U.S. Pharmacy Practice Under Managed Care: Today and Tomorrow
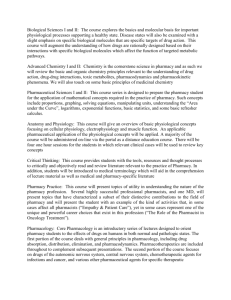
advertisement

FAPA 2002 Seoul 19th Congress of Asian Pharmaceutical Sciences and Practice Symposium Paper U.S. Pharmacy Practice Under Managed Care: Today and Tomorrow Jose P.B.Gallardo* and Purificacion S.Gallardo** Introduction Pharmacy practice in the United States of America is regulated by the individual States. State Boards of Pharmacy are empowered by laws to conduct licensing examinations, issue rules and regulations that govern the practice of pharmacy. Licensees are required to renew their licenses every two years. Proof of continuing education and compliance with other requirements are submitted to the Board of Pharmacy . Prescription dispensing is subject to Federal and State laws. Pharmacists are required to follow the stricter law. Pharmaceutical care is required by state laws. The majority of states require mandatory counseling. In addition to verbal counseling the patient is provided with a copy of the drug monograph. Dispensing of prescription drugs is the main professional function of licensed pharmacists. There are 343,816 licensed pharmacists in the 501 states including D.C., Guam, and Puerto Rico. Of these there are 216,248 with In-State addresses.1 There are numerous practice settings such as: Community pharmacy, Hospital pharmacy, Manufacturing/wholesale, Teaching/Government, and other areas, where licensed pharmacists work. Pharmacy technicians are allowed to work under the supervision of a licensed pharmacist. Different States have different requirements for registration or licensing of technicians. Duties that may be assigned depend on the practice location. In all States the responsible supervisor is the licensed pharmacist. Dispensing authority has also been allowed for other professions: Medical Doctor, Doctor of Osteopathy, Dentists, Podiatrists, Veterinarians, Doctor of Homeopathy (with limited formulary), Physician Assistants, Advanced Registered Nurse Practitioner, Clinical Nurse Specialist, Nurse/Midwife, Midwife, Nurse Practitioner, OB/GYN Nurse Practitioner, Pediatric Nurse Practitioner, Psychiatric Nurse Practitioner, Optometrist, Naturopathic Doctor.1 There are limitations on the foregoing practitioners for the dispensing authority. Physician dispensing is on the upsurge. Various reasons are given by medical doctors on why they dispense. A family practice doctor based in Salem, N.H., Azar A. Korbey,M.D. in an interview with Drug Topics said that dispensing adds approximately $20,000 a year to his bottom line.2 Allscripts, of Libertyville, Illinois, a corporation founded in 1986 is the major company that promotes physician dispensing. The number of dispensing doctors has jumped from 7,500 to 12,000 in 18 months. Allscripts carries 6,000 SKUs of which about 700 are for first-fill acute medications.2 Majority are for non-refillable acute care medications. Physician dispensing provides the patients with the 3 Cs – convenience, cost and compliance.2 *Jose P.B.Gallardo,R.Ph.,M.S.,FACA,FASCP **Purificacion S.Gallardo,R.Ph.,B.S.,ASCP President, Paramount Pharmacy Consultants Vice-President, Paramount Pharmacy Consultants Fellow American College of Apothecaries Member American Society of Consultant Pharmacists Fellow American Society of Consultant Pharmacists Health Care Financing – Traditional The traditional system of financing health expenditures is the fee for service method. Under the free enterprise system there are numerous and huge variations that exist in a community. Medical specialists will charge more for office visits than a family or general practice physician. Hospital charges also vary depending on the type of hospital, i.e. private, county or local government supported, state financed, federal government operated, charitable organization support, educational/teaching hospital, etc. Pharmacy service which mainly involved the dispensing of medications pursuant to a legal prescription may or may not involve a monetary transaction. The cost of a given prescription also varied extensively. Costs depended upon several factors that the owner or pharmacist have to factor in determining what the charge will be. Factors that get into play may include: drug cost plus a percent mark-up or fixed professional fee or sliding scale fee, maintaining credit/charging privileges to some clients, after hours service, delivery services, etc. Pharmacy has been defined as primarily providing dispensing services.3 In this narrow definition opportunities for new services were missed. Providing drug information to clients is not enough to broaden the scope of pharmacy practice. The future is in providing prescribing services. But who has the education and experience to prescribe?3 The answer is simple. The pharmacy educational system is not geared towards the clinical/diagnostic elements to compare with the specialized