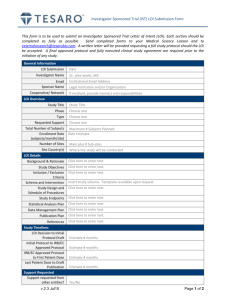
PHASE I, II, or I/II LETTER OF INTENT Submission Form v2.0
advertisement

PHASE I, II, or I/II LETTER OF INTENT Submission Form v2.0 National Cancer Institute Division of Cancer Treatment and Diagnosis Cancer Therapy Evaluation Program To complete the form electronically, use the mouse pointer or the Tab key to navigate. Select and enter text for each text field. To easily see text fields, go to Tools|Options from Word’s menu, click the View tab, and in the Show block select ‘Always’ from the Field Shading drop down list. Lead Group/Institution: Southeast East Phase 2 Consortium Emory University, Winship Cancer Institute Lead Institution/Group CTEP ID:1 Other Institutions/Groups on study: H Lee Moffitt Cancer Center /FL065 Emory University Winship Cancer Institute Vanderbilt-Ingram University University of North Carolina Virginia Commonwealth University Title of LOI: Agent(s) supplied by NCI:1 Commercial Agents in Study: A Phase I Study of ABT-263 in Combination with Topotecan ABT-263 Topotecan Tumor Type: [X] Solid Tumor (Click within the [[ ]] [[ ]] Hematologic Malignancy (NOS) and type ‘x’ to indicate the tumor [[ ]] Disease-Specific type) Disease-Specific:1 1. Small Cell Lung Cancer 10041071 (Specify the Name 2. Ovarian Cancer, NOS 10033272 and Code of the Study Disease) Performance Status: Abnormal Organ Function Permitted? Prior Therapy: Phase of Study: Treatment Plan: 1 ECOG 0-2 No Prior Therapy Allowed I Primary Objectives: 1. To determine the maximum tolerated dose (MTD), dose limiting toxicities (DLT), and recommended phase II doses (RP2D) of ABT-263 and topotecan in patients with Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 1 of 13 advanced solid organ malignancies. 2. To establish preliminary evidence of improved efficacy in an expanded cohort of patients with ovarian cancer treated at the P2RD Secondary Objectives: 1. To evaluate pharmacokinetics (PK) of ABT-263 and topotecan in order to identify potential drug-drug interactions and correlate PK parameters with toxicity profile and response. 2. Perform correlative analysis of the relationship between the expression of prosurvival (Bcl-2, Bcl-XL, Mcl-1 and Bcl-w), and proapoptotic (Noxa, Puma, Bim and Bad) Bcl-2 proteins and tumor response using archival diagnostic tissue. Design: Patients with advanced malignancies for which topotecan treatment is appropriate will be enrolled and treated in cohorts of three patients per dose level. Escalation of ABT-263 and topotecan will proceed in a modified Fibonacci 3+3 fashion with the requirement that dose escalation to the next level can only proceed if 0 of 3 or 1 of 6 patients experience a dose limiting toxicity (DLT). ABT-263 will be administered orally starting at 150mg daily days 1-5 as recommended in combination with cytotoxic agents. Topotecan will be administered concurrently on days 1-5 at a starting dose of 1 mg/m2/day for 5 days. We plan to evaluate six dose cohorts starting at dose level 1 with the provision to de-escalate 1 level should DLT be encountered at the starting dose level as detailed in the table below. The RP2D will be defined as the highest dose level at which < 33% of the dose cohort (0 of 3 or 1 of 6) experiences DLT after 1 cycle. Table 1 Dose Level -1 Starting Level 1 2 3 4 5 6 ABT-263 po daily, Days 1-5 150 mg 150 mg Topotecan iv daily Days 1- 5 0.75 mg/m2 1 mg/m2 150 mg 150 mg 200 mg 250 mg 300 mg 1.25 mg/m2 1.5 mg/m2 1.5 mg/m2 1.5 mg/m2 1.5 mg/m2 Patients: Based on the dose escalation scheme outlined, a maximum of 36 patients will be enrolled for the dose escalation if the MTD is the maximum planned dose and if each cohort required six patients to be treated. An expansion cohort of 15 patients will be treated at the RP2D to obtain additional safety information. In order to establish preliminary evidence of improved efficacy, this cohort will be restricted to ovarian cancer patients who are platinum refractory or who have relapsed following frontline platinum therapy. 