Normalizing Doctor`s Compensation
advertisement

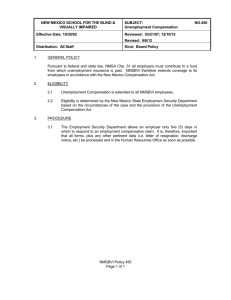
Medical Business Valuations: Normalizing Doctor’s Compensation BY: REED TINSLEY CPA, CVA AND PAUL FRENCH CPA/ABV, CVA, BVAL, CFE, CFFA, CDFA, CFD, CM&AA, CPIM, FCPA, CRFA, CMEA Reprinted from the September 2008 issue of the National Litigation Consultants’ Review Over the years, we have seen a number of different methods used by valuators to normalize physician-owner compensation; some good and some outrageously improper. In this article we will discuss what we believe is the most accepted method of determining reasonable physician-owner compensation and common errors we have seen. Background Physician-owner’s compensation generally consists of two components: 1. compensation for the services that the physician renders in the practice, including administrative and patient related services and 2. a return or a dividend on the physician’s investment in the practice. The return on investment component paid to the physician-owner can sometimes be as much as the salary (services rendered) component compensation. Consider the physician-owner who ordinarily would make about $250,000 per year according to published survey reports, but because of increased productivity of associate, non-owner physicians and/or mid-level providers, ancillary services and/or tremendous practice, rather than personal, goodwill; he or she is compensated at approximately $350,000 per year. The $100,000 difference theoretically represents a return on the physician’s investment, rather than compensation for services rendered. The actual compensation may also be driven by available cash, or by a desire to avoid personal service corporation tax rates. Normalizing Physician-Owner’s Compensation An adjustment to normalize physician-owner compensation may be required so that owner compensation from the medical practice represents approximatelywhat it would cost to hire a replacement physician(s): in the same geographic area as the subject practice, and who would perform the same duties as the current physician-owner, and who would produce a revenue stream comparable to the current physician-owner thus resulting in “reasonable, local market” replacement compensation. In other words, any dividends or return on investment, as opposed to compensation for medical services rendered, are stripped out of the subject practice’s compensation expense. Physician Market Compensation Studies To arrive at a reasonable, local market replacement compensation figure for the subject physician-owner, the valuator should compare the actual compensation to a peer comparison set of compensation data. Two of the commonly used, generally accepted peer data sets are developed by the Medical Group Management Association (MGMA) and by American Medical Group Association (AMGA). The MGMA’s Physician Compensation and Production Survey 2007 Report (www.mgma.com) allows users to compare and learn more about the factors affecting market rate of compensation and production. The report includes: Data on more than 52,000 physicians and non-physician providers categorized by specialty; Data on more than 2,300 group practices categorized by their specialty or multispecialty; Data reported for more than 100 physician specialties and more than 25 nonphysician provider specialties; More than ten performance ratios to illustrate the relationship between compensation and productivity; and Productivity measures of collections for professional charges, gross charges, ambulatory encounters, hospital encounters, surgical/anesthesia cases as well as total and physician work relative value units (RVUs). Like MGMA, AMGA’s Medical Group Compensation and Financial Survey 2007 Report (www.amga.org) was compiled from data submitted by medical groups from across the nation. These 222 medical practices reported 43,293 providers, for an average of 195 providers per group. The report provides compensation data by percentile, compensation to productivity ratios, compensation to Work RVU ratios, gross productivity, and patient visit data. It also provides Work RVUs — The professional component of total relative value units (RVUs), as measured by the Resource Based Relative Value Scale (RBRVS), not weighted by a conversion factor attributed to ambulatory care, inpatient care, and other professional services of each physician and allied healthcare professional in the medical group. The MGMA and the AMGA studies are not cheap; but they are worth their price in many valuations. Arriving at a Reasonable Physician-Owner Compensation Figure One significant mistake we have seen valuators make when valuing medical practices is blindly using the “median” or “mean” compensation figure from these surveys (or any survey for that matter) to determine the reasonable, local market physician-owner replacement compensation. To be correct, the valuator must determine the appropriate compensation based on the subject