medical professionals. The classroom hours that Ophthalmologists are required to take are 2957 compared to 520 for pharmacists.3 This depicts a big deficiency if one claims to be a pharmacist-specialist. Pharmacy education should be constantly revised to prepare pharmacists to be credentialed as specialists. Right now there are pharmacists with special disease management training and are able to work in collaboration with medical specialists. There is a great need for pharmacists with special training. Pharmaceutical Care Hepler & Strand provides the definition: “the responsible provision of drug therapy for the purpose of achieving definite outcomes that improve a patient’s quality of life.”4 Pharmacists are now required to provide pharmaceutical care to the patient or to the responsible care giver. Are pharmacists ready to undertake training programs in Pharmaceutical Care? State pharmacy associations started conducting seminars for their members. These were presented as continuing education courses to their members. In addition professional pharmacy journals printed full length papers to provide the pharmacists with a better understanding of Pharmaceutical Care. Pharmacists have for many years provided free information to their clients/patients as a valueadded service. Patients always expected free services from the neighborhood pharmacy. Thus, the pharmacists find it very difficult to start charging a fee for pharmaceutical care services. The pharmacists who have undergone training in Disease State Management (DSM) also use their new expertise to augment the value added service that clients/patients look for. Financial gains are yet to be realized. Trends Toward Managed Care The physical location of the public dispensing area has always been located towards the rear of the store. It was elevated to provide the pharmacist with a vantage view of the front. Health and beauty aids were displayed nearer the pharmacy. After patients/clients drop off their prescriptions to the pharmacist they can wander around and will probably make an impulse purchase. If the patient/client needs other non-prescription (OTC) drugs the pharmacist will be able to offer suggestions. The additional sale will augment the profits of the pharmacy. The pharmacist was always a respected professional in his community and this is also reflected nationwide. Prior to 1996 the health care system in the US underwent about three evolutions. The growth in population and the industrialization of the U.S. Health care became a right of every citizen. Employers began to provide health benefits that included the families of their workers. This opened the door for reforms. From private contracts with health care providers the employers began to purchase insurance plans which include all aspects of medical care. Many felt that the government be involved with providing health care services particularly to old and low income citizens. Government involvement increased with the passage of the Medicare and Medicaid laws in 1965. With the ever increasing cost of health care a new delivery system was needed. President Nixon in 1973 signed a new law called the Health Maintenance Organization (HMO) Act. Incentives were provided to HMOs to promote their use by companies that have at least twenty-five employees. Managed care systems grew in number. Every health provider organization that was organized towards cost containment. During the last six years there was a proliferation of managed care organizations. The US health care system has been rated as the “best” because of the freedom of choice of physician, hospital and pharmacist with access to the latest surgical and treatment techniques. Insurance plans manage the payments for these health services. It is rated as the “worst” by people with no health insurance, under insured, and those whose insurances are not portable to the new employer’s health plan.5 Private and Public Health Care Private health care includes: employed, insured, middle-income and those using the private sector with Fee-For-Service Plans. The services are covered by health insurance. Premiums for single or family coverage are paid by both employer and employee through payroll deductions. The employee may have freedom of choice as to physician, hospital or pharmacy. Some employers have their health benefits on a self-insured basis managed by an insurance company with a specific contract for reimbursement of managing expenses on a percentage that is agreed upon. The employee usually has a deductible amount based on an annual projection of medical expenses.5 Deductible amounts may or may not include hospitalization expenses. Deductibles are out-of-pocket expenses for the insured. It is estimated that more than 50 percent of health care expenditures in the U.S. are spent by the private sector. There is an upward trend in the cost of health care for the private