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 2 of 13 Key inclusion criteria: 1. Histological/cytological confirmation of malignancy appropriate for treatment with a topotecan-containing regimen 2. Progression following prior standard therapy 3. ECOG PS 0, 1 or 2 4. Adequate renal, hepatic and bone marrow function (Hemoglobin > 10; WBC > 4000/mm3 or ANC > 1500/mm3; notably platelets > 150,000/mm3), renal (CrCl > 60 mL/min) and hepatic function < 1.5 x ULN 5. Archival tumor biopsy specimen (mandatory for the expansion cohort) Key exclusion criteria: 1. Prior topotecan or ABT-263 treatment 2. Untreated or symptomatic brain metastasis 3. Inability to take oral medications on a regular basis 4. Severe intercurrent illness Duration of Intervention and Evaluation: Subjects will be treated until disease progression, withdrawal of consent or intolerable adverse events. Subjects will be evaluated for disease status at screening and after every 2 cycles, or as clinically indicated. Patients suffering a DLT will be treated off-study according to standard of care for their stage of disease. Assessment and Definition of DLT: Toxicity will be assessed by NCI Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. DLT will be assessed during cycle 1 of therapy only. Response will be assessed by imaging studies after every 2 completed cycles of therapy. Rationale/Hypothesis: 1 The following will constitute DLT: Grade 4 neutropenia lasting more than 7 days; Grade 3/4 neutropenia of any duration with fever; Grade ≥3 nausea and or vomiting in spite of standard supportive therapy; Grade ≥3 non-hematologic toxicity; Inability to re-treat patient within 2 weeks of scheduled treatment due to a treatmentrelated event. Changes in laboratory parameters will be considered DLT only if deemed to be related to therapy. Topotecan is a camptothecin derivative that potently inhibits the topoisomerase I enzyme. By stabilizing the covalent enzyme-DNA intermediate, topotecan promotes persistent DNA torsional stress, resulting in DNA damage and cell death. Preclinical work showed that cell death induced by topotecan is closely related to changes in a proapoptotic Bcl-2 protein family member, Bcl2L12.1 Irinotecan, another topoisomerase inhibitor, showed synergistic interaction with ABT-737, a Bcl-2 targeted compound (figure 1 below).2 This synergy correlates with the dissociation of proapoptotic BH3 molecules and induction of Noxa, a potent negative regulator of Mcl-1. Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 3 of 13 Figure 1: ABT-737 and the topoisomerase I inhibitor irinotecan showed enhanced cytotoxicity in human colorectal cancer cell lines. Isobologram showing CI < 1 indicates synergy.2 Figure 2: ABT-737 treatment unsequestered Bim from its complex with Bcl-xL or Bcl-2 in HCT116 cells compared with control-treated cells (A). Bim displaced from its complex with Bcl-xL in HT-29 cells that lack endogenous Bcl-2 (B) while ABT-737 induce Mcl-1 expression and Bim/Mcl-1 complexes in both cell lines (A and B) and displaced Bim and Bak from their complex with Mcl1, Bcl-xL/Bcl-2 or Bcl-xL.2 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 4 of 13 Figure 3: ABT-737 plus CPT-11 induced apoptosis to a greater extent than did either drug alone in two colorectal cell lines (Fig. A-C ). Greater apoptosis induced in HCT116 versus HT-29 cells, in part because of the lower levels of endogenous Mcl-1 and higher levels of Bcl-2 in HCT116 cells (Fig. D).2 Topotecan has clinical activity and is approved for the treatment of relapsed small cell lung cancer based on comparable activity but better toxicity profile over multi-agent chemotherapy.3 It also has demonstrable efficacy and is an approved agent as salvage therapy for ovarian cancer after initial platinum therapy.4,5 Abnormalities in the Bcl-2 family of proteins have been described in SCLC and may play a key role in the refractoriness of this disease to conventional therapy.6-8 Similarly, immunohistochemical studies showed very high level of expression of Bcl-2 in high grade epithelial ovarian cancer relative to low grade lesions.9 Further, Bax and Bcl-2 expression correlate with disease free survival and chemosensitivity in ovarian cancer patients treated with frontline platinum containing regimen. It is reasonable to expect that recalibrating the balance between the pro-apoptotic and anti-apoptotic members of the Bcl-2 family (Figure 4) using agents that selectively target the antiapoptotic components will result in improved chemosensitivity and efficacy. 