"in situ" mantle cell lymphoma (<5% of all lymphoid cells)
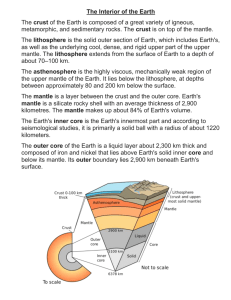
advertisement
LW43.2: "IN SITU" MANTLE CELL LYMPHOMA (<5% OF ALL LYMPHOID CELLS) Viera Nelson1, Patrick Browne1 and Bharat N Nathwani2 1.Genzyme Genetics, Hematopathology, Los Angeles, USA 2.Cedars-Sinai Medical Center & University of Southern California, Hematopathology, Los Angeles, USA vierkan@hotmail.com Clinical history: 62- year- old asymptomatic male in November 2008 had an excision biopsy of right axillary lymph node and there was no history of any malignancy. The initial clinical staging was inconclusive, and the issue was whether the disease was localized to the axillary lymph node (stage 1) or the porta hepatic and inguinal lymph nodes were also involved (stage 3). The bone marrow was normal histologically, by flow cytometry and FISH. Patient received 6 cycles of Bendamustine and Rituxan and is in complete remission without disease, 14 months after diagnosis. Details of biopsy: The excised lymph node had 2 pieces that measure 4.2x3.7x2.1 cm and 2.3x1.7x1.0 cm. Formalin fixation. Histopathology: The 4 HE stained slides showed that more than 95% of the sections were benign. Follicles of uniform shape were present throughout, focally closely packed, and their germinal centers showed a mixture of benign centrocytes and centroblasts. Most follicles were completely surrounded by well-defined mantle zones, and their thickness varied from 10 to 30 mantle lymphocytes. 95% of the mantle cells had round and 5% slightly irregular nuclei. The nuclear chromatin of most cells was condensed and, the cytoplasm was scanty like that seen in benign mantle cells. Scattered, few, small mantle cell nodules were also present, whose cytologic features were identical to those seen in the mantle zones (photos 1, 2). Immunohistochemistry/immunophenotype: Overall, the total number of Bcl-1 + cells occupied < 5% of all lymphoid cells, and they were seen in the mantle zones and mantle cell nodules in variable numbers. Very few Bcl-1 + cells extended immediately inwards into the periphery of germinal centers, and a few also extended immediately outwards into the Tzones admixed with benign T-cells (Photos 3, 4, 5). In the intrerfollicular areas, bcl-1+ cells were rare. Thus, the Bcl-1+ cells were essentially localized to the mantle zones and mantle cell nodules. In contrast, the total number of the IgD + cells occupied about 10% of all lymphoid cells, and the IgD stained only the mantle cells. Moreover, <40% of the IgD + cells stained weakly, whereas >60% stained strongly resulting in a “two-tone” staining pattern. (Photos 6-8) The CD5 stained weakly all mantle cells and, had a two-tone staining pattern (Photos 9-11), wherein the malignant cells stained weakly, whereas the benign T-cells stained strongly (Photos 9-11). The number of weakly stained CD5 and weakly stained IgD + cells was very similar to the number of BCL-1 + cells. All mantle cells were also + with CD20, PAX-5 and bcl-2, but negative with CD23, and CD3. In the CD20 stain, <1 % of the cells were + in the interfollicular areas. Flow cytometry on bone marrow:: Polytypic B cells and no light chain restriction. Genetic/molecular analysis: FISH: 1. Paraffin block of the lymph node: Positive for CCND1/IGH rearrangement (Photo 12). 2. Bone marrow aspirate: Negative for CCND1/IGH rearrangement. Proposed diagnosis In situ mantle cell lymphoma (< 5 % of all lymphoid cells). Interesting feature(s) of the submitted case 1. Without the bcl-1 stain, the diagnosis of “in situ” mantle cell lymphoma could not have been made. This stain also permitted estimation of the number of positive (malignant) cells, their localization and distribution. 2. Because the malignant mantle cells were <5% of the total lymphoid cells present in the node, this is an “in situ” mantle cell lymphoma which is confined to the mantle zones and the mantle cell nodules, albeit in variable numbers. Thus, it seems that the spread of the malignant cells is initially, selectively localized/homed via their homing receptors to the areas where there are mantle cells (mantle zones and mantle cell nodules). This restricted localization of the bcl-1 positive cells strongly indicates that this mantle cell lymphoma is at an early stage, and other than the t(11;14) translocation, no other molecular abnormalities (second-hit) have been sustained by these bcl-1 + mantle cells. Any subsequent additional molecular abnormalities will result in histologic and clinical progression, however, it cannot be predicted when it will occur. 3. The findings in our case suggest that to ascertain the incidence of “in situ” mantle cell lymphoma, bcl-1 staining could be done on all biopsy sections that show mantle zones. And the results of such studies could provide practice guidelines for the pathologists about the use of the bcl-1 stain.