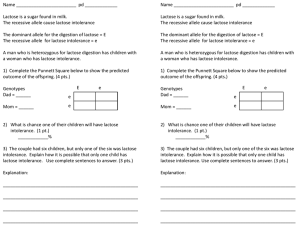
Lactose Intolerance
advertisement

Lactose Intolerance Emily Schwichtenberg 1 Lactose Intolerance: The Difference in Lactose Digestion and Symptoms. Emily Schwichtenberg Advanced Nutrition 361 Abstract Lactose Intolerance Emily Schwichtenberg 2 Lactose Intolerance is the inability to breakdown the disaccharide lactose. It usually occurs when the enzyme lactase is produced in low amounts or not at all. When milk is ingested the main disaccharide, lactose, is broken down into glucose and galactose by the enzyme lactase in the duodenum. If the enzyme is lacking in a persons body lactose cannot be broken down and this person is considered lactose sensitive. The lactose can only sit in the intestine and take in water to dilute it enough until it can pass. This causes much discomfort especially in the abdominal area and can cause diarrhea and gas. Milk is a vital daily dietary need; it provides most of the calcium and vitamin D used in our bodies. Most lactose intolerant people can tolerate a small amount of milk and should try to drink as much as possible before symptoms occur. There are also other conditions in our body that would cause similar symptoms such as; irritable bowel syndrome, lactose malabsorption, and milk allergy. When these conditions are experienced one should not limit milk intake. Calcium deficiencies are very prevalent and should be avoided at all costs to reduce future problems with health. Emily Schwichtenberg Lactose Intolerance Emily Schwichtenberg 3 Advanced Nutrition Ellen Lutgen Johnson 10 October 2007 Lactose Intolerance: The Difference in Lactose Digestion and Symptoms. Experiencing stomach cramps, gas and overall discomfort after eating a meal is not unusual. However, the cause may not be the same with each person. It is easy to blame one food group or another and then remove it completely from ones diet. However, doing this may remove essential vitamins or minerals out of ones body, such as, calcium. When milk is ingested the main disaccharide, lactose, is broken down into glucose and galactose by the enzyme lactase in the duodenum. If the enzyme is lacking in a persons body lactose cannot be broken down and this person is considered lactose sensitive. The lactose can only sit in the intestine and take in water to dilute it enough until it can pass. Because there is so much water attained it will pass as diarrhea not as solid feces causing discomfort for the individual experiencing this process. Explained by Dennis A. Savaiano, a professor in the department of food science and nutrition at the University of Minnesota and Michael D. Levitt from the Veterans administration medical center in Minneapolis, Minnesota: Lactose-deficient persons cannot digest significant quantities of lactose due to enzyme insufficiency. Because the disaccharide lactose is not absorbed, the result of this maldigestion is malabsorption, a lack of blood Lactose Intolerance Emily Schwichtenberg 4 glucose elevation, and the transit of lactose to the large intestine where it is available for fermentation by the microflora (Savaiano p. 397). Many people suffer from symptoms associated with lactose intolerance such as: gas, diarrhea, distension, abdominal cramping, and bloating. Although symptoms may be similar there are differences in bowel disorders most often confused with lactose intolerance. Discussed will be the difference between Irritable bowel syndrome, malabsorption of lactose, lactose intolerance and milk allergy. Treatments of these symptoms can be easy, such as limiting milk intake where as other options involve taking medication before milk is ingested. Not every person that experiences symptoms may have any sensitivity to lactose. There are many misdiagnoses when one diagnosis oneself. This can cause a person to restrict milk and the intake of calcium when it is not necessary and could cause more dire problems in the future. Lactose intolerance is a condition that one either has or does not have; it is not a “sometimes” occurrence. Many people mistake other conditions for Lactose intolerance such as, Irritable bowel syndrome. Irritable bowel syndrome, or IBS, is an ailment that anyone can experience after eating a meal. This “syndrome affects 5% to 20% of the Western population,” (lactose intolerance in IBS patients p. 7). It is comprised of any combination of common disturbances of the bowel such as diarrhea or constipation, along