sector. The state of the economy influences the upward or downward spirals in health care. Add to this the cost of new drugs which prove to be more effective in treating specific diseases. Reduction in the length of hospital confinements results in the earlier return of the employee to active work. Public health care is a Federal Government provided care includes: Military medical care, Veterans Administration (VA), Civilian Health And Medical Program of the Uniformed Services (CHAMPUS), the Indian Health Service (IHS), Local government healthcare for the unemployed, uninsured, low-income Americans, Medicaid – a joint federal and state program that provides health care for the poor. Medicare – the beneficiaries are senior citizens covered by the Social Security amendments to persons 65 years and older.5 The Health Care Financing Administration (HCFA) now known as Centers for Medicaid & Medicare Services (CMS) administers both Medicaid and Medicare services. Managed Competition 6 In a free market economy competition in business is inevitable. Pharmacy is practiced mainly as a business. Ownership of a drug store or pharmacy is not limited to pharmacists. There is no limit in the number of retail outlets that a person or group of persons (investors) can operate. Thus, there are local chain stores, regional chains and even national chains. These are the establishments operated in the community setting – thus they are known as community pharmacies. Each of these ventures compete for the prescriptions written by various prescribers. Competition usually results in ‘lower’ prices. Pharmacists who are able to own their own community store are in constant pressure to provide lower prescription prices. Many are able to participate in buying groups to be able to reduce their cost of goods. Pharmacists become businessmen and constantly seek ways to promote their business. Those who are located in fairly large urban areas where several industries are operated may be able to enter into agreements to provide prescription services. They become primary providers for health care. Enhanced patient care services that a pharmacist is able to provide should be made available to physicians and other providers of care. A face-to-face consultation with other providers to share information enhances patient care management. Who pays the bills? The economics of the pharmacy business is dictated by the demands of the payers. Payers want more services for less money. Managed competition is not governed by the traditional law of ‘supply and demand’. Rather it is the entity that provides more for less dollars that beats the competition. Making better use of supportive personnel, automation and other technologies in the distribution of pharmaceuticals is what pharmacy needs to do to provide service at the lowest possible cost. Pharmaceutical benefit management companies are not the payers but are ‘middlemen’. Their role is to control the rising cost of medical care and are usually on the ‘combative’ end with pharmacy providers. The basis for prescription cost management is the heavy discounting of the average wholesale price (AWP) with a fixed ‘professional fee.’ This fee does not take into consideration the cost of the drug. The providers and administrators of health plans should organize their systems to provide good quality and cost effective care to produce the best outcomes for the beneficiaries. Patients need more rational management of drug therapy. This combined with pharmaceutical care will result in lower total costs of health care delivery. Patients must be made partners in their own health care management. A partnership between the 3 Ps (physician-patient-pharmacist) will result in a win-win situation if practice models and payment systems change before time runs out. The economics of health care has not included a provision to compensate for pharmaceutical care. Insurance companies nationwide have not recognized the value of the pharmacists’ role in disease management. In the institutional settings there is a better recognition of the value of pharmacist intervention. In the ambulatory care environment the patients still expect the free value added service from the pharmacist. An assessment of the cost effectiveness of pharmacist intervention will be a positive impact on the other costs of health care. The role of the pharmacist in managed competition has largely been overlooked. Society has not even begun to realize that the time pharmacists devote to providing pharmaceutical care needs to be properly compensated. A re-engineering of the whole practice of pharmacy including the physical layout of the practice area and the method of calculating the value of pharmacy services must be done. Are pharmacists ready to delegate their dispensing activities to technical assistants? Are corporate employers of pharmacists ready to recognize that the pharmacy is a primary health care facility? Will employee benefit managers and plan sponsors understand a new role of pharmacists to improve care and decrease costs of health services? Will pharmacy benefit managers change their attitudes, network support, and marketing practices to integrate real pharmaceutical care into their network strategies? 