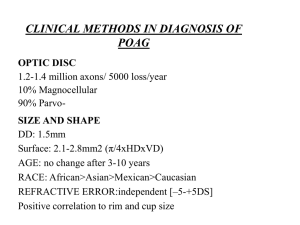
Evaluation of preperimetric glaucoma CHAIRPERSON -Dr. H T Venkategowda MODERATOR - Dr. Spoorthy S PRESENTER : Dr. Malvika Suresh Definition POAG- A chronic, progressive, anterior optic neuropathy that is accompanied by a characteristic cupping and atrophy of the optic disc with corresponding visual field loss. Preperimetric glaucoma (PPG) is defined as the presence of characteristic glaucomatous changes in the optic disc and increased vulnerability to damage in the retinal nerve fiber layer (RNFL), without the presence of visual field defects detectible with standard automated perimetry. NEED FOR EARLY DIAGNOSIS Studies have proved that structural changes in glaucoma (ONH, RNFL) preceed functional changes Glaucoma is a continuum. Optic nerve maybe abnormal WITHOUT glaucoma This has a great potential value in delaying and avoiding progression of the disease Indications for early diagnosis 1. 2. 3. 4. 5. Family history Raised IOP Increase in size of cup Difference in size of cup Associated disease state - diabetes mellitus Pre perimetric Glaucoma diagnosis & monitoring require 3 main tests 1. SCANNING LASER POLARIMETRY (GDX) 2. CONFOCAL SCANNING LASER OPHTHALMOSCOPY (HRT) 3. OPTICAL COHERENCE TOMOGRAPHY 1. Scanning laser polarimetry ● Scanning laser polarimetry is an imaging technology to measure peripapillary RNFL thickness ● GDX is a device that uses this technology ● Latest generation - GDX VCC (variable corneal compensator) ● Evaluates the site of damage before patient experiences visual loss ● Total chair time less than 3 minutes for both eyes ● Undilated pupils work best, no drops required ● Painless procedure, safe, ● Principle - BIREFRINGENCE ● Phenomenon of double refraction where a ray of light when incident on a birefringent material is split by polarization into 2 ways taking slight different paths. ● Main birefringent intraocular tissues - cornea, lens and retina ● In the retina, the parallel arrangement of the microtubules in retinal ganglion cell axons causes a change in the polarization of light passing through them. ● The change in the polarization of light is called retardation ● The retardation value is proportionate to the thickness of the RNFL ● Technique - ● 780nm DIODE laser ● The scan is obtained by the use of an 3.2mm fixed ellipse centered over the optic disc as seen in reflectance map ● Data is displayed as color coded grids which displays a ‘heat map’ - representing different levels of retardation and therefore RNFL thickness. ● VCC stands for variable corneal compensator, which was created to account for the variable corneal birefringence in patients. ● Uses the birefringence of Henle’s layer in the macula as control for measurement of corneal birefringence GDX PRINTOUT ● PATIENT DATA: patient data and quality score - the patient’s name, date of birth, gender and ethnicity are reported. An ideal quality score is from 7-10. ● FUNDUS/ REFLECTANCE IMAGE -useful to check image quality ● Every image has a Q score representing the overall quality of the scan ● The Q ranges from 1-10, with values 8-10 representing acceptable quality ● This score is based on a no. of factors including - well focussed, evenly illuminated, optic disc well centered and ellipse is properly around the ONH ● The calculation circle is the area found in between the two concentric circles, which measure the TSNIT and Nerve fibre indicator (NFI) parameters. ● By resizing the calculation circle and the ellipse, the operator is able to measure beyond a large peripapillary atrophy area RNFL thickness map ● A color coded format from blue to red. ● Hot colors like red and yellow mean high retardation or thicker RNFL ● Cool colors like blue and green mean low retardation / thinner RNFL ● A healthy eye has yellow and red colors in the superior and inferior regions representing thick RNFL regions and blue and green areas nasally and temporally representing thinner RNFL areas ● In glaucoma, RNFL loss will result in a more uniform blue appearance TSNIT map ● TSNIT displays the RNFL thickness values along the calculation circle in relation to normal range ● Normal eye - typical “double hump” pattern ● Healthy eye - there is good symmetry between the TSNIT graphs of the two eyes and the two curves will overlap ● In glaucoma - one eye often has more advanced RNFL loss and therefore the 2 curves will have less overlap Green and pink shaded areas of normality, over which a black line is drawn to demonstrate patient’s RNFL thickness TSNIT symmetry graphR & L superimposed on each other Deviation map ● Reveals the location and magnitude of RNFL defects over the entire thickness