with abdominal pain. This can be caused by emotional or physiological stress, and nonspecific food consumption. “While symptoms such as diarrhea, bloating and flatulence can occur as a result of lactose maldigestion, they are not specific to lactose maldigestion and may also be experienced after ingestion of other foods” (self-reported LI pg. 52). As stated by Heather Lovelace and Susan Barr in their research journal based on self- Lactose Intolerance Emily Schwichtenberg 5 reported lactose intolerance we can safely say that irritable bowel syndrome is not directly linked to lactose digestion. It would be best to eat foods that are easily digestible by the stomach such as soups, breads and grains. It is not necessary to reduce the intake of any food groups while experiencing irritable bowel syndrome. The most commonly mistaken condition is malabsorption; it is also the most closely related. Malabsorption is faulty or inadequate absorption of nutrients by the intestinal tract where as intolerance is the inability to produce the enzyme to help break down the nutrient lactose. In this case the enzyme is lactase and the disaccharide is lactose. Malabsorption occurs when “…glucose in blood does not rise at least 20mg/dl…” (Savaiano et al p. 398). “This is tested either by the lack of rise in blood glucose or the elevation of alveolar hydrogen” (Savaiano et al p.398). This is tested using a breathing test after lactose ingestion. Those individuals that are classified as lactose intolerant will not have blood glucose above 20mg/dl and they will experience one or more of the symptoms previously mentioned. Although this is a slight difference many people that have self diagnosed lactose intolerance are more than likely just malabsorbers. In the study done by Carroccio, Montalto, Cavera, Notarbatolo and the Lactase Deficiency Study Group looking at the difference between lactose intolerance and malabsorption: They took 323 volunteers that fit the demographic of the region and subjected them to the hydrogen breathing test after an overnight fast and then 25 grams, or less depending on weight, of lactose suspended 250 to 300 milliliters of water. The breaths were taken every thirty minutes for three hours. Based on the data collected from this procedure the scientists Lactose Intolerance Emily Schwichtenberg 6 concluded that of the 323: 104/323 subjects (32.2%) as lactose maldigesters but tolerant, 13/323 subjects (4%) as maldigesters and intolerants, 3/323 subjects (1%) as digesters but intolerants and 203/323 subjects as digesters and tolerant (Carroccio et al. p 632-633). These two deficiencies lack the ability to utilize the disaccharide lactose in the body. With intolerance, lactose cannot be broken down and the body cannot use this for an energy source. Malabsorption is able to break down the disaccharide it is not actively absorbed into the blood stream to be used as energy. The most severe symptoms experienced are by those with a milk allergy. An allergy is a reaction one receives when they are hypersensitive to the allergen. In this case it is milk, more specifically usually the proteins in milk. Along with the symptoms discussed earlier milk allergies can also cause the individual to produce hives, experience wheezing and trouble breathing, vomit or form a rash. This allergic reaction happens when: [Milk] proteins are broken down, [and] macromolecules are formed. These high-molecular weight food proteins are then absorbed via the intestinal mucosa. This results in the development of antibodies against cow’s milk protein and is thought to be a normal physiological response. (Wilson p. 204). This process is a predisposition to digestion problems of milk throughout ones life. Milk allergies can usually be identified in infants. This allows doctors to come up with appropriate treatments to allow the patient adequate intake of calcium to promote future bone health. Lactose Intolerance Emily Schwichtenberg 7 If one is not lactose intolerant or allergic there are some simple recommendations to continue milk and calcium intake along with lowering some symptoms. A small brochure was put out by the National Dairy Council addressing this issue along with providing general information about lactose intolerance. The first suggestion is not to eliminate milk completely; start with small doses of milk “try small portions of milk and milk products. This allows whatever lactase is there to do its