The Reproductive System
advertisement

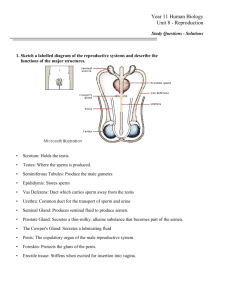
25 PART 1 The Reproductive System The Reproductive System • Primary sex organs • Testes • Ovaries • Accessory sex organs • Glands • External genitalia The Male Reproductive System • Testes are located within the scrotum • The scrotum • Skin and superficial fascia surrounding the testes • Positioning provides an environment 3C cooler than body temperature The Male Reproductive System • Dartos muscle • Is a layer of smooth muscle • Is responsible for wrinkling of scrotal skin • Cremaster muscle • Bands of skeletal muscle surrounding the testes • Elevates the testes The Testes • Are enclosed in a serous sac—the tunica vaginalis • Tunica albuginea—fibrous capsule of the testes • Divides each testis into 250–300 lobules • Lobules contain 1–4 coiled seminiferous tubules • Epididymis • Comma-shaped structure on posterior testis Nerves and Vessels • Arterial supply of the testes • Testicular arteries • Testicular veins arise from the pampiniform plexus • Pampiniform plexus helps keep testes cool • Testes innervated by parasympathetic and sympathetic divisions of ANS Microscopic Anatomy • Seminiferous tubules • Separated by areolar connective tissue • Epithelium consists of • Spermatogenic cells—sperm-forming cells • Columnar sustentocytes—support cells Microscopic Anatomy • Spermatogenic cells produce sperm • Sperm formation • 400 million sperm formed per day • Begins at puberty • Process takes 75 days • Cells differentiate and move toward the lumen • Spermatogonia—stem cells • Primary spermatocytes • Secondary spermatocytes • Spermatids • Sperm Microscopic Anatomy • Sustentocytes • Surround spermatogenic cells • Extend from basal lamina to the lumen • Tight junctions between cells • Blood testis barrier • Assist sperm production • Secrete testicular fluid and androgen-binding protein Microscopic Anatomy • Myoid cells—surround seminiferous tubules • Contract rhythmically • Interstitial endocrine cells • Secrete testosterone • Secretion regulated by LH The Epididymis • Duct of the epididymis is 6 m long (when uncoiled) • Dominated by pseudostratified columnar epithelium • Bears tufts of stereocilia—immotile, long microvilli • 20-day journey for sperm to move through • Gain the ability to swim and to fertilize an egg through the acrosomal reaction The Ductus Deferens • Stores and transports sperm • Hisotology of the ductus deferens • Epithelium—pseudostratified columnar • Thick muscularis • Adventitia The Spermatic Cord • Contains • Ductus deferens • • Testicular blood vessels Nerves • Superior portion of ductus deferens • Runs through inguinal canal The Urethra • Carries sperm from ejaculatory ducts to “outside” • Three parts of male urethra • Prostatic urethra • Intermediate part of urethra • Spongy urethra 25 PART 2 The Reproductive System Accessory Glands • The seminal glands • Lie on the posterior surface of the urinary bladder • Secrete about 60% of the volume of semen • Fluid contains • Fructose to nourish sperm • Substances to enhance sperm motility • Prostaglandins • Substances that suppress immune response against semen • Enzymes that clot and then liquefy semen Accessory Glands • The prostate • Encircles the prostatic urethra • Consists of 20–30 compound tubuloalveolar glands • Secretes about 25–30% of seminal fluid • Contains • Substances that enhance sperm motility • Enzymes that clot and then liquefy semen Accessory Glands • The bulbo-urethral glands • Pea-sized glands inferior to the prostate gland • Produce a mucus • Mucus enters spongy urethra prior to ejaculation • Neutralizes traces of acidic urine • Lubricates urethra The Penis • External anatomy • Shaft—body • Glans penis—distal expanded end • Prepuce—foreskin • Removed during circumcision The Penis • Internal anatomy • Three erectile bodies • One corpus spongiosum • Surrounds spongy urethra • Two coropora cavernosa • Contain sinuses; make up most of the penis • Male sexual response • Erection—parasympathetic control • Ejaculation—sympathetic control The Male Perineum • Contains—scrotum, root of penis, anus • Diamond-shaped area between • Pubic symphysis anteriorly • Coccyx posteriorly • Ischial tuberosities laterally Spermatogenesis • Divided into three stages • Stage 1—spermatogonia divide by mitosis • Type A—maintain the germ cells • Type B—differentiate into primary spermatocytes • Stage 2—meiosis I and meiosis II • Meiosis I—forms two secondary spermatocytes • Meiosis II—each spermatocyte forms two spermatids Spermatogenesis • Stage 3—spermiogenesis • The four spermatids differentiate into spermatozoa • Spermatozoa shed superfluous cytoplasm • Composed of • Head, midpiece, and tail Spermatogenesis • Sustentocytes surround spermatogenic cells • Bound together by tight junctions • Divides seminiferous tubules into • Basal compartment • Adluminal compartment Spermatogenesis • Tight junctions between sustentocytes • Blood testis barrier • Protects developing sperm from the immune system Spermatogenesis • Spermatogenesis • Is controlled by • Follicle-stimulating hormone (FSH) • Testosterone • Secretions from sustentocytes also influence spermatogenesis • Androgen-binding protein concentrates testosterone near spermatogeneic cells • Inhibin—inhibits FSH The Female Reproductive System • Produces gametes (ova) • Prepares to support a developing embryo • Undergoes changes according to the menstrual cycle • Menstrual cycle is the monthly cycle as it affects all female reproductive organs • Includes • Ovaries • Uterine tubes, uterus, and vagina The Ovaries • Small, almond-shaped organs • Produce ova • Held in place by ligaments and mesenteries • Broad ligament • Suspensory ligament • Ovarian ligament • Ovarian arteries—arterial supply • Innervated by both divisions of the ANS Internal Structure of the Ovaries • Tunica albuginea • Fibrous capsule of the ovary • Covered in simple columnar epithelium • Ovarian cortex—houses developing oocytes • Follicles—multicellular sacs housing oocytes • Ovarian medulla—loose connective tissue • Contains blood vessels, lymph vessels, and nerves 25 PART 3 The Reproductive System The Uterine Tubes • Receive ovulated oocyte • Parts of the uterine tube • Infundibulum—distal end of uterine tube • Surrounded by fimbriae • Ampulla—middle third of uterine tube • Usual site of fertilization • Isthmus—medial third of uterine tube The Uterus • Lies anterior to rectum—posterior to bladder • Anteverted (anteflexed) usual position of uterus • Parts of the uterus • Fundus—rounded superior portion • Cervix—“neck” of uterus • Cervical canal—communicates with vagina inferiorly • Internal os—opening connecting with uterine cavity • External os—inferior opening of cervix Supports of the Uterus • Uterus is supported by • Mesometrium—anchors uterus to lateral pelvic walls • Cardinal ligaments—horizontal from cervix and vagina • Round ligaments—bind uterus to the anterior pelvic wall Uterine Wall • Wall of the uterus composed of • Perimetrium • Serous layer—is the peritoneum • Myometrium • Interlacing bundles of smooth muscle • Contracts during childbirth • Endometrium • Mucosal lining of uterine cavity Uterine Wall • Embryo burrows into endometrium • Endometrium has two layers • Functional layer • Basal layer Uterine Wall • Uterine arteries—send branches to the uterine wall and divide into arcuate arteries • Radial arteries reach the endometrium and branch into • Straight arteries—to basal layer • Spiral arteries—to functional layer • Undergo degeneration and regeneration with menstrual cycle The Female Menstrual Cycle and Oogenesis • Monthly menstrual cycle • Due to hormonal fluctuations in ovaries and uterus • Ovarian cycle • Stimulates production of ovarian follicles and oocytes • Uterine cycle • Prepares uterine wall for implantation The Ovarian Cycle • Has three successive phases • Follicular phase • Ovulation • Luteal phase The Ovarian Cycle • Follicular phase • First half of the ovarian cycle • 6–12 primordial follicles stimulated to develop • Growth stimulated by FSH from anterior pituitary • Primordial follicle becomes a primary follicle • Zona pellucida—glycoprotein coat surrounding oocyte • Theca folliculi—internal layer secretes hormones The Ovarian Cycle • Follicular phase (continued) • Antrum forms • A fluid-filled cavity between granulosa cells • Primary follicles become a secondary follicle • Corona radiata—coat of granulosa cells surrounding oocyte • Secondary follicle enlarges and becomes • Vesicular (Graafian) follicle—ready to be ovulated The Ovarian Cycle • Ovulation • Occurs about halfway through each ovarian cycle (day 14) • One mature oocyte exits from one ovary • Enters peritoneal cavity • Swept into uterine tube • Sudden increase in LH is signal for ovulation The Ovarian Cycle • Luteal phase • Occurs after ovulation in last half of the ovarian cycle • Remaining follicle becomes a corpus luteum • Secretes progesterone • • Acts to prepare for implantation of an embryo If no implantation • Corupus luteum dies and becomes a corpus albicans Oogenesis • Takes many years to complete • Primordial follicles are arrested (stalled) in meiosis I • Surge of LH also causes primary oocyte to compete meiosis I Oogenesis • Oogenesis produces only one ovum and three polar bodies • Polar bodies do not contribute to developing embryo • Meiosis II is completed only if sperm penetration occurs The Uterine Cycle • Series of cyclic phases of the endometrium • Phases coordinate with the ovarian cycle • Endometrial phases directed by FSH and LH • Phases of uterine cycle • Menstrual phase—days 1–5 • Stratum functionalis is shed • Proliferative phase—days 6–14 • Secretory phase—days 15–28 The Vagina • Consists of three coats • Adventitia—fibrous connective tissue • Muscularis—smooth muscle • Mucosa—marked by transverse folds • Consists of lamina propria and stratified squamous epithelium • Hymen—an