map. Color coded pixels indicate amount of deviation. ● Compared to the age matched normative database ● Dark blue squares - RNFL thickness is below 5th percentile of the normative database ● Light blue squares - deviation below the 2% level ● Yellow - deviation below 1% ● Red- deviation below 0.05% Nerve fibre indicator ● An indicator of likelihood that an eye has glaucoma ● Calculated using an advanced form of neural network, called a support vector machine (SVM) ● Output values range from 1-100 1-30 = low likelihood for glaucoma 31-50 = glaucoma suspect 51+ = high likelihood of glaucoma Quality assesment ● Appropriate focusing and illumination of retina. ● Ellipse must be centered over ONH Review of GDx LIMITATIONS STRENGTH ● No pupil dilatation ● Rapid data on RNFL ● Large normative database ● Sensitivity and specificity to detect glaucoma >80% ● ● ● ● Only RNFL information Corneal surgery will induce error (if no VCC) Macular pathology is a hinderance NFI -proprietary value 2. Confocal scanning laser ophthalmoscopy (HRT) ● CSLO is a rapid, non-invasive, non contact imaging technology ● Heidelberg Retina Tomography is the major commercially available instrument that uses this technology ● 3 generations - HRT, HRT 2, HRT 3 ● Gives 3-D images- high resolution ● Principle - spot illumination and spot detection ● Stimulus - 670 micron DIODE laser ● Uses laser light instead of a bright flash of white light to illuminate the retina ● Conjugated pinholes are placed in front of the light source and light detector and allow only light originating from a determined focal plane to reach the detector. ● Sequential sections are obtained by moving through the whole depth of tissue - in this case the optic nerve. ● Oscillating mirrors in the HRT redirect the laser beam to the x and y axis (which is perpendicular to the optic axis). A bi-dimensional image is obtained at each focal plane. What the HRT does ● Once the patient is positioned, HRT 2 automatically performs a pre-scan through the optic disc to determine the depth of the individual’s optic nerve ● Next, it determines the number of imaging planes to use (range of scan depth 1-4mm) ● Each successive scan plane is set to measure 0.0625mm deeper ● Automatically obtains 3 scans for analysis ● Aligns and averages the scans to create the mean topography image ● A series of 32 confocal images each 256x256 pixels is obtained in a duration of 1.6 secs ● Computer converts 32 confocal images to a single topographic image in approximately 90 secs. ● Once image is taken, operator indicates the optic nerve contour line over the reflectance or topography image. ● Reference plane - located 50 microns posterior to the mean height along a 6deg arc of contour line at temporal inferior sector ● HRT 3 provides ONH stereometric analysis without manual delineation of disc. ● Stereometric parameters are calculated by the machine and analysed by A1 classifier - Relevance Vector Machine(RVM). Then a Glaucoma Probability Score is created. HRT REPORT HRT III HRT II PATIENT DATA ● Provides information on exam type (initial report/baseline/follow up), patient demographic information ( patient name, age, gender, ethnicity, etc) and basic image information including image focus position and whether astigmatic lenses were used during acquisition, TOPOGRAPHIC IMAGE ● On left upper corner ● A false color image ● Color coded representation of disc ● Superficial areas- darker ● Deep areas - lighter ● Red - cup ● Blue, green - NRR Blue - sloping rim Green - non sloping rim REFLECTION IMAGE ● On right upper corner in u/l report, below topographic image in OU report ● Brighter areas - higher reflectance - cup ● Darker areas - less reflectance ● Valuable in locating and drawing the contour line around the disc margin ● In the reflectance image the optic nerve head is divided into 6 sectors ● Depending on this patient’s age and overall disc size the eye is then statistically classified as : HORIZONTAL and VERTICAL HEIGHT PROFILE ● Height profile along the white horizontal line in the topography image ● Height profile along the white vertical line in the topography image ● The subjacent reference line (red) indicates the location of the reference plane (separation between cup and NRR) ● The 2 black lines perpendicular to the height profile denote the borders of the disc as defined by the contour line. MEAN CONTOUR HEIGHT GRAPH ● After the contour line is drawn around the border of the optic disc, the software automatically places a reference plane parallel to the peripapillary retinal surface located 50 um below the retinal surface ● The reference plane is used to calculate the thickness and cross-sectional area of the RNFL. ● The parameters of area and volume of the NRR and optic cup are also calculated based on the location of the reference plane. CUP = area of the image that falls below the reference plane. NRR = above the reference plane ● Normal contour - DOUBLE HUMP - humps correspond to the superior and inferior NFL, which are normally thicker ● Green contour line should never go below red ref. Plane. If it does, then contour like likely not in proper position ● The graph depicts from left to right T-TS-NS-N-NI-TI-T STEREOMETRIC ANALYSIS ● Hrt 2- 14 parameters ● HRT 3- 6 parameters ● Each value is designated as MOORFIELDS REGRESSION ANALYSIS (MRA) Glaucoma probability ● New software included in HRT 3 ● Based on construction of a 3-D model of ONH and RNFL by using 5 parameterscup size & depth, rim steepness, horizontal & vertical RNFL ● Employs artificial intelligence: relevance vector machine and derives probability of glaucoma of scanned eye after comparing it to a predetermined model ● - probability </= 28% - WNL ● - probability >/= 28% - BL ● -probability >/= 64% -ONL HRT can differentiate between normal and early glaucomatous eyes with a sensitivity of 79% to 87% and specificity of 84% to 90%. Unlike the MRA, the GPS utilizes the whole topographic image of the optic disc, including the cup size, cup depth, rim steepness and horizontal/vertical RNFL curvature whereas the MRA uses only a logarithmic relationship between the NRR and optic disc areas Quality indicators ● Even luminance ● Sharp borders of topography and reflectance 11-20= very good images 21-30= good ● Good centration of the disc 31-40= acceptable ● Manufacturer’s classification by standard 41-50= poor deviation --> ● <10 = excellent >50 =very poor Review of HRT LIMITATIONS STRENGTH ● No pupil dilatation ● Rapid 3D data on ONH ● Software available for longitudinal change analysis ● ● ● ● Operator draws contour line (except in HRT 3) Reference plane affects data outcome Blood vessels often included in rim area Less useful for analysis of macula or RNFL 3. Optical coherence tomography (OCT) ● It is an imaging technology that measures intensity and echo-time delay of back scattered and back reflected light from scanned tissues. ● Developed in 1991 ● High resolution cross sectional imaging of ONH, RNFL, macula ● Generations - OCT 1,2,3 (stratus), Spectral ● Light source - 820 or 850nm IR DIODE laser ● PRINCIPLE- low coherence interferometry & the ability to differentiate retinal layers depending on the different time delay of their reflections ● High reflectivity tissues (white and red colors) - NFL, RPE and choriocapillaries ● Low reflectivity tissues (blue and black colors) - photoreceptor layer, choroid, pockets of fluid ● Advantage- can scan RNFL, ONH and macula ● Resolution - 8-10 microns OCT REPORT Healthy eye (RE) Glaucomatous eye (LE) Peripapillary RNFL scan ● 3.4 mm circular scan around ONH ● RNFL curve starts with temporal quadrant & continues clockwise in RE, counterwise in LE. ● Thickness values are provided for 4 quadrants & each clock hours ● Classification based on normative database is color coded - green = WNL - yellow = borderline - red = ONL ● Average RNFL is also established. ONH SCAN ● 6 linear scans (length=4mm) ina spoke fashion obtained ● Automatically defines ONH margins at the end of RPE layer (blue cross). Straight line is drawn joining the blue crosses. ● Reference plane - parallel line drawn 150 microns anterior to previous line ● Tissues above reference plane - rim (Red) ● Tissues below - cup (contour -green & edge - yellow) ● One radial scan is yellow denoting the axis of cross-sectional image in the printout Ganglion cell complex (GCC) analysis ● Measurement of retinal thickness at the macula in an attempt to detect early stage glaucomatous damage Review of OCT LIMITATIONS STRENGTH ● Highest axial resolution ● image can be compared with histology slides ● Rapid data on RNFL, ONH and macula ● ONH margin determined by device ● No need for pupil dilation ● Detects different pathologies ● Easy to operate, safe ● ● ● Limited normative database Data originate from only 1 set of scans Limited programs for longitudinal evaluation glaucomatous progression Conclusion ● ● ● ● Proven advantages in early diagnosis and monitoring of glaucoma Limitations : Disability to capture all nuances of appearance as instereo- photographs Cannot discriminate glaucoma in difficult optic discs (high myopia , tilted optic disc) ● Hence , these modalities cannot replace the gold standards of functional and structural tests but can definitely compliment them in clinician’s decision making process.