physician’s productivity. Think in terms of getting paid for the revenue that you generate. Generally the valuator should determine where the subject physician’s actual “production” falls in comparison to the overall study data for physicians in the same specialty in the same geographic area of the country. Use this comparison to determine where the reasonable replacement compensation number falls in the study data such as in the 25th, 50th, 75th, or even the 90th percentile (or somewhere in between these). The following table demonstrates what might be the appropriate market level compensation for a physician owner in a hospital based medical specialty based upon the collections for professional charges that he was responsible for during 2006 as reported by MGMA. The table also compares this reasonable market compensation to the physician’s actual compensation. Even without a thorough analysis, this table indicates that “Subject Dr.” owner’s compensation is in the broad range of reasonable market compensation for a physician in the same medical specialty, in the same geographic area, producing comparable collections. If his collections were $694,000, the valuator might use an average of the 50th and 75th percentile compensation, an extrapolation or even a trend line to determine the reasonable compensation based on the study data. Southern Region of the United States MGMA 2007 Report Based on 2006 Data Percentile Compensation Collections th 50 $400,274 $634,901 75th $467,000 $751,901 th 90 $543,026 $868,637 Subject Dr. $576,392 $958,429 In the military we learned that “Two is One and One is None.” Consequently, in a litigation situation it might be a good idea to do two separate calculation methods: first, fine tune the answer within the Percentiles, then compare the two calculations and use professional judgment to select your result and define its level of precision. In addition to the Productivity/Collections comparison, some valuators also consider the relative value comparison to remove the medical practice’s fee schedule and payer mix from the analysis – a poor payer mix might result in poorer than usual collections for a specific physician and a high fee schedule might overstate his or her gross productivity. Common Mistakes When determining a physician owner’s reasonable local market compensation in any medical practice valuation, keep these issues in mind: Don’t use Integra or RMA information as your only data source. (We have seen this more than once.) Integra and RMA do not consider the different medical specialties or geographic regions. Don’t blindly use median/mean compensation – always include some measure of physician productivity in your compensation analysis. (Yes, we are repeating ourselves on purpose.) Make sure there are enough reporting medical practices to support your analysis. If the survey includes only 5 reporting practices in your geographic area, consider expanding to the entire country or looking for a somewhat similar specialty. (Think in terms of what you do in a Guideline Merged and Acquired Company Market valuation method when you have insufficient transaction data in the subject Company SIC code.) Make sure you understand exactly what physician services are included in the reported survey productivity numbers when making your comparisons – make sure you are comparing apples to apples in your analysis. Consider if the subject physician’s productivity could be over- or understated for any reason: over- or under-coding, a fee schedule that is too high or too low, inclusion of midlevel productivity as the supervising physician’s production, etc. Consider whether the subject physician-owner’s compensation is being reduced by internal practice buy-in allocations or other factors that may significantly impact your analysis conclusions. Reed Tinsley, CPA is a Houston-based CPA, Certified Valuation Analyst, and healthcare consultant. He works closely with physicians, medical groups, and other healthcare entities with managed care contracting issues, operational and financial management, strategic planning, and growth strategies. He is the author or co-author of several healthcare related books including Valuation of a Medical Practice. His entire practice is concentrated in the health care industry. Please visit www.rtacpa.com. Paul French’s practice focuses on Forensic Accounting, Business Valuation, and Litigation Support. His testifying experience includes cases concerning damages, legal and business valuator malpractice, fraud, lost profits, business valuation, marital dissolution, shareholder oppression and other financial matters. He is the Chairman of NACVA’s Executive Advisory Board and is the Chairman of the Texas Society of CPA’s statewide Business Valuation, Forensics and Litigation Services (BVFLS) Committee (4th consecutive term). Mr. French’s practice is located in Plano, TX, a Dallas suburb, and he can be reached at 972424-1133 or at paul@frenchcpa.com.