job of digesting the lactose before it starts causing problems.” Work milk and calcium into the diet “Start with a smaller portion and slowly increase the serving size of the dairy foods you eat. When you notice symptoms that may signal your limit for the amount of lactose you can handle at one sitting.” Take dairy products with other foods. This will help slow the emptying of the duodenum and may decrease symptoms. “Older is wiser” aged cheeses have most of the lactose removed during processing. “Aged hard cheeses, such as cheddar, Colby, Swiss and parmesan, are particularly low in lactose… Look for cultured milk products such as yogurt with live, active cultures, which contain ‘friendly’ bacteria that help digest lactose.” Reduce the intake of high lactose milk, “look for lactose-free milk in the dairy case. It has all the nutrients of regular milk.” If necessary, there are pills that one can take. It is a lactase enzyme pill that when taken with the first bite or drink of a dairy food will help ones body digest lactose. Taking these small steps may lower the lactose intake just enough that one will no longer experience symptoms. A common problem related to lactose intolerance is the decrease in calcium intake potentially to a level of inadequacy. There are supplements that can help with this such as calcium chew-ables and other over the counter pills. Other options recommended by the “2005 dietary guidelines… [are] milk alternatives within the milk food group, such as Lactose Intolerance Emily Schwichtenberg 8 yogurt and lactose-free milk, are the most reliable and easiest way to derive the health benefits associated with milk and milk products” (National Dairy Council). Other options would include cheese, ice cream and soy milk. It is important to consume some sort of dairy products even if one is lactose intolerant to get the essential mineral, calcium, and vitamin, vitamin D. These are vital to bone health and growth in all ages. Milk is the most commonly complained about food in our diet and it is the most common food allergen. Milk is the food that is most blamed for causing discomfort. However, only 15% of the white population and 53% among Mexican-Americans and 80% in the black population show prevalence of lactose maldigestion in America (Lactose Intolerance p. 166s). Often time’s lactose intolerance is self diagnosed and is usually incorrect. Only a physician can test for intolerance and should prescribe a dairy free diet or any supplements. This misdiagnosis can result in calcium deficiency and possible bone and health issues in the future. Lactose intolerance is not as common as many people think. This misconception causes many people to decrease their milk intake which directly effects calcium and vitamin D intake. This could affect bone health and bone strength later in life. Milk is a vital part of our diet. Most discomfort can be avoided with smaller does of milk throughout the day. This will also help with calcium absorption. Overall, only a physician can diagnose anyone with intolerance and one should not diagnose oneself. Lactose Intolerance Emily Schwichtenberg 9 References A. Carroccio, G. Montalto, G. Cavera, A. Notarbatolo, and the Lactose Deficiency Study Group. (1998). Lactose intolerance and self-reported milk intolerance: Relationship with lactose maldigestion and nutrient intake.17 (6), 631-636. Carlos Felipe Bernarders-Silva, Alexandre C. Perira, Gloria de Fatima Alves da Mota, Jose Eduardo Krieger, Antonio Atilio Laudanna. (2007). Lactase Persistence/nonpersistence variants, C/T_13910 and G/A_22018, as a diagnostic tool for lactose intolerance in IBS patients. Science Direct, 7-11. Dennis A Savaiano, Michael D. Levitt. (1987). Milk intolerance and microbe-containing dairy foods.70 (2), 397-406. Heather Y. Lovelace & Susan I. Barr. (2005). Diagnosis, symptoms and calcium intakes of individuals with self-reported lactose intolerence.24 (1), 51-57. Lactose Intolerance Emily Schwichtenberg 10 Janice Wilson. (2005). Milk intolerance: Lactose intolerance and cow's milk protein allergy. Newborn and Infant Nursing Reviews, 5(4), 203-207. National Dairy Council. (2007). The Lowdown on Lactose Intolerance: Making the Most of Milk. Tuula H Vesa, Philippe Marteau and Riitta Korpela. (2000). Lactose intolerance.19 (2), 165s-175s.

![Lac Operon AP Biology PhET Simulation[1]](http://s3.studylib.net/store/data/006805976_1-a15f6d5ce2299a278136113aece5b534-300x300.png)