June 2009 - Conference of Allegheny Providers
advertisement
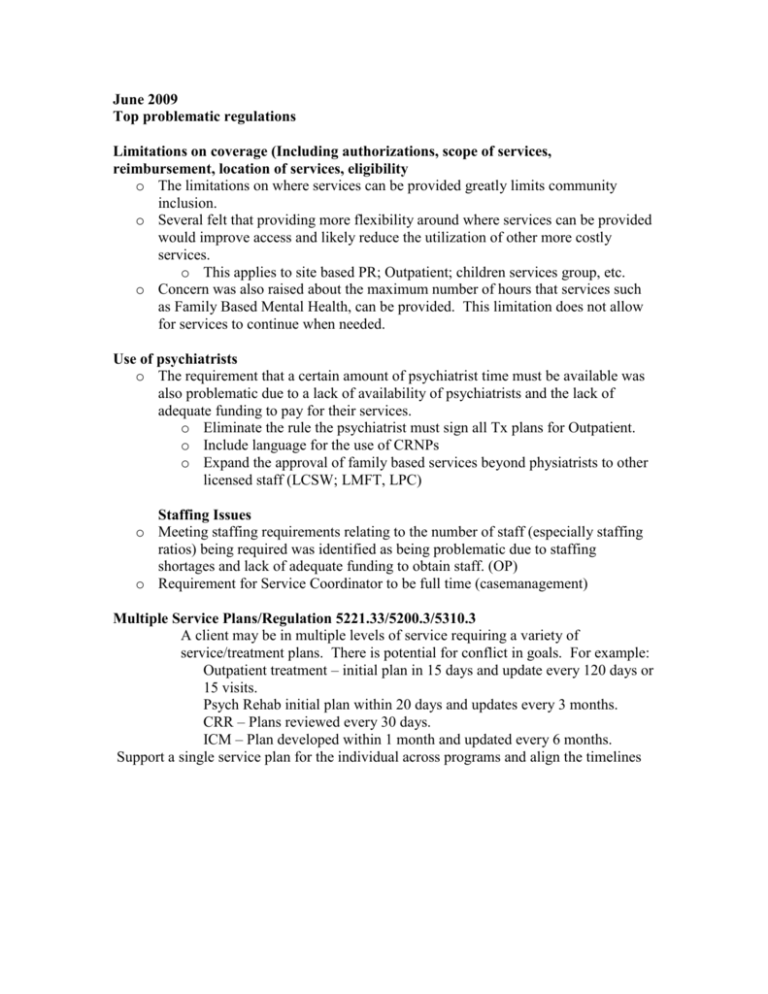
June 2009 Top problematic regulations Limitations on coverage (Including authorizations, scope of services, reimbursement, location of services, eligibility o The limitations on where services can be provided greatly limits community inclusion. o Several felt that providing more flexibility around where services can be provided would improve access and likely reduce the utilization of other more costly services. o This applies to site based PR; Outpatient; children services group, etc. o Concern was also raised about the maximum number of hours that services such as Family Based Mental Health, can be provided. This limitation does not allow for services to continue when needed. Use of psychiatrists o The requirement that a certain amount of psychiatrist time must be available was also problematic due to a lack of availability of psychiatrists and the lack of adequate funding to pay for their services. o Eliminate the rule the psychiatrist must sign all Tx plans for Outpatient. o Include language for the use of CRNPs o Expand the approval of family based services beyond physiatrists to other licensed staff (LCSW; LMFT, LPC) Staffing Issues o Meeting staffing requirements relating to the number of staff (especially staffing ratios) being required was identified as being problematic due to staffing shortages and lack of adequate funding to obtain staff. (OP) o Requirement for Service Coordinator to be full time (casemanagement) Multiple Service Plans/Regulation 5221.33/5200.3/5310.3 A client may be in multiple levels of service requiring a variety of service/treatment plans. There is potential for conflict in goals. For example: Outpatient treatment – initial plan in 15 days and update every 120 days or 15 visits. Psych Rehab initial plan within 20 days and updates every 3 months. CRR – Plans reviewed every 30 days. ICM – Plan developed within 1 month and updated every 6 months. Support a single service plan for the individual across programs and align the timelines § 1153.2. Definitions. Group psychotherapy—Psychotherapy provided to no less than two and no more than ten persons with diagnosed mental disorders for a period of at least 1 hour. These sessions shall be conducted by a clinical staff person. Some folks ca not tolerate 1 hour group The requirement for 10 or less than ten persons does not allow for over booking to account for no shows, etc. Mobile Psych Rehab: Travel time is not included as part of the service. Although the rate is modestly inflated, it does not cover travel costs. No part of a broken appointment is reimbursable. When a consumer does not cancel appointment, but is not home or otherwise misses the appointment, the counselor cannot bill for any time. Reimbursement for Hearing Impaired Services: eimbursement does not come close to covering the costs which are, on average, $65 per hour for the interpreter and with a minimum requirement for two hours. PHP 3 hour minimum requirements: Inconsistent with Medicare regs. Athough D&A regulations are a DOH issue, the conflict with BH regulations and ideology create: Extra provider costs; Unnecessary redundancy Barriers for collaboration between providers Undue risks to clients as a result of care fragmentation. Support quick turnaround for demonstration project waivers to encourage creativity and calculated risk for new service delivery model