Pregnant Women. Reducing Malaria's Burden. G. H. Council, Global Health Council. Midhet, F., S. Becker, et al. (1998). "Contextual determinants of maternal mortality in rural Pakistan." Social Science and Medicine 46(12): 1587-1598. Miller, J. E. (1991). "Birth intervals and perinatal health: an investigation of three hypotheses." Family Planning Perspectives 23(2): 62-70. Mswia, R., M. Lewanga, et al. (2003). "Community-based monitoring of safe motherhood in the United Republic of Tanzania." Bulletin of the World Health Organization 81(2): 87-94. Mwabu, G., J. Mwanzia, et al. (1995). "User charges in government health facilities in Kenya: effect on attendance and revenue." Health Policy and Planning 10(2): 164-170. Nahar, S. and A. Costello (1998). "The hidden cost of 'free' maternity care in Dhaka, Bangladesh." Health Policy and Planning 13(4): 417-422. Nanda, P. (1999). "Women's participation in rural credit programmes in Bangladesh and their demand for formal health care: is there a positive impact?" Health Economics 8: 415-428. Nanda, P. (2002). "Gender dimensions of user fees: implications for women's utilization of health care." Reproductive Health Matters 10: 127-134. Nasir, K. and A. Hyder (2003). "Violence against pregnant women in developing countries: review of evidence." European Journal of Public Health 13: 105-107. National Research Council (2000). The Consequences of Maternal Morbidity and Maternal Mortality: Report of a Workshop. H. E. Reed, M. A. Koblinsky and W. H. Mosely. Washington, DC, Commission on Behavioral and Social Sciences and Education, Committee on Population, National Research Council. Newbrander, W., D. Collins, et al. (2000). "Ensuring equal access to health services: user fee systems and the poor." Boston. Newman, J., M. Pradhan, et al. (2002). "An impact evaluation of education, health, and water supply investments by the Bolivian Social Investment Fund." World Bank Economic Review 16(2): 241-274. Oxaal, Z. and S. Baden (1996). Challenges to Women's Reproductive Health: Maternal Mortality. London, Report No.38, Social Development Department, DFID UK. PATH (1997). The Facts: Female Genital Mutilation. Seattle, Program for Appropriate Technology in Health. Pathmanathan, I., J. Liljestrand, et al. (2003). Investing in Maternal Health: Learning from Malaysia and Sri Lanka, The World Bank, Human Development Network. Paul, B. K. (1993). "Maternal mortality in Africa: 1980-87." Social Science and Medicine 37(6): 745-752. Pebley, A. and J. DaVanzo (1993). Maternal Depletion and Child Survival in Guatemala and Malaysia. Labor and Population Program Working Paper Series 93-18. Santa Monica, Rand Corporation. Pendse, V. (1999). "Maternal deaths in an Indian Hospital: a decade of (no) change?" Reproductive Health Matters(Special Issue on Safe Motherhood Initiatives): 119-126. Peters, D., A. Yazbeck, et al. (2002). Better Health Systems for India's Poor: Findings, Analysis, and Options. Washington, DC, World Bank. 50 Rani, M. and E. Lule (2004). "Exploring the socioeconomic dimensions of adolescent reproductive health: a multicountry analysis." International Family Planning Perspectives 30(3): 110-117. Ransom, E. and N. Yinger (2002). Making Motherhood Safer: Overcoming Obstacles on the Pathway to Care. Washington, DC, Population Reference Bureau. Rawlings, L., L. Sherburne-Benz, et al. (2004). Evaluating Social Funds a Cross-Country Analysis of Community Investments. Washington, DC, World Bank Regional and Sectoral Study. Reinnikka, R. and J. Svensson (2002). Assessing frontline service delivery. Washington, DC, The World Bank Development Research Group. Ridde, V. (2003). "Fees-for-services, cost recovery, and equity in a district of Burkina Faso operating the Bamako Initiative." Bulletin of the World Health Organization 81(7): 532538. Ronsmans, C. and O. Campbell (1998). "Short birth intervals don't kill women: evidence from Matlab, Bangladesh." Studies in Family Planning 29: 282-290. Ross, J. A. and W. L. Winfrey (2002). "Unmet need for contraception in the developing world and the former Soviet Union: an updated estimate." International Family Planning Perspectives 28(3): 138-143. Sachs, J. D., J. McArthur, et al. (2004). Millennium Development Goals Needs Assessments: Country Case Studies of Bangladesh, Cambodia, Ghana, Tanzania, and Uganda. Working Paper, Millennium Project: 1-225. Samai, O. and P. Sengeh (1997). "Facilitating emergency obstetric care through transportation and communication, Bo, Sierra Leone." International Journal of Gynecology and Obstetrics 59(Suppl. 