outline6062
advertisement

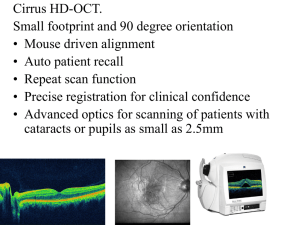
1 I. Optic Disc Topography-HRT II, Heidelberg Engineering, Inc. A. Principles 1. 2. 3. 4. 5. B. Obtaining an Image 1. 2. 3. 4. 5. 6. 7. C. The series begins with the focal plane located in the vitreous Focal plane moves posteriorly through the optic nerve head until it reaches the retina 32 confocal 2-D images are obtained in 1.6 sec. A matrix is constructed consisting of 256X256 (65,536) height measurements (measuring points) Each height is represented as a color - bright = excavated areas (cup) - dark = elevated areas (retina) Three image series are taken and averaged Pupil dilation not required HRT II Display 1. 2. 3. 4. 5. 6. D. Uses a confocal laser scanning system 670 nm diode laser Objects are scanned sequentially in two dimensions (optic sections) Sections are imaged layer by layer to form a three-dimensional image Provides three-dimensional imaging of the optic nerve head Provides objective information about macular thickening Fundus Image Computed average disc topography image of three captured series Stereometric parameters of disc topography Mooresfiled Regression Analysis display – neuroretinal rim (green) and cup (red) Results compared against normative database of 112 Caucasians Topography classified a. Within Normal Limits b. Borderline c. Outside Normal Limits Applications of Optic Nerve Head Topography 1. 2. Quantitative description and classification at first visit and change over time Quantification of stereometric parameters a. disk area b. cup and rim area and volume c. mean and maximum cup depth d. cup shape i. the more negative value the better e. retinal nerve fiber layer (RNFL) topography 2 i. 3. Uses an artificial reference plane located 50 microns below the retina to differentiate neuroretinal rim (above 50 microns) from cup (below 50 microns) HRT II is most clinically useful for documenting change over time. II. Optical Coherence Tomograpy (OCT3), Carl Zeiss Meditec, Inc. A. Principles 1. 2. 3. 4. B. Infrared light (850 nm) from a diode is directed into the retina Backscattered light is detected from several retinal layers and resolved using Low Coherence Interferometry to produce high resolution cross sections (10 um with OCT3) Resulting image looks like a histological slide section of the retina a. can differentiate 6-7 retinal layers Pupil dilation not required OCT Displays 1. Optic Disc Topography a. Cross-sectional display in 6 different merdians b. Quantification of stereometric parameters of the disc, neuroretinal rim and cup 2. Macular Analysis a. Thickness measurements i. In a 1mm circular area around the fovea ii. Four juxtafoveal sectors 3.00 mm from the fovea iii. Four extrafoveal sectors 6.00 mm from the fovea 3. RNFL Analysis a. RNFL thickness measurement displayed in 12 clock hours 1.73mm from the edge of the ONH C. Clinical Applications of OCT3 1. 2. 3. 4. 5. 6. 7. Increases in retinal thickness secondary to vascular disease and venous-occlusive disease Retinal elevations (serous retinal detachments) Choroidal neovascular membranes Macular hole Vitreo-retinal traction Juxtapapillary nerve fiber layer loss (3.4mm circular scan) Optic nerve head topography measurements III. Scanning laser Polarimetry (GDxVCC), Carl Zeiss Meditec, Inc. A. Principles 1. 2. Uses principle of birefringence of layered structures in the eye (like the RNFL) which cause retardation of polarized light as an indirect measure of the thickness of the nerve fiber layer Birefringent (layered) structures in eye 3 a. b. c. cornea (lamellae) lens retinal (RNFL) 3. To isolate RNFL birefringence, GDx uses a corneal compensator to cancel out corneal birerefringence; the lens of the eye has minimal birerefringence 4. B. Measures the thickness of the retinal NFL (65,536 points) in an area 15 degrees X 15 degrees around the optic nerve head a. The thicker and more robust the NFL, the greater the retardation GDxVCC: Screening for Retinal Nerve Fiber layer (RNFL) Loss 1. 2. C. Images acquired in 0.7 sec Pupil dilation not necessary GDxVCC Display 1. 2. 3. 4. 5. D. 1. 2. 3. E. 1. Fundus image Thickness Map a. Bright colors (yellow and orange) = thicker areas of RNFL i. superior and inferior to ONH b. Dark blue colors = thinner areas of RNFL i. nasal and temporal to ONH ii. defects in NFL sup/inf Thickness parameters Deviation Map TSNIT Curve GDx: The NFI (Nerve Fiber Indicator) NFL measurements are assigned a “number” between 0 and 98 The NFI is a computer-generated neural net number that represents the artificial intelligence of a computer that has been trained to distinguish norman RNFL patterns from glaucomatous RNFL patterns. General Categories: a. The number 30 correctly classifies 90% of patients into normal or abnormal i. 0-30: Normal ii. over 30: RNFL Loss GDxVCC Serial Analysis Displays up to 4 images per eye on one page-for follow-up 4 IV. Optos Retinal Exam, Optos, Inc A. 1. 2. 3. 4. 5. 6. 7. V. Principles Uses a scanning laser ophthalmoscope to digitally image the fundus Couples a green laser (532 nm) that scans the sensory retinal through the RPE with a red laser (633 nm) that scans deeper structures from the RPE to the deep into the choroid Provides a 200 degree view Does not require pupil dilation Captures images in 0.25 sec per eye Useful for detection of central and peripheral abnormalities without pupil dilation Two lasers help differentiate retinal lesions from choroidal lesions Pascal Dynamic Contour Tonometry (DCT), Zeimer Ophthalmics, Inc. A. 1. 2. 3. 4. B. 1. 2. Principles A contoured tonometer tip that fits into the tip holder of a standard Goldmann Applanation Tonometer (GAT) Applies pressure to the cornea with a constant force DCT measurements are not influenced by changes in corneal thickness DCT is equal in accuracy to IOP measurements with traditional Goldman Applications Studies have demonstrated that DCT is more accurate that GAT for corneas thinner than 450 nm and thicker than 550 nm Is also useful for accurately measuring IOP in post-LASIK patients and other thin corneas