Therapies for TB – Current and Future Approaches
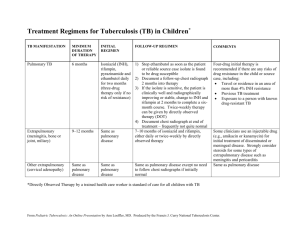
advertisement

Therapies for Childhood Tuberculosis – Current and Future Approaches Cristina Pierry, M.D. Division of Pediatric Pulmonology Clinica Alemana de Santiago Santiago, Chile cpierry@alemana.cl Tuberculosis (TB) in Children is an important cause of morbidity and mortality. Multiple therapeutic regimens for different clinical manifestations are in use. The World Health Organization (WHO) has suggested a category-based treatment that has its focus on adult type of TB (1). DOTS (directly observed therapy, short-course) has become the cornerstone for TB control across the world. There are five key elements for treatment: 1) Government commitment to sustained TB control 2) Case detection by sputum smear microscopy 3) Standardized treatment regimens for all confirmed smear-positive cases 4) Regular uninterrupted supply of essential anti-TB drugs 5) A standardized recording and reporting system DOTS has been adopted by 148 of 210 countries around the world (2). The main objectives in TB treatment are: 1) To cure the patient of TB (by rapidly eliminating most of the bacilli) 2) To prevent death from active TB or its late effects 3) To prevent relapse of TB (by eliminating the dormant bacilli) 4) To prevent development of drug resistance (by using a combination of drugs) 5) To reduce transmission of TB (1). Anti-tuberculosis drugs: TB treatment is divided into two phases: • An intensive initial multidrug phase that aims at killing of the majority of viable bacilli and preventing the emergence of drug resistance. • A continuation phase: aims at sterilization of TB lesions and prevention of relapse by eradicating the dormant organisms. Fewer drugs are generally used. The action of anti-TB drugs on these different populations may be bactericidal or sterilizing (or both). Bactericidal activity refers to the agent’s ability to rapidly kill the actively metabolizing organisms in the sputum of patients with pulmonary TB. Agents can be compared by determining their “Early bactericidal activity” (EBA), defined as the fall in viable colony-forming units (cfu) of Mycobacterium tuberculosis per ml of sputum per day during the first 2 days of treatment (3).There are five “first line” anti-TB agents that have been in use for over 30 years: Isoniazid (INH, H); Rifampicin (RMP, R); Pyrazinamide (Z); Ethambutol (EMB, E) and Streptomycin (S). Regimens: Most children are not smear-positive and do not require four drugs in the initial intensive phase; those who are smear-positive or have a visible cavity on chest radiograph have a high bacillus count and should be treated with four drugs. Also those with severe disease such as extensive lung disease, meningitis or disseminated and Spinal TB with neurological signs, are managed with four drugs in the intensive phase. There is a standard code for TB treatment regimens (4). (Table 1) Table 1. - Recommended treatment regimens for each diagnostic category based on WHO recommendations: Daily Three times a Regimen week regimen TB diagnostic TB cases Intensive Continuation category phase phase III New smear- negative PTB. Less 2HRZ 4HR or 6HE severe forms of EPTB I New smear- positive PTB 2HRZS (or 4HR or 6HE New smear-negative PTB with E) extensive parenchymal involvement Severe forms of EPTB Severe concomitant HIV disease I TB meningitis 2RHZS 7RH Disseminated TB Spinal TB II Previously treated smear-positive 2RHZS 4RH PTB IV Chronic and MDR-TB Specially Specially designed designed TB: tuberculosis; PTB: pulmonary tuberculosis; EPTB: extra-pulmonary tuberculosis; H: isoniazid; R: rifampicin; Z: pyrazinamide; E: ethambutol; S: streptomycin; HIV: human immunodeficiency virus; MDR-TB: multidrug resistant TB; The number in front of each phase represents the duration of that phase in months. Doses: The need for better data on anti-TB drug pharmacokinetics in children is highlighted by the variations in national recommendations for drug doses, particularly those related to INH. Based on several studies it appears that dosage calculations of RPM and EMB are more valid based on body surface area rather than body weight, the latter may be leading to higher doses. Most of the guidelines worldwide recommend the same doses (5). (Table 2) Table 2. - Doses of first line anti-TB drugs in children in mg/kg body weight (range) and varying regimens (1). Drug Daily regimen Three time/ week regimen Isoniazid 5 (4 – 6) max 300 mg 10 (8 – 12) Rifampicin 10 (8 – 12) max 600 mg 10 (8 – 12) Pyrazinamide 25 (20 – 30) 35 (30 – 40) Ethambutol 20 (15 – 25) 30 (25 – 35) Streptomycin 15 (12 – 18) 15 (12 – 18) • Isoniazid: remains the most important agent, because of its high EBA, outstanding pharmacokinetics and relatively low toxicity. It is rapidly absorbed and has excellent penetration into most body compartments. It is the first agent against which resistance develops. Recent