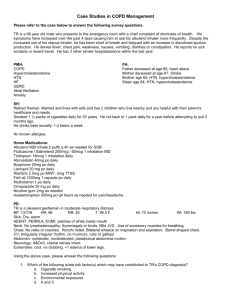
COPD Management: Maintenance
advertisement
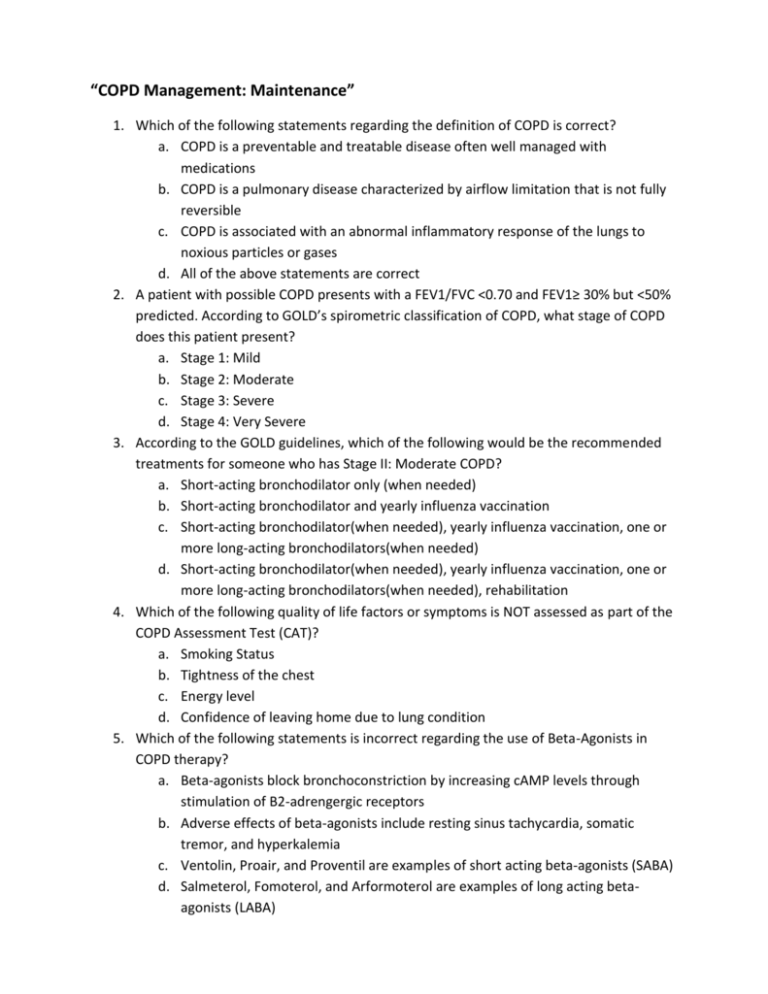
“COPD Management: Maintenance” 1. Which of the following statements regarding the definition of COPD is correct? a. COPD is a preventable and treatable disease often well managed with medications b. COPD is a pulmonary disease characterized by airflow limitation that is not fully reversible c. COPD is associated with an abnormal inflammatory response of the lungs to noxious particles or gases d. All of the above statements are correct 2. A patient with possible COPD presents with a FEV1/FVC <0.70 and FEV1≥ 30% but <50% predicted. According to GOLD’s spirometric classification of COPD, what stage of COPD does this patient present? a. Stage 1: Mild b. Stage 2: Moderate c. Stage 3: Severe d. Stage 4: Very Severe 3. According to the GOLD guidelines, which of the following would be the recommended treatments for someone who has Stage II: Moderate COPD? a. Short-acting bronchodilator only (when needed) b. Short-acting bronchodilator and yearly influenza vaccination c. Short-acting bronchodilator(when needed), yearly influenza vaccination, one or more long-acting bronchodilators(when needed) d. Short-acting bronchodilator(when needed), yearly influenza vaccination, one or more long-acting bronchodilators(when needed), rehabilitation 4. Which of the following quality of life factors or symptoms is NOT assessed as part of the COPD Assessment Test (CAT)? a. Smoking Status b. Tightness of the chest c. Energy level d. Confidence of leaving home due to lung condition 5. Which of the following statements is incorrect regarding the use of Beta-Agonists in COPD therapy? a. Beta-agonists block bronchoconstriction by increasing cAMP levels through stimulation of B2-adrengergic receptors b. Adverse effects of beta-agonists include resting sinus tachycardia, somatic tremor, and hyperkalemia c. Ventolin, Proair, and Proventil are examples of short acting beta-agonists (SABA) d. Salmeterol, Fomoterol, and Arformoterol are examples of long acting betaagonists (LABA) 6. A patient comes into your pharmacy with a prescription for Pulmicort inhaler. Which of the following counseling points would you expect to articulate to this patient? a. “Pulmicort is an inhaled corticosteroid not to be used in conjunction with any other inhalers used for COPD” b. “Common side effects seen with Pulmicort include shortness of breath and vision changes” c. “Pulmicort is a metered-dose inhaler” d. “Oral thrush is common with Pulmicort, so it is advised that you rinse your mouth after each use” 7. Which of the following statements is incorrect regarding other infrequently used COPD treatments? a. Mucolytics have been shown to improve chest discomfort, airflow limitations, and dyspnea in patients with chronic bronchitis b. Oral steroids are reserved for exacerbation treatments due to significant side effects associated with long-term use c. Side effects of methylxanthines such as theophylline include arrhythmias and insomnia d. Certain antibiotics used for chronic COPD treatment have shown some antiinflammatory effects 8. A patient experiencing refractory COPD disease is a candidate for: a. Triple therapy: tiotropium, salmeterol, fluticasone b. An assessment of inhaler technique to ensure maximum benefit of their medications c. Attend pulmonary rehab d. All of the above 9. Which of the following counseling points regarding initiation of oxygen therapy is NOT accurate? a. Air travel is safe for patients with oxygen therapy and patients should ideally be able to maintain an in flight PaO2 of at least 50mmHg b. Patients with oxygen therapy have generally seen improvements in physical activity, sleep quality and mental function c. Patients often become addicted to oxygen over time d. Patients who use oxygen both at night and during the day reduce the risk of death by ½ compared to patients who use oxygen only at night 10. Which of the following medications may result in significant weight loss in patients with COPD? a. Levalbuterol (Xopenex) b. Roflumilast (Daliresp) c. Prednisolone (Orapred) d. Tiotropium (Spiriva)