incomplete diaphragm • Fornix—recess formed at the superior part of the vagina 25 PART 4 The Reproductive System External Genitalia and Female Perineum • Mons pubis • Overlies the pubic symphysis • Pubic hair covers after puberty • Labia majora • Homologue of the male scrotum • Encloses the labia minora • Vestibule • Space between the labia minora • Houses opening to urethra and vagina External Genitalia and Female Perineum • Clitoris • Anterior to vestibule • Is erectile tissue • Homologous to the penis • Female perineum • Anterior boundary—pubic arch • Posterior boundary—coccyx • Lateral boundaries—ischial tuberosities The Mammary Glands • Breasts—modified sweat glands • Glandular structure—undeveloped in nonpregnant women • Milk production—starts at or after childbirth Pregnancy • Events leading to fertilization • Sperm binds to the zona pellucida • Undergoes the acrosomal reaction • Release of enzymes to form a slit in the zona pellucida • Fusion of oocyte and sperm plasma membranes • Cortical reaction • Enzymes prevent any other sperm from binding to the egg • Fertilization—chromosomes of male and female gametes join 25 PART 5 The Reproductive System Implantation • Blastocyst begins implantation • About 6 days after conception • Blastocyst consists of • An inner cell mass and outer trophoblast • Trophoblast forms two layers • Cytotrophoblast—inner layer • Syncytiotrophoblast—outer layer Placenta Formation • Embryonic and maternal tissues contribute to the placenta Anatomy of the Placenta • Exchanges across the chorionic villi between maternal and fetal blood • Provide fetus with nutrients and oxygen • Dispose of its wastes • Allow hormonal signals to be sent to the mother • By week 13 the placenta is fully formed Anatomy of the Placenta • Placental barrier consists of • All three layers of the chorionic villi • Sugars, fats, and oxygen • Diffuse from mother to fetus • Urea and carbon dioxide • Diffuse from fetus to mother Anatomy of the Placenta • Syncytiotrophoblast • Secretes substances that regulate events of pregnancy • Maternal antibodies are transported across placenta • Viruses, alcohol, and heroin cross the placental barrier 25 PART 6 The Reproductive System Childbirth • Parturition—266 days after fertilization • Labor—events that expel the infant from the uterus Reproductive System Cancers in Males • Testicular cancer • Affects 1 of 50,000 males • Commonly from early-stage spermatogenic cells • Increase of 50% from 1974 to 1990 • Cured in 95% of cases Reproductive System Cancers in Males • Prostate cancer • Slow-growing • Arises from peripheral glands • Risk factors • Fatty diet • Genetic predisposition Reproductive System Cancers in Females • Ovarian cancer • Arises from cells in the germinal epithelium • Endometrial cancer • Arises from the endometrium of the uterus • Cervical cancer • Slow-growing, arises from epithelium at the tip of the cervix • Often caused by human papillomavirus (HPV) Reproductive System Cancers in Females • Breast cancer • Second most common cause of cancer deaths in women • 97% of cases occur in women over 50 • Treatment • Surgical removal of the mass (lumpectomy) • Radiation therapy • Administration of selected hormones • Chemotherapy Embryonic Development of the Sex Organs • Embryo at 5–6 weeks is sexually indifferent • Mesonephric ducts • Future male ducts • Paramesonephric ducts • Future female ducts Embryonic Development of the Sex Organs • Male embryos—sexual differentiation begins in week 7 • Mesonephric duct becomes • Epididymis • Ductus deferens • Ejaculatory duct • Paramesonephric ducts degenerate Embryonic Development of the Sex Organs • Female embryos—sexual differentiation begins in week 8 • Cortical portion of immature ovaries form ovarian follicles • Paramesonephric duct becomes • Uterus • Uterine tubes • Superior part of vagina • Mesonephric ducts degenerate Puberty • Period of life between ages 10 and 15 • Reproductive organs grow to their adult size • Events of puberty occur in the same sequence in all individuals • Age at which events of puberty occur varies widely Puberty • Male secondary sex characteristics • Enlargement of the scrotum and testes (about age 13) • Appearance of pubic, axillary, and facial hair • Lengthening of vocal folds—deepening voice • Musculoskeletal system increases in mass • Sexual maturation—mature sperm in semen Puberty • Female secondary sex characteristics • Budding breasts (around age 11) • Menarche—the first menstruation Puberty • Other estrogen-induced secondary sex characteristics • Increase in subcutaneous fat • Widening and lightening of the bones of the pelvic girdle • Appearance of axillary and pubic hair • Estrogen-induced growth spurt from age 12 to 17 Menopause • Female reproductive peak—late 20s • Around age 35—rate of follicle degeneration increases • Ovulation and menstruation cease—age 46–54 • Ovaries stop secreting estrogen • Reproductive organs and breasts begin to atrophy