pediatric studies suggest higher doses of INH per kilogram of body weight to achieve similar concentration to those in adults (6). • Rifampicin: is a key drug in chemotherapy because it rapidly kills the majority of bacilli in TB lesions and prevents relapse, it has moderate EBA. Absorption is influenced by gastric pH. Pharmacokinetic studies of higher dosages in children are urgently needed (7). • Pyrazinamide: has favorable pharmacokinetics and penetrates most tissues, including cerebrospinal fluid; serum levels are related to body weight. Resistance is uncommon but modern studies with molecular methodologies suggest that the prevalence of resistance to PZA may be higher than previously appreciated (3). • Ethambutol: Inhibits cell-wall biosynthesis and is effective against actively growing M. Tuberculosis. A review of recent publication showed that children have significantly lower peak serum concentrations than adults receiving the same dose; additionally use of higher dose of EMB does not increase ocular toxicity. The recommended dose in children is 20 mg/kg (8-9). • Streptomycin: An aminoglycoside, has the highest bactericidal activity in vitro of any anti-TB agent, though it has low EBA. Its aim is to prevent resistance to companion drugs. It can cause otovestibular damage and nephrotoxicity. • Corticosteroids: While not an anti-TB agent per se, is used in meningitis, endobronchial TB, enlarged lymph nodes that compress the tracheobronchial tree, localized emphysema, or severe pulmonary disease. It can also be used in tamponade with TB-related pericardial effusion. The most frequently used drug is prednisone, at a dose of 1 to 2 mg/kg/day for 4 to 6 weeks with gradual tapering (dose should be reduced over 1 – 2 weeks before stopping) (1). Adverse effects: Are less common than in adults. The most frequent is hepatotoxicity, which can be caused by INH, RMP or Z. An asymptomatic mild elevation of serum liver enzymes is not an indication for cessation of treatment, but hepatomegaly and jaundice should lead to discontinuation of the potentially hepatotoxic drugs. If treatment needs to be completed, non-hepatotoxic drugs should be utilized, such as: ethambutol, an aminoglycoside and a fluoroquinolone. INH may cause symptomatic pyridoxine deficiency, particularly in severely malnourished children and HIV-infected children on highly active antiretroviral therapy. Supplemental pyridoxine (5 – 10 mg/day) is recommended in such cases. Latent infection: Treatment of latent TB infection or chemoprophylaxis is important to prevent future disease activation. WHO guidelines recommend that children under 5 years of age in close contact with an infectious case receive 6 months of INH once active disease has been excluded; recent studies suggest that 3 months of combined INH and RPM is equally effective (10). Another trial recommends 4 months of RMP because of fewer adverse events (11). Second line drugs: Treatment is further complicated by the emergence of multidrug resistant TB (MDRTB) and by the infection’s synergy with HIV/AIDS. Patients with MDR-TB must be treated with a combination containing second-line drugs that are less effective, more expensive, and more toxic: • Fluorquinolones: wide-spectrum antibiotics. The most used are ciprofloxacin and ofloxacin, but new studies of levofloxacin, gatifloxacin and moxifloxacin have shown high EBA similar to INH (12). Caution should be exercised with the use of these medications since recent data suggest that they could lead to emergence of invasive pneumococcal disease (13). Recommended dose of ciprofloxacin is 30-50 mg/kg given twice a day. More studies about pharmacokinetics of the rest of fluorquinolones in children are required in order to recommend safe doses. • Thioamides: Ethionamide (ETH) and Prothionamide: two different presentations of the same active substance. The mechanism of action is similar to INH; they inhibit mycolic acid synthesis, with similar pharmacokinetics for both preparations. Recommended dose: 15 – 20 mg/kg. • Aminoglycosides: Kanamycin or Amikacin (AM): both have similar structure and low efficacy, AM is less ototoxic and preferred in children (15 – 20 mg/kg). • Terizidone/Cycloserine: Terizidone is a combination of two molecules of cycloserine. Moderately active and bacteriostatic. Side effects are associated with the central nervous system and include depression (15 – 20 mg/kg). • Capreomycin (CM) and Viomycin: macrocyclic peptide antibiotics with similar structure, administered intramuscularly. Not recommended below 14 years of age (20 mg/kg). • Para-aminosalicylic acid: Is one of the oldest anti-TB drugs. It is a weak agent, and produces severe gastrointestinal discomfort (150 mg/kg). Multidrug-resistant TB: Organisms that are resistant to both INH and RPM, with or without resistance to other anti-TB drugs. Treatment is therefore difficult, some principles are as follows: • Treat the child according to drug susceptibility testing (DST) of the source case’s strain. Do not just add a new drug to a failing regimen • Use at least four drugs that are certain to be effective • Use daily treatment only, and DOTS is essential • Follow up is important • Treatment duration for most cases will be 12 months or more. • Use second line drugs in correct dosing to avoid long-term adverse effects (1). Future Developments: For the first time in decades, there is now a promising pipeline of more than 20 compounds in various stages of development under the guidance of Global Alliance. New anti-tuberculosis drugs are being developed and several have entered preliminary clinical trials. Of these the following appear to be of particular value: • Rifapentine: recently approved and has not yet been widely used in clinical settings, inhibits bacterial DNA-dependent RNA polymerase; this is unique mechanism that is advantageous because it occurs even when enzyme exposure to drug is very brief in otherwise metabolically dormant organisms. It should be given with INH during continuation phase of treatment. Not recommended in HIV patients and in children aged < 12 years; the half-life is long, which allows once – weekly dosing. (600 mg) (14). • Diarylquinoline TMC207: Offers a new mechanism of anti-TB action by inhibiting mycobacterial ATP synthase. In vitro, potently inhibits drug-sensitive and drug-resistant M. tuberculosis isolates, it also has bactericidal effect against dormant tubercular bacilli. Safety and efficacy findings in some studies validate this treatment in patients with MDR –TB (15). • OPC-67683, A Nitro-Dihydro-Imidazooxazole derivative: Mycolic acid biosynthesis inhibitor, free of mutagenicity and posseses high activity against TB, including MDR-TB, as shown by its exceptionally low minimum inhibitory concentration in vitro and highly effective therapeutic activity at low doses in vivo (16). References: 1) World Health Organization. Guidance for national tuberculosis programmes on the management of tuberculosis in children. WHO/HTM/TB/2006.371, 10-31. 2006 2) Shingadia D, Novelli V. Diagnosis and treatment of tuberculosis in children. Lancet Infect Dis. 2003 Oct;3(10):624-32 3) Donald PR, Schaaf HS. Old and new drugs for the treatment of tuberculosis in children. Paediatr Respir Rev. 2007 Jun;8(2):134-41 4) Stop TB Partnership Childhood TB Subgroup World Health Organization. Guidance for National Tuberculosis Programmes on the management of tuberculosis in children. Chapter 2: Anti – tuberculosis treatment in children. Int J Tuberc Lung Dis. 2006 Oct;10(10):1091-7 5) Newton SM, Brent AJ, Anderson S, et al. Paediatric tuberculosis. Lancet Infect Dis. 2008 Aug;8(8):498-510 6) McIlleron H, Willemse M, Werely CJ, et al. Isoniazid plasma concentrations in a cohort of South African children with tuberculosis: implications for international pediatric dosing guidelines.Clin Infect Dis. 2009 Jun 1;48(11):1547-53. 7) Schaaf HS, Willemse M, Cilliers K, et al. Rifampin pharmacokinetics in children, with and without human immunodeficiency virus infection, hospitalized for the management of severe forms of tuberculosis. BMC Med. 2009 Apr 22; 7:19 8) Donald PR, Maher D, Maritz JS et al. Ethambutol dosage for the treatment of children: literature review and recommendations. Int J Tuberc Lung Dis. 2006 Dec;10(12):1318-30 9) Thee S, Detjen A, Quarcoo D et al. Ethambutol in paediatric tuberculosis: aspects of ethambutol serum concentration, efficacy and toxicity in children. Int J Tuberc Lung Dis. 2007 Sep;11 (9):965-71 10) Ena J, Valls V. Short-Course therapy with rifampin plus isoniazid, compared with standard therapy with isoniazid, for latent tuberculosis infection: a meta-analysis. Clin Infect Dis. 2005;40:670-6 11) Menzies D, Long R, Trajman A, et al. Adverse Events with 4 Months of rifampin therapy or 9 months of isoniazid therapy for latent tuberculosis infection: a randomized trial. Ann Intern Med. 2008 Nov 18;149(10):689-697 12) Johnson JL, Hadad DJ, Boom WH et al. Early and extended bactericidal activity of levofloxacin, gatifloxacin and moxifloxacin in pulmonary tuberculosis. Int J Tuberc Lung Dis 2006 Jun; 10(6):605-612 13) Von Gottberg A, Klugman KP, Cohen C et Al. Emergence of levofloxacin-non-susceptible Streptococcus pneumoniae and treatment for multidrug-resistant tuberculosis in children in South Africa: a cohort observational surveillance study. Lancet. 2008 Mar 29;371(9618):110813 14) Munsiff SS, Kambili C, Ahuja SD. Rifapentine for the treatment of pulmonary tuberculosis. Clin Infect Dis. 2006 Dec 1;43(11):1468-75 15) Diacon AH, Pym A, Grobusch M, et al. The Diarylquinoline TMC207 for Multidrug-Resistant Tuberculosis. The New England Journal of Medicine. 2009 Jun;360(23):2397-2405 16) Matsumoto M, Hashizume H, Tomishige T, et al. OPC-67683, a nitrodihydro-imidazooxazole derivative with promising action against tuberculosis in vitro and in mice. PloS Med 2006; 3:2131 – 2144