10-13 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 5 of 13 Figure 4: Bcl-2 protein family and regulation of cancer cell survival A previous attempt to target the Bcl-2 protein using antisense oligonucleotide technology was not effective probably due to incomplete abrogation of Bcl-2 mRNA translation as measured in peripheral mononuclear cells.14 Equally important for cytotoxicity induced by BH3-mimetic inhibitors is the need to abrogate the prosurvival action of Mcl-1, a Bcl-2 family member that is under stronger regulatory control of Noxa than of any other BH3-molecules. The ability of a topoisomerase I inhibitor, irinotecan, to induce the expression of Noxa provides a strong rationale to combine topoisomerase I inhibitors with agents targeting the Bcl-2 protein family. ABT-737 and ABT-263 represent 1st and 2nd generation compounds, respectively, that target the BH-3 pocket of the Bcl-2 family protein members. Both have single agent activity in solid tumors such as SCLC.15,16 ABT-263 has improved pharmacological properties over ABT-737 making it better suited for clinical development. It is an orally available agent with high nanomolar affinity for the BH-3 region of the pro-survival Bcl-2 family members including Bcl-XL, Bcl-w and Bcl-2. In in vivo experiments, ABT-263 completely suppressed Bcl-2 expression in xenograft tumor tissue at 100mg/kg dose with associated tumor regression including complete regression. This dose was 3-fold less than the tolerable dose tested in mice.16 Preclinical work showed considerable synergy when ABT-737 was combined with topoisomerase inhibitors such as etoposide and irinotecan leading to increased apoptosis2,15 and greater tumor volume reduction in vivo.15 In addition, ABT-737 and ABT-263 both displayed potent in vivo activity against xenograft derived from paclitaxel-resistant breast cancer and SCLC cell lines irrespective of the level of expression of pgp-1 efflux pump expression.16,17 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 6 of 13 Figure 5: Irinotecan markedly induced Noxa expression in HCT116 (wild-type p53) but not HT-29 (mutated p53) cells with associated up-regulation of Bax compared with vehicle-only treated cells (A). Irinotecan treatment enhance the interaction between Mcl-1 and Noxa (B) leading the release of Bak from its interaction with Mcl-1 (B). Based on the foregoing preclinical and clinical data, we propose to conduct a phase I evaluation of the combination of ABT-263 and topotecan in patients with advanced solid malignancies. We hypothesize that this combination will be well tolerated without any exacerbation of the well-characterized and manageable toxicities associated with topotecan. This combination will result in improved therapeutic efficacy in appropriately selected patient populations such as those with relapsed ovarian cancer and SCLC. We hypothesize that: I. The addition of ABT-263 will enhance the anti-cancer effects of topotecan in patients with solid malignancies. II. Pretreatment tumor expression of proapoptotic and antiapoptotic members of 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 7 of 13 the Bcl-2 family of proteins (Bcl-2, Bcl-XL, Bim and Bcl-w) in archival diagnostic biopsy specimens will correlate with response rate. Laboratory Correlates: PK Analysis: Blood will be drawn at the following time points for PK analysis of ABT-263 and topotecan: Cycle 1, day 1: 30 min before ABT-263 ingestion, and prior to topotecan infusion; then at 15 minutes, 45 minutes, 2, 3, 4, 6, 8, and 24 h post drug administration. We anticipate that ABT-263 PK analysis will be performed through a CTEP-designated central laboratory. We plan to have all PK samples analyzed at such facility using a validated standard operating procedure for PK sample collection, handling, storage and shipping as currently obtained with other multicenter trials at our center (please see appendix A). In the event that no lab is designated by CTEP for ABT-263, we plan to work with the sponsor to develop the appropriate analytical method for the PK samples. The analytical method for topotecan PK has been published previously and will be performed at Emory.18 Pharmacodynamic Correlates: 1. BCL-2 pathway proteins expression by immunohistochemistry (IHC): We plan to use the available expertise within the Winship Cancer Institute Pathology Core facility to produce the IHC stained slides. Evaluation of the slides and scoring for level of expression of the proteins of interest will be performed with our collaborator in the department of pathology, Dr. Anthony Gal. Funding for the proposed correlative studies will come