2): S157-S164. Santelli, J., R. Rochat, et al. (2003). "The measurement and meaning of unintended pregnancy." Perspectives on Sexual and Reproductive Health 35(2): 94-101. Santiso, R. (1997). "Effects of chronic parasitosis on women's health." International Journal of Gynecology and Obstetrics 58: 129-136. Save the Children (2001). State of the World's Newborns. Washington, DC, Saving Newborn Lives Program, Save the Children. Save the Children (2002). Mothers and Children in War and Conflict. State of the World's Children 2002. Washington, DC, Save the Children. Save the Children (2004). State of the World's Mothers 2004. Washington, DC, Save the Children. Schneider, P., F. Diop, et al. (2001). Pilot testing prepayment for health services in Rwanda: results for policy directions and implementation. Technical Report No. 66. Bethesda, MD, Partnerships for Health Reform. Schneider, P. and T. Dmytraczenko (2003). Improving Access to Maternal Health Care Through Insurance. Insights for Implementers No. 3. Bethesda, MD, Partnerships for Health Reformplus. Seneviratne, H. R. and L. C. Rajapksa (2000). "Safe motherhood in Sri Lanka: a 100-year march." International Journal of Gynecology and Obstetrics 70: 113-124. Seoane, G., R. Equiluz, et al. (2003). Bolivia, 1996-2000. Reducing Maternal Mortality: Learning From Bolivia, China, Egypt, Honduras, Indonesia, Jamaica, and Zimbabwe. M. A. Koblinsky, Human Development Network, The World Bank: 83-91. Shehu, D., A. T. Ikeh, et al. (1997). "Mobilizing transport for obstetric emergencies in northwestern Nigeria." International Journal of Gynecology and Obstetrics 59(Suppl. 2): S173-S180. 51 Shen, C. and J. B. Williamson (1999). "Maternal mortality, women's status, and economic dependency in less developed countries: a cross-national analysis." Social Science and Medicine 49: 197-214. Shiffman, J. (2000). "Can poor countries surmount high maternal mortality?" Studies in Family Planning 31(4): 274-289. Sibley, L., S. Buffington, et al. (2001). "Home based life saving skills: promoting safe motherhood interventions through innovative community-based interventions." Journal of Midwifery and Women's Health 46(4): 258-266. Skoufias, E. and B. McClafferty (2001). Is PROGRESA Working? Summary of the Results of an Evaluation by IFPRI. Washington, International Food Policy Research Institute. Soucat, A., W. Van Lerberghe, et al. (2002). Marginal budgeting for bottlenecks: a new costing and resource allocation practice to buy health results. Washington, DC, Africa Region Human Development, Policy and Sector Analysis Support Team, The World Bank. Standing, H. (1997). "Gender and equity in health sector reform programmes: a review." Health Policy and Planning 12(1): 1-18. Sundari, T. (1992). "The untold story: how the health care systems in developing countries contribute to maternal mortality." International Journal of Health Services 22(3): 513528. Thaddeus, S. and D. Maine (1994). "Too far to walk: maternal mortality in context." Social Science and Medicine 38(8): 1091-1110. Tinker, A. (2000). "Women's health: the unfinished agenda." International Journal of Gynecology and Obstetrics 70: 149-158. Tinker, A. and E. Ransom (2002). Healthy Mothers and Healthy Newborns: Policy Perspectives on Newborn Health. Washington, DC, The Population Reference Bureau. Tsui, A. O., J. N. Wasserheit, et al. (1997). Reproductive Health in Developing Countries: Expanding Dimensions, Building Solutions. Washington, DC, National Academy Press. United Nations Development Program-UNDP (2003). Human Development Report, 2003. New York, United Nations Development Program. United Nations Population Fund (2001). Reproductive Health for Communities in Crisis. New York, United Nations Population Fund. United Nations Population Fund (2003). Achieving The Millennium Development Goals, Population and Reproductive Health as Critical Determinants. Population and Development Strategies. New York, UNFPA, United Nations Population Fund. 10. Upadhyay, U. D. and B. Robey (1999). Why Family Planning Matters. Population Reports, Series J, Number 49. Baltimore, Johns Hopkins School of Public Health, Population Information Program. Van Poppel, F. and C. van der Heijden (1997). "The effects of water supply on infant and child mortality: a review of historical evidence." Health Transition Review 7(2): 113-148. Venugopal, V. and U. Upadhyay (2002). Birth Spacing: Three to Five Saves Lives. Population Reports, Series L, Number 13. Baltimore, Johns Hopkins School of Public Health, Population Information Program. Wagstaff, A. (2002). Health spending and aid as escape routes from the vicious circle of poverty and health. Meeting of the British Association for the Advancement of Science. Leicester, UK. Wagstaff, A. and Claeson, M. (2004) The Millennium Development Goals for Health:Rising to the Challenges. Washington, DC, The World Bank. Ward, J. (2002). If not now, when? Addressing gender-based violence in refugee, internallydisplaced, and post-conflict settings: a global overview. New York, The Reproductive 52 Health for Refugees Consortium. Winkvist, A., K. M. Rasmussen, et al. (1992). "A new definition of maternal depletion syndrome." American Journal of Public Health 82(5): 691-694. World Bank (1996). Kingdom of Morocco, Impact Evaluation Report: Socioeconomic Influence of Rural Roads. Washington, DC, Operations Evaluation Department, The World Bank. World Health Organization (2004). Making Pregnancy Safer: The Critical Role of the Skilled Attendant: A Joint Statement by WHO, ICM, and FIGO. Geneva, Department of Reproductive Health and Research, WHO. World Health Organization (2004). Maternal Mortality Estimates for 1990 and 1995: Estimates Developed by WHO, UNICEF, and UNFPA. Geneva, Department of Reproductive Health and Research, WHO. Zabin, L. S. and K. Kiragu (1998). "The health consequences of adolescent sexual and fertility behavior in Sub-Saharan Africa." Studies in Family Planning 29(2): 210-232. 53