6 Generic Drugs in Managed Competition Pharmaceuticals constitute a small percentage of the total health care costs. However, health care spending is becoming a great concern for the payers. Employee beneficiaries pay for prescription drugs out of pocket. The U.S. government does not pay for the drugs that most Americans take. It does not even pay for Medicare beneficiaries medications outside of the hospital. It is estimated that only about 8% of the total cost of health care. Prescription drug costs should not really be an issue. In terms of health care expenditures corporations are changing their methods of calculating their budgets. It is no longer the benefits of taking prescription drugs rather the cost that takes prime consideration. With the increasing availability of generic drugs the cost of prescriptions should be lower. Drug substitution is mandated by the government as well as insurance companies. Many manufacturers compete for the generic market. This is good for the consumer. Multiple manufacturers join the ‘bandwagon’ whenever a branded drug loses patent protection. This results in a wide variation in costs. Managed care then sees an opening to put an upper limit for all claims they process. There are instances when manufacturers produce a ‘branded generic’ which they promote to physicians. What is a branded generic? It is a generic drug that is given a name that is short and easier to remember. Prescriber’s choice of drugs is also influenced by payers. Generic competition is on the increase. Managed care organizations use cost containment strategies to large groups of providers. Generic competition has been intensifying. Compared to the producer price index between 1989 and 1992 price increases declined from 9.5% to 6.4%. When measured against the consumer price index for the same period there was a decline from 9.5% to 5.6%.7 Generic drug costs have been on the decline. There is evidence that discounting has increased for existing drugs. Managed care organizations control almost 80% of the insured population. Formularies have been in use to control expenditures on drugs. In 1991 generic substitution was used by 70% of managed care organizations. Mandatory drug utilization reviews are used by 48%.7 After OBRA 90 (Omnibus Budget Revision Act) drug companies were required to reimburse the larger of 15.7% of the Average Market Price (AMP) or AMP minus the best price given in the market to the states. Between 1991 and 1995 the estimated savings of 3M$ to1,856M$. These amounts represent the lost revenue of drug manufacturers. The government is the single largest purchaser of pharmaceuticals. Managed Care Organizations The 2002 Eleventh Edition Executive Managed Care Directory published by Managed Care Interface,8 Bronxville, New York lists the following: 1. Health Maintenance Organizations (HMO) in the 50 states total 1,183 plus 3 in Puerto Rico. California alone has 128 HMOs. 2. Preferred Provider Organizations (PPO) in the 50 states total 954 plus 1 in Puerto Rico. California alone has 103 PPOs. 3. Pharmacy Benefit Managers (PBM) in the 50 states total 169 4. Third-Party Administrators (TPA) in the 50 states total 542 5. Utilization Review Services (UTS) in the 50 states total 120 6. Physician-Hospital Organization (PH0) unknown number 7. Independent Practice Association (IPA) unknown number 8. Blue Cross/Blue Shield (BC/BS) at least one in each state 9. Exclusive Provider Organization (EPO) unknown number 10. Independent Practice Organization (IPO) unknown number 11. Drug Price Review (DPR) unknown number 12. Primary Care Network (PCN) unknown number 13. Primary Care Physician (PCP) unknown number, more numerous than HMOs 14. Quality Review Organization (QRO) unknown number There are more local companies that are involved in managed care but are not listed in the directory. Managed Care Terms A thru Z Managed Care Terms,9 published by Medicom International is the most complete list of the terminology that is used in conjunction with managed care. Following are some of the terminologies with definitions that have been used in the earlier and in the next segments of this paper. Access A patient’s ability to obtain medical care determined by factors such as the availability of medical services, their acceptability to the patient, the location of the health care facilities, transportation, hours of operation, and cost of care. Actively at Work A requirement of many insurances policies stipulating that if a given employee is not actively at work on the day the policy goes into effect, medical coverage