from an unrestricted research grant to the PI (Taofeek Owonikoko, MD, PhD) through the Georgia Cancer Coalition Distinguished Clinician Scientist Award program. This award is worth $ 50,000 per year over 5 years. Funding for pharmacokinetic evaluations up to $50,000.00 will be made available from the research budget of the Emory Winship phase I clinical trial program (R. Donald Harvey, PharmD). Endpoints/Statistical Considerations: The frequency of all toxicities will be tabulated by grade for each dose cohort. Descriptive statistics and graphic displays will be presented to characterize each dose cohort in terms of disease features and for the PK and PD correlative endpoints. Mean expression level of Bcl-2 pathway proteins will be assessed by semiquantitative immunoscore in archival tissue. Correlation between immunoscore the administered dose of ABT-263 and tumor response will be evaluated using Spearman correlation coefficients and exact Chi-square tests. Due to the limited sample size and the phase I clinical trial design, the results of these analysis will be deemed exploratory at this time. The expansion cohort: Based on contemporary phase III evaluation of topotecan in ovarian cancer patients previously treated with a platinum agent or a taxane, topotecan achieved a 27% objective response rate.19 Assuming a doubling of the response rate to 54% when topotecan is combined with ABT-263, 15 patients treated at the RP2D will have 70% power to detect a 100% improvement in response rate at a one-sided alpha error rate 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 8 of 13 of 0.05. Such a sample size will have 85% of truly calling an effective regimen and a 5% chance of accepting an ineffective regimen. Estimated Monthly Accrual: 2-3 per month Proposed Sample Size: Minimum: 18 Maximum: 45 In the year ending December 31st 2008, a total of 159 patients were enrolled on phase I clinical trials at the Winship Cancer Institute. This represents a 53% increase in our enrolment over 2007. Of these patients, 45 were enrolled in broad, nondisease specific phase I clinical trials. We currently have 4 open phase I studies at Emory University for patients with solid organ malignancies, of which 2 would be completed by the time this study is ready for activation. The abundance of patients referred to our phase I program and the long waiting list of patients available for phase I studies will allow for timely and rapid accrual to multiple studies at any given time. The Winship Cancer Institute has an active gynecology oncology clinic, staffed by three full time medical oncologists with a large patient referral base. There is currently no active clinical trials for patient with platinum refractory ovarian cancer at our center. One of the physicians from the gynecology oncology team, Dr. Joan Cain is a coinvestigator on this application. We therefore anticipate that accrual to the expansion phase of the study will proceed quickly. Earliest date the study can begin: Projected Accrual Dates: (Month/Year format) 12/01/2009 Start: 01/ 01/ 2010 End: 12/31/2012 To document accrual rate, list trials with patients who had similar Tumor Type/Phase of Study/Prior Therapy: If more than one trial is similar, copy and paste the row below to the end of the form, then add the additional study information. Protocol Number / Title / Sponsor : X05226 / Phase IB Dose Escalation Study of Bortezomib (VELCADE) Administered Weekly for 4 Weeks and Sunitinib (SU-011248) Administered Daily for 4 Weeks Followed by a 14 Day Rest in Patients with Refractory Solid Tumors / Institutional-IIT / March 2008 - September 2009/ 33 patients; trial based on adaptive design and we are currently testing the last dose cohort Trial Activation / Trial Completion Dates: No. of Patients Enrolled:* NCI 8063/ A Phase 1 and Pharmacokinetic Single Agent Study of Pazopanib in Patients with Advanced Malignancies and Varying Degrees of Liver Dysfunction/ October 2008 – September 2009/ 2 NCI7967/ A Phase I Study of ABT-888 in Combination with Carboplatin and Paclitaxel in Advanced Solid Malignancies/ March 2008 – September 2009/ 9 NCI8057 / Phase I and Pharmacokinetic Study of Vorinostat for Solid Tumors and Lymphomas in Patients with Varying Degrees of Hepatic Dysfunction / 5 List all Active, If more than one trial is similar, copy and paste the row below to the end of the form, then add the additional study Approved, or In Review information. 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 9 of 13 studies at your institution for which this patient population will be eligible: Protocol Number / [Click and enter Number] / [Click and enter Title] / [Click and enter Sponsor] Title / Sponsor: (Include NCI Number if NCI-sponsored) [Click and enter Activation Date] / [Click and enter Anticipated Completion Date] Trial Activation Date / Anticipated Completion [Click and enter Patients Enrolled] / Date: [Click and enter enrollment start date] to [Click and enter enrollment end date] / No. of Patients [Click and enter the number of months of enrollment] / [Click and enter Planned Enrollment] Enrolled to Date / (*Only include patients enrolled at site(s) relevant to LOI proposal) Patient Enrollment Period / Duration of Patient Enrollment / Total planned Patient Enrollment:* Is this LOI part of an NIH Grant, Cooperative Agreement or Contract? Y If yes, provide the [Click and enter Award Number] Award Number: Will this study receive support from non-NCI sources (i.e., industry, ACS)? If the proposed trial includes correlative studies, CTEP assumes funding is available to support them. If yes, is it Grant funding? If yes, provide the Grant Number: Is this a Career Development LOI? If yes, please attach and check off the following: N YES Y Account 6-39419, GCC Distinguished Cancer Clinician Y Further information and instructions regarding the submission of a Career Development LOI may be found at http://ctep.cancer.gov/protocolDevelopment/letter_of_intent.htm#instructions PI curriculum vitae [X] Institutional letter of commitment [X] Mentor letter of commitment [X] The Investigational Drug Steering Committee (IDSC) is designed to provide NCI with broad external scientific and clinical input for the design and prioritization of phase I and phase II trials with agents for which CTEP holds an IND. Membership of the IDSC includes the Principal Investigators of phase I U01 grants and phase II N01 contracts, representatives from the NCI Cooperative Groups, NCI staff members, and additional representatives with expertise in biostatistics, correlative science technologies, radiation oncology, etc., as well as patient advocates and community oncologists, as needed. Experts with specific expertise will be included as ad hoc members for consideration of specific agents. The current membership list may be found at http://ccct.nci.nih.gov/steering-committees/idsc Periodically the IDSC will assess LOIs from a strategic perspective to determine whether the Clinical Development Plan for an agent should be modified. When requested by CTEP, the IDSC will provide input on LOIs to assist in CTEP decision-making. Information in an LOI assessed by IDSC is kept confidential and members with potential conflict of interest are recused from participating in the LOI assessment. The IDSC strategic assessment is not part of the CTEP LOI review process and will not affect LOI review timelines. For unsolicited LOIs only: Please check one of the following options (Note: While selecting an option is required, neither choice will affect 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 10 of 13 the outcome of the CTEP review of this LOI): This LOI may /may not Principal Investigator (PI) Name: be looked at by the IDSC. Taofeek K. Owonikoko, MD, PhD PI Signature: PI Street Address: Date: 1/13/09 Room C4094 1365C Clifton Road, NE Atlanta, GA 30322 PI Phone: 404-778-5575 PI Fax: 404-778-5230 PI E-mail: Group Chair/Cooperative Agreement-PI (GCCA-PI) Name: towonik@emory.edu Dan Sullivan, MD GCCA-PI Signature: GCCA-PI Address: Date: [Click and enter Room/Suite/Dept.] [Click and enter Street Adress] [Click and enter City, State, Postal Code] GCCA-PI Phone: [Click and enter Phone No.] GCCA-PI Fax: [Click and enter Fax No.] GCCA-PI E-mail: Dan.Sullivan@moffitt.org Non Group Grant-PI [Click and enter Name] Name: Non Group Grant-PI Signature: Date: Non Group Grant-PI [Click and enter Room/Suite/Dept.] Address: [Click and enter Street Adress] [Click and enter City, State, Postal Code] Non Group Grant-PI [Click and enter Phone No.] Phone: Non Group Grant-PI [Click and enter Fax No.] Fax: Non Group Grant-PI [Click and enter E-mail Address] E-mail: 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 11 of 13 Please submit Letter of Intent forms (LOIs) to the Protocol and Information Office (PIO) via e-mail at: pio@ctep.nci.nih.gov, Attention: LOI Coordinator Notes: LOIs from Cooperative Group must be submitted through the Group Operations. Proposals for trials to be conducted under a Cooperative Agreement must include complete contact information for the Principal Investigator and Protocol Chair. Questions? Please call LOI Coordinator at (301) 496-1367. 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 12 of 13 Reference: 1. Floros KV, Talieri M, Scorilas A: Topotecan and methotrexate alter expression of the apoptosis-related genes BCL2, FAS and BCL2L12 in leukemic HL-60 cells. Biological Chemistry 387:1629-1633, 2006 2. Okumura K, Huang S, Sinicrope FA: Induction of Noxa sensitizes human colorectal cancer cells expressing Mcl-1 to the small-molecule Bcl-2/Bcl-xL inhibitor, ABT-737. Clin Cancer Res 14:8132-42, 2008 3. von Pawel J, Schiller JH, Shepherd FA, et al: Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol 17:65867, 1999 4. Eckardt JR: Emerging role of weekly topotecan in recurrent small cell lung cancer. Oncologist 9 Suppl 6:25-32, 2004 5. Vandenput I, Amant F, Neven P, et al: Effectiveness of weekly topotecan in patients with recurrent epithelial ovarian cancer. Int J Gynecol Cancer 17:83-7, 2007 6. Ben-Ezra JM, Kornstein MJ, Grimes MM, et al: Small cell carcinomas of the lung express the Bcl-2 protein. Am J Pathol 145:1036-40, 1994 7. Kim YH, Girard L, Giacomini CP, et al: Combined microarray analysis of small cell lung cancer reveals altered apoptotic balance and distinct expression signatures of MYC family gene amplification. Oncogene 25:130-8, 2006 8. Olejniczak ET, Van Sant C, Anderson MG, et al: Integrative genomic analysis of smallcell lung carcinoma reveals correlates of sensitivity to bcl-2 antagonists and uncovers novel chromosomal gains. Mol Cancer Res 5:331-9, 2007 9. O'Neill CJ, Deavers MT, Malpica A, et al: An immunohistochemical comparison between low-grade and high-grade ovarian serous carcinomas: significantly higher expression of p53, MIB1, BCL2, HER-2/neu, and C-KIT in high-grade neoplasms. Am J Surg Pathol 29:1034-41, 2005 10. Certo M, Del Gaizo Moore V, Nishino M, et al: Mitochondria primed by death signals determine cellular addiction to antiapoptotic BCL-2 family members. Cancer Cell 9:351-65, 2006 11. Kim H, Rafiuddin-Shah M, Tu HC, et al: Hierarchical regulation of mitochondriondependent apoptosis by BCL-2 subfamilies. Nat Cell Biol 8:1348-58, 2006 12. Chen L, Willis SN, Wei A, et al: Differential targeting of prosurvival Bcl-2 proteins by their BH3-only ligands allows complementary apoptotic function. Mol Cell 17:393-403, 2005 13. Willis SN, Fletcher JI, Kaufmann T, et al: Apoptosis initiated when BH3 ligands engage multiple Bcl-2 homologs, not Bax or Bak. Science 315:856-9, 2007 14. Rudin CM, Kozloff M, Hoffman PC, et al: Phase I study of G3139, a bcl-2 antisense oligonucleotide, combined with carboplatin and etoposide in patients with small-cell lung cancer. J Clin Oncol 22:1110-7, 2004 15. Hann CL, Daniel VC, Sugar EA, et al: Therapeutic efficacy of ABT-737, a selective inhibitor of BCL-2, in small cell lung cancer. Cancer Res 68:2321-8, 2008 16. Shoemaker AR, Mitten MJ, Adickes J, et al: Activity of the Bcl-2 family inhibitor ABT-263 in a panel of small cell lung cancer xenograft models. Clin Cancer Res 14:3268-77, 2008 17. Kutuk O, Letai A: Regulation of Bcl-2 family proteins by posttranslational modifications. Curr Mol Med 8:102-18, 2008 18. Bai F, Kirstein MN, Hanna SK, et al: Determination of plasma topotecan and its metabolite N-desmethyl topotecan as both lactone and total form by reversed-phase liquid chromatography with fluorescence detection. J Chromatogr B Analyt Technol Biomed Life Sci 784:225-32, 2003 19. Meier W, du Bois A, Reuss A, et al: Topotecan versus treosulfan, an alkylating agent, in patients with epithelial ovarian cancer and relapse within 12 months following 1st-line platinum/paclitaxel chemotherapy. A prospectively randomized phase III trial by the 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 13 of 13 Arbeitsgemeinschaft Gynaekologische Onkologie Ovarian Cancer Study Group (AGO-OVAR). Gynecol Oncol 114:199-205, 2009 1 Detailed Institution, Group, Agent NSC, and Disease codes are available on the CTEP Home Page at http://ctep.cancer.gov/protocolDevelopment/codes_values.htm 31-LOI Submission Form Revised 12/01/2008 Page 14 of 13