Complement
advertisement

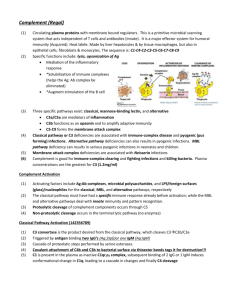
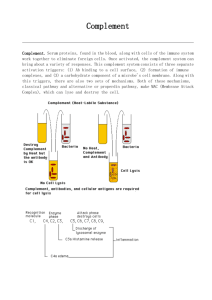
Complement Complement Pathways: General Features 1. family of proteins made by liver 2. many found as zymogens 3. proteolytic fragments can function as effector molecules to: a. facilitate interaction of phagocytes to induce opsonin-mediated phagocytosis b. induce osmotic lysis of microbes (MAC) c. enhance vascular permeability by inducing degranulation of mast cells/basophils d. induce chemotaxis of neutrophils e. facilitate immune complex elimination 4. Two pathways: classical and alternative generate common fragment “C3b” and converge into a common pathway Alternative complement pathway: Activation 1. 2. 3. 4. 5. 6. 7. 8. 9. involved in innate immunity spontaneously generated C3b by tickover binds to microbe Factor B binds to microbe Factor D cleaves Factor B Ba, Bb C3bBb = alternative pathway C3 convertase a. stabilized by properdin C3bBb cleaves C3 C3a, C3b C3bBbC3b = alternative pathway C5 convertase C3bBbC3b cleaves C5 C5a, C5b terminal pathway membrane attack complex Classical complement pathway: Activation 1. immune complex formation with either IgG or IgM (IgM more effective) 2. C1 binds to Fc region of antibody 3. C1 cleaves C4 C4a, C4b 4. C2 binds next to C4b 5. C2 cleaved by C1 C2a, C2b 6. C4b2a = classical pathway C3 convertase 7. C4b2a cleaves C3 C3a, C3b 8. C4b2a3b = classical pathway C5 convertase 9. C4b2a3b cleaves C5 C5a, C5b 10. terminal pathway membrane attack complex Terminal complement pathway: Activation 1. activation of alternate or classical pathway C5b formation of MAC insertion of MAC into target membrane osmotic lysis and death of microbe Complement Biological Activities C3a and C5a 1. anaphylatoxins 2. bind to receptors on mast cells and basophils degranulation histamine increases vascular permeability cells migrate from blood into tissues 3. C5a is chemotactic for neutrophils 4. histamine + chemotaxis of neutrophils inflammatory response 5. C4a is only generated by classical pathway C3b 1. 2. 3. 4. opsonin if put on surface of microbe if put on immune complexes facilitates their elimination amplifies complement activity via alternative pathway required for formation of C5 convertase of alternative and classical pathways C5b 1. stimulus for formation of membrane attack complex (C5b, C6, C7, C8, C9) C2b 1. weak kinin increase vascular permeability contributes to inflammation Complement Regulation 1. complement proteins are species specific 2. Factor I – inactivates C3b and C4b iC3b, iC4b 3. Factor H – binds fluid phase C3b preventing its attachment to cells a. dissociates alternative pathway C3 convertase by binding C3b competitively 4. DAF – binds membrane bound C4b and C3b prevent formation of C3 convertases a. promote dissociation of convertases by binding C4b and C3b competitively 5. C4bp – binds fluid phase C4b preventing its attachment to cells a. dissociates classical C3 convertase by binding C4b competitively 6. CR1 – binds membrane bound C4b and C3b prevent formation of C3 convertases 7. MCP – cofactor for Factor I 8. AI – binds to C3a, C4a, C5a preventing their binding to mast cell receptors 9. C1 INH – inhibits C1 prevents spontaneous activation of classical pathway a. inactivates kallikrein 10. MAC INH incluce HRF, S-protein, CD59 Complement and Coagulation Pathways are Linked Via Kallikrein Intrinsic coagulation pathway generates kallikrein Factor XII –– tissue damage Factor XIIa prekallikrein –– Factor XIIa kallikrein Factor XII –– kallikrein Factor XIIa [amplification] C5 –– kallikrein C5a + C5b kininogen –– kallikrein kininogen(a) + bradykinin (vasodilator, increases vascular permeability) 6. kallikrein is inhibited by C1 INH 1. 2. 3. 4. 5. Complement Genetic Deficiencies C1 esterase inhibitor deficiency (C1 INH) 1. 2. 3. 4. associated with the disease hereditary angioedema (HAE) recurrent facial/tongue and laryngeal edema edema of GI tract colic or diarrhea overproduction of C4a (weak anaphylotoxin) and C2b (weak kinin) causing histamine release and vasodilation respectively 5. C5a and bradykinin produced vasodilation 6. vasodilation edema Deficiencies in glycosylphosphatidylinositol (GPI) anchors 1. DAF, CD59 and HRF are attached to cell membrane by GPI anchors 2. DAF – decay of C3 convertases blocks amplication of alternative and classical pathways 3. CD59, HRF – block formation of MAC 4. GPI deficiency DAF, CD59, HRF not anchored cells susceptible to lysis by complement 5. paroxysmal nocturnal hemoglobulinuria (PNH) 6. only affects RBCs hemolytic anemia C3 protein deficiency 1. severe recurrent pyogenic infections 2. C3 required for: a. C3b – opsonization b. Immune complex elimination c. Formation of C5 convertases Terminal pathway protein deficiencies 1. MAC is required for elimination of Neisseria species 2. MAC not formed recurrent meningococcal and gonococcal Neisserial infections Xenotransplantation: Complement is Deleterious 1. hyperacute rejection – minutes to hours after graft transplantation a. humans have IgM antibodies that react with 1,3 galactosyl linkage of porcine carbs on endothelial lining of graft blood vessels b. immune complex formation c. classical pathway activated d. destruction of endothelial cells lining graft blood vessels e. graft thrombosis 2. How does damage to the endothelial cells occur? a. anaphylatoxins (C3a, C4a, C5a) made b. anaphylatoxins bind to receptors on mast cells and basophils c. degranulation and histamine release d. histamine increases vascular permeability e. C5a is chemotactic for phagocytes. It also activates phagocytes f. Phagocytes try to eat immune complexes and release inflammatory mediators that damage the endothelial cells g. Cell damage activates intrinsic coagulation pathway, thrombosis and activation of kallikrein bradykinin h. MAC formation on porcine endothelial cells i. Osmotic lysis. Activated macs fibroleukin or fgl2 fibrin deposition and thrombosis

![Major Change to a Course or Pathway [DOCX 31.06KB]](http://s3.studylib.net/store/data/006879957_1-7d46b1f6b93d0bf5c854352080131369-300x300.png)