will not be provided until the employee returns to work. Actual Acquisition Cost The pharmacist’s net payment made to purchase a drug product, after taking into account such items as purchasing allowances, discounts, and rebates. Acute Care Treatment for a short-term, episodic illness or health problem. Adjudication Processing a claim through a series of edits to determine proper payment. Administrative Costs The costs assumed by a managed care plan for administrative services such as claims processing, billing, and overhead costs. Allied Health Personnel Trained and licensed health workers other than physicians, dentists, optometrists, chiropractors, podiatrists and nurses. Allowable Charge The maximum fee that a third party will reimburse a provider for a given service. Allowable Costs Items or elements of an institution’s costs that are reimbursable under a payment formula. Allowable may exclude, for example, uncovered services, luxury accommodations that are not reasonable, and expenditures that are unnecessary. Alternate Medical Care Medical care received in lieu of inpatient hospitalization. Examples include outpatient surgery, home health care, and skilled nursing facility care. It also may refer to nontraditional care delivered by providers. Ambulatory Care Health services delivered on an outpatient basis. If the patient makes a trip to the doctor’s office or surgical center without an overnight stay, it is considered ambulatory care. Assisted Living Facility (ALF) A residential setting that provides or coordinate personal care services, 24-hour supervision and assistance, activities, and health-related services, and is designed to minimize the need to move and to maximize privacy and independence. Authorization As it applies to managed care, authorization is the approval of care, such as hospitalization, Preauthorization may be required before admission takes place or care is given by nonHMO providers. Beneficiary A person who is eligible to receive insurance benefits. Benefit Package Services an insurer, government agency, health plan, or employer offers under the terms of a contract. Blue Cross A hospital service insurance plan that provides benefits covering specified healthrelated services and pays member hospitals directly for services rendered. Blue Shield A medical service insurance plan that provides benefits covering specified physicianrelated services and pays either the patient or the physician. Cafeteria Plan A corporate benefits plan under which employees are permitted to choose among two or more options that consist of cash and certain qualified benefits. Cafeteria plans are also called flexible benefit plans or flex plans. Capitation A per-member, monthly payment to a provider that covers contracted services and is paid in advance of its deliver. In essence, a provider agrees to provide specified services to plan members for this fixed, predetermined payment for a specified length of time (usually a year), regardless of how many times the member uses the service. The rate can be fixed for all members or it can be adjusted for the age and sex of the member, based on actuarial projections of medical utilization. Carrier An insurer; an underwriter of risk. A voluntary association, corporation, partnership, or other nongovernmental organization that is engaged in providing, paying for, or reimbursing all or part of the cost of health services agreements, membership or subscription contracts, or similar group arrangements, in consideration of premiums or other periodic charges payable to the carrier. Chain Pharmacy One of a group of pharmacies under the same management or ownership. Chargeback An amount of money returned by a pharmaceutical manufacturer directly or through a wholesaler to a health plan after the purchase of pharmaceuticals. A chargeback is essentially a “discount” for the purchase of pharmaceuticals. It is usually the difference between the average wholesale price and the price bid by the pharmaceutical manufacturer. Chemical Equivalents Those multiple-source drug products containing essentially identical amounts of the same active ingredients, in equivalent dosage forms, and that meet existing physical/chemical standards. Chronic Care Care for a patient with a long-term illness. Co-insurance The percentage of the costs of medical services paid by the patient. This is a characteristic of indemnity insurance, POS, and PPO plans. The co-insurance is usually about 20% of the cost of medical services after the deductible is paid. Compliance Refers to capability of voluntarily following the written instructions for using a drug or other prescribed treatment regimen. Consultant Pharmacist A pharmacist who provides pharmacy and clinical services to a long-term care facility. Often, a consultant pharmacist has a community pharmacy practice and offers his or her services to local nursing homes. The services provided include drug regimen review and pharmaceutical care, among others. Continuum of Care A range of clinical services provided during a single inpatient hospitalization or for multiple conditions over a lifetime. It provides a basis for evaluating quality, cost, and utilization over the long term. Contracted Pharmacy (Network Pharmacy) A chain or independent retail pharmacy that has contracted with an MCO or PBM to provide prescription drugs to plan members based on financial arrangements calling for discounted dispensing fees or capitated payments. Co-payment A fee charged to HMO members to offset costs of paperwork and administration of each visit or pharmacy prescription filled. Today, nearly all health plans have implemented multitiered co-pays, particularly for pharmacy benefits. For instance, a prescription for a generic drug may be associated with only a $5 co-pay; a prescription for a preferred, branded product may have a $15 co-pay; and a non-preferred, branded product may have a $30 co-pay. Cost Containment A strategy that aims to reduce health care costs and encourages cost-effective use of services. Cost Effectiveness Usually considered as a ratio, the cost effectiveness of a drug or procedure, for example, relates the cost of that drug or procedure to the health benefits resulting from it. In health terms, it is often expressed as the cost per year per life saved. Coverage The health care services of benefits that are arranged, provided, or paid for through a health insurance plan for a group or an individual. Customary Charge The typical amount charged by a provider for a particular service. Payers typically pay the provider a percentage of this amount. Deductible A fixed amount of health care dollars of which a person must pay 100% before his or her health benefits begin. Most indemnity plans feature a $200 to $500 deductible, and then pay up to 100% of money spent for covered services above this level. Disease Management A philosophy toward the treatment of the patient with an illness (usually chronic in nature) seeking to prevent recurrence of symptoms, maintain high quality of life, and prevent future need for medical resources by using an integrated, comprehensive approach to health care. Pharmaceutical care, continuous quality improvement, practice guidelines, and case management all play key roles in this effort, which (in theory) will result in decreased health care costs as well. Dispensing Fee A charge levied by pharmacists and added to the price of a drug, which covers both their pharmaceutical expertise and the cost involved in the prescription. Drug Maintenance List Also called an additional drug list, it is a catalog of a limited number of prescription medications, as designed by an MCO, commonly prescribed by health care providers for long-term patient use. This list is usually modified on a regular basis. Drug Regimen Review (DRR) A frequent evaluation of the medications being taken by a patient in intermediate- or long-term care facilities. Typically performed by a pharmacist, DRR is especially useful in avoiding adverse drug reactions and drug interactions in patients taking multiple medications. Drug Use Evaluation (DUE) An evaluation of prescribing patterns of physicians to specifically determine the appropriateness of drug therapy. There are three forms of DUE: prospective (before or at the time of prescription dispensing), concurrent (during the course of drug therapy), and retrospective (after the therapy has been completed). Drug Utilization Review (DUR) The process of retrospectively evaluating prescription drug use, physician prescribing patterns, or patient drug utilization to determine the appropriateness of drug therapy. Electronic Data Interchange (EDI) The electronic exchange (through computers) of information between two or more organizations. In the health care setting, EDI has made enormous gains in the transmission of claims information. Exclusive Provider Organization (EPO) A form of PPO in which patients must visit a caregiver who is on its panel of providers. If an outside provider is visited, the EPO will offer limited or no coverage for the office or hospital visit. Extended Care Facility A nursing home-type setting that offers skilled, intermediate, or custodial care. Fee for Service Traditional provider reimbursement in which the physician is paid according to the service performed. This is the reimbursement system used by conventional indemnity insurers. Flexible Benefit Plan A benefit program that offers employees a number of benefit options, allowing them to tailor benefits to their needs. Formulary The panel of drugs chosen by a hospital, MCO, or other health plan that is used to treat patients. Formularies may be of an open or closed type. Drugs excluded from a closed formulary are only used in rare, specific circumstances. Gatekeeper Most health plans rely on the primