view web only data 58 KB

Gaber et al 1
1 MS Thorax 2008/101196 data supplement
2
3
Title:
4 Authors:
5
6
7
8
Increased levels of cysteinyl-leukotrienes in saliva, induced sputum, urine and blood from aspirin-intolerant asthmatics
Flora Gaber M Sc
1
, Kameran Daham MD
Noritaka Higashi MD, PhD
1,#
Sc
1
, Anna James PhD
1,2
MD, PhD 2
Maria Kumlin BM, PhD
1,4
2
, Ai Higashi MD
, Barbro Dahlén MD, PhD 2
1,#
,
, Agneta Gülich RN 2
, Ingrid Delin B
, Maria Skedinger MD, PhD
2
, Pär Gyllfors
, Magnus Nord MD, PhD 3 , Sven-Erik Dahlén MD, PhD 1 ,
13
14
15
16
9 Affiliations:
10
11
12
1
Unit of Experimental Asthma & Allergy Research, The National
Institute of Environmental Medicine, and
2
Division of Respiratory
Medicine and Allergy, Department of Medicine at Karolinska
University Hospital Huddinge and 3 Solna, 4 Sophiahemmet University
College, Stockholm, Sweden, all partners at Centre for Allergy
Research, Karolinska Institutet, Stockholm, Sweden.
#
Current address:
Clinical Research Center, National Sagamihara Hospital, Kanagawa,
Japan.
17 Corresponding author: Dr Barbro Dahlén, Barbro.dahlen@ki.se
; Lung and Allergy
18 Clinic, C1 88, Karolinska University Hospital, SE-141 86 Stockholm, Sweden; Tel +468
19 5858 6734; Fax +468 7117306
20
Gaber et al 2
21 METHODS
22
23 Subjects
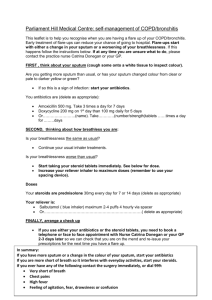
24 The study involved 21 non-smoking subjects with chronic asthma, recurrent
25 rhinosinusitis and/or nasal polyps, and a suspicion of intolerance to non-steroidal anti-
26 inflammatory drugs (NSAID) (Table I in the main text). All subjects were recruited from
27 the Lung/Allergy Clinic at Karolinska University Hospital Huddinge. All had an
28
FEV1≥70% of predicted and had a stable asthma. Subjects were excluded if they had an
29 asthma exacerbation or lower respiratory tract infection within six weeks. The study was
30 approved by the local ethics committee (Dnr 518/03) and the subjects gave written
31 informed consent.
32 Before each visit, subjects were instructed to withhold inhaled short-acting β
2
-
33 agonists for 6 hours, inhaled ipratropium for 12 hours, theophylline for 24 hours, inhaled
34 long-acting β
2
-agonists or combination treatments, cromoglycate, montelukast, short-
35 acting antihistamine drugs for 48 hours, and long-acting antihistamines for 5 days.
36 In order to gain further insight into the source of the salivary leukotrienes, analyses
37 were performed in urine and saliva from 8 patients with atopic asthma (5F/3M, age range
38 19-55 years). Samples were collected at baseline and after allergen provocation while
39 screening for another study (approved by the local ethics committee, Dnr 04-470/1-4).
40
41 Study design (Table II in the main text)
42 After an initial screening visit including physical examination and spirometry, eligible
43 patients were enrolled for a baseline visit (visit 1), followed by an aspirin provocation
Gaber et al 3
44 visit after 3 to 10 days (visit 2), except for one subject who returned for the provocation
45 visit after 3 months (identified as ATA). At the baseline visit, measurement of F E
NO
was
46 followed by collection of saliva and urine samples, and induction of sputum in that order.
47 On the second visit, subjects underwent a lysine-aspirin inhalation challenge as described
48 in the EAACI/GA
2
LEN guidelines.[1] Thus, increasing doses were administered at 30
49 minute intervals until a fall in FEV
1
of 20% or greater, as compared with post saline
50 FEV
1
, was obtained (these subjects were assigned as AIA), or when the maximum
51 cumulative dose of lysine-aspirin (600 µmol) was reached without significant
52 bronchoconstriction or other adverse symptoms (these subjects were assigned as ATA).
53 The cumulative provocative dose causing 20% decrease in FEV
1
(PD
20
) was calculated
54 by linear interpolation of the last 2 points of the dose-response curve. One hour before
55 the start of the lysine-aspirin challenge, F E
NO
was measured, and samples of saliva, urine
56 and blood were collected. During the provocation, samples of saliva and urine were
57 collected every hour. Blood was collected immediately after the end of provocation, and
58 at 30 minutes and 2 hours after provocation. Hourly collections of saliva and urine were
59 continued up to two to three (saliva) and three (urine) hours, respectively.
60
61
In the allergen challenge experiment, saliva samples were collected at baseline, and at 15 and 45 minutes after end of provocation (i.e. fall in FEV
1
≥ 20%). Urine samples
62 were collected at baseline and at one hour after end of provocation.
63
64 Measurement of F
E NO
65 Exhaled nitric oxide was analyzed by a NIOX™ device (Aerocrine AB, Solna, Sweden)
66 at a flow rate of 50 mL/s as described by the ATS/ERS guidelines.[2] The subjects were
Gaber et al 4
67 instructed to avoid intake of caffeine-containing beverages, vegetables or to exercise 4
68 hours before F E
NO
measurements. The subjects washed their mouth with water followed
69 by 10% bicarbonate solution before the measurement procedure to decrease
70 contamination from the oral cavity.
71
72 Saliva collection
73 Subjects were instructed to wash their mouth with water before collecting 5 mL of saliva.
74
75
The sample was stored at -70°C. Before assayed, the sample was thawed and centrifuged at 1500 x g for 10 min (+4
C), and the supernatant was subsequently
76 analysed.
77
78 Urine collection
79 The voided volume was measured and the urine samples were stored at -20°C until
80 assayed.
81
82 Ex vivo blood incubation
83 Whole blood was collected and ex vivo stimulation with ionomycin (calcium salt from
84 Streptomyces conglobatus , Sigma-Aldrich Co., Stockholm, Sweden) was performed as
85 previously described.[3] Briefly, freshly drawn blood was kept in room temperature and
86 incubated within 1-2 hrs after venipuncture. Ionomycin was dissolved in 95% ethanol
87
88 and added in a 1/10 dilution with autologous plasma. Aliquots of blood (1 mL) were preincubated at 37°C for 2 min, vehicle (95% ethanol) or ionomycin were added in 50 µl
Gaber et al 5
89 of autologous plasma. Final concentration of ionomycin was 50 µM. Incubation was
90 continued for 15 min at 37°C and interrupted on ice. Plasma was obtained by
91 centrifugation at 714 x g for 5 min, and stored at -70°C until assayed.
92
93 Sputum induction
94 Sputum induction was performed according to the ERS guidelines [4, 5]. The subjects
95 were pre-treated with 2x200 µg inhaled salbutamol to inhibit excessive airway
96 constriction. The subjects were instructed to expectorate sputum into a sterile tube after
97 inhaling an aerosol of isotonic saline and increasing doses of hypertonic saline,
98 administered from an ultrasonic nebuliser (Ultra Neb 2000; DeVilbiss Health Care,
99 Somerset, PA). The nebuliser output was 6 mL·min
-1
. The concentrations of saline were
100 0.9, 3, 4 and 5%. The duration of each inhalation was 7 minutes. After each period of
101 inhalation, the subjects were instructed to blow their nose and to rinse their mouth with
102 water to minimize contamination of the sputum sample. The subjects were asked to
103 cough deeply and to attempt to expectorate sputum. FEV
1
was monitored after 1, 2, and 7
104 minutes. If the FEV
1
fell with >10% after inhalation of isotonic saline, the induction
105 procedure was stopped. If the FEV
1
fell with <10%, the induction was continued with
106 increasing concentrations of saline. If the FEV
1
fell between 10-20% after inhalation of
107 hypertonic saline, the concentration of saline was not increased but repeated, and the
108
109 induction was stopped if the FEV
1
had fallen by >20%. The sample was considered adequate when it weighed ≥1 g.
110
111 Sputum processing
Gaber et al 6
112 Whole sputum was processed according to the ERS guidelines with some modifications
113 [6]. Dithiothreitol (DTT; Sputolysin® Reagent; EMD Biosciences, Inc., San Diego, CA)
114 0.1% was added to the sample equivalent to 4x sputum weight and rocked for 15 minutes.
115 Phosphate-buffered saline was added to an equal volume of DTT and the sample was
116
117 rocked for an additional 5 minutes. The sample was filtered through a 70 µm cell strainer
(BD Falcon™, BD Biosciences, San Jose, CA) and centrifuged at 400 x g , 10 minutes.
118 The supernatant was stored at -70ºC until assayed for fluid-phase mediators. Cytospins
119 were prepared from the cell pellet and stained with May-Grunwald Giemsa (Sigma-
120 Aldrich Co.). Cell differential was performed by counting 500 cells in random fields.
121 Each cytospin preparation was counted twice. The results of the cell differentials are
122 expressed as a percentage of the total number of non-squamous cells, except for the
123 squamous cells that are expressed as the percentage of the total cell number.
124
125 Measurement of CysLTs, LTB
4
, and 9α,11β-PGF
2
126 Analyses of CysLTs, LTB
4
and 9α,11β-PGF
2
were performed in serially diluted aliquots
127 of the respective samples by enzyme immunoassays (Cayman Chemical Co., Ann Arbor,
128 MI) as previously described.[3, 7] The cysteinyl-leukotriene assay used a CysLT
129 antiserum with 100% cross-reactivity to LTC
4
and LTD
4
, and 67% for LTE
4
. Leukotriene
130
131
E
4
was used as tracer. Results of CysLTs analyses are expressed as LTE
4
equivalents.
The detection limits for LTB
4
, LTE
4
and 9
,11
-PGF
2
were 3.9, 7.8 and 7.8 pg/mL,
132 respectively. The final concentrations of LTE
4
and 9α,11β-PGF
2
in urine are given as ng
133 per mmol of creatinine. Creatinine was determined in urine samples using a modification
134 of Jaffe’s creatinine protocol.[8]. For analyses of LTB
4
and CysLTs in sputum, the same
Gaber et al 7
135 concentration of DTT (0.04%) as in the sputum supernatant was added to the standard
136 curve and EIA buffer.
137
138 Measurement of CC-16
139 Levels of CC-16 in serum were determined using an enzyme-linked immunosorbent
140 assay for serum CC-16 from BioVendor Laboratory Medicine (Brno, Czech Republic),
141 according to the protocol provided by the manufacturer. All analyses were performed in
142 duplicate. In addition to the quality controls provided by the manufacturer, a pooled
143 serum standard of known CC-16 concentration and a CC-16-immunodepleted serum were
144 included in each assay to control for performance and interassay variability.
145
146 Statistical analysis
147 Baseline levels of F E
NO
were analyzed by Student’s t-test to assess differences between
148 the groups. The F E
NO
results are expressed as mean and standard deviations. All other
149 results were analyzed using the non-parametric tests of Mann-Whitney rank-sum test and
150 Wilcoxon signed-rank test. Results are expressed as medians and interquartile range
151 (IQR). A p-value of <0.05 was regarded as significant.
152 For urine, the mean value from four baseline samples (the first two samples from
153
154 the baseline visit and from the provocation visit) was used to determine baseline values.
The average concentration of LTE
4
or 9
,11
-PGF
2
in the first two urine samples taken
155 on the day of provocation (i.e. before and after inhalation of the diluent) were considered
156 as the pre-provocation value. For the post-provocation results, the average concentration
157 in the last two urine samples collected two and three hours after inhalation of the highest
Gaber et al 8
158 aspirin dose, were used to calculate peak values for the ATA group. For the AIA group,
159 the actual peak value within 3 hours after the last aspirin dose was used. For saliva, the
160 mean of two baseline samples were used to estimate baseline values, viz.
the first sample
161 from the baseline visit and the first sample from the provocation visit. For the
162 provocation visit, the first sample was regarded as the first and true pre-provocation value
163 (pre 1). The sample taken before the last inhaled dose was designated as the second pre-
164 provocation value (pre 2) in order to distinguish from the three hourly samples that were
165 collected after the max drop in lung function (for AIA), or after the inhalation of the
166 highest dose of lysine-ASA (for ATA). Post-provocation samples of saliva collected up to
167 2-3 hours after the end of provocation were compared with the pre-provocation results.
168
Gaber et al 9
189
190
191
192
193
194
195
179
180
181
182
183
184
185
186
187
188
170
171
172
173
174
175
176
177
178
1.
2.
3.
4.
5.
6.
7.
8.
169 REFERENCES
Nizankowska-Mogilnicka E, Bochenek G, Mastalerz L, Swierczynska M, Picado
C, Scadding G, Kowalski ML, Setkowicz M, Ring J, Brockow K, et al.
EAACI/GA2LEN guideline: aspirin provocation tests for diagnosis of aspirin hypersensitivity. Allergy 2007.
ATS/ERS recommendations for standardized procedures for the online and offline measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide,
2005. Am J Respir Crit Care Med 2005; 171: 912-930.
Gyllfors P, Kumlin M, Dahlen SE, Gaber F, Ehrs PO, Dahlen B. Relation between bronchial responsiveness to inhaled leukotriene D4 and markers of leukotriene biosynthesis. Thorax 2005; 60: 902-908.
Paggiaro PL, Chanez P, Holz O, Ind PW, Djukanovic R, Maestrelli P, Sterk PJ.
Sputum induction. Eur Respir J Suppl 2002; 37: 3s-8s.
Pizzichini E, Pizzichini MM, Leigh R, Djukanovic R, Sterk PJ. Safety of sputum induction. Eur Respir J Suppl 2002; 37: 9s-18s.
Efthimiadis A, Spanevello A, Hamid Q, Kelly MM, Linden M, Louis R,
Pizzichini MM, Pizzichini E, Ronchi C, Van Overvel F, Djukanovic R. Methods of sputum processing for cell counts, immunocytochemistry and in situ hybridisation. Eur Respir J Suppl 2002; 37: 19s-23s.
Brannan JD, Gulliksson M, Anderson SD, Chew N, Seale JP, Kumlin M.
Inhibition of mast cell PGD2 release protects against mannitol-induced airway narrowing. Eur Respir J 2006; 27: 944-950.
Creatinine - Jaffe's method. World Health Organization; 2006 [Cited 2007
November 19]. Available from http://www.searo.who.int/en/section10/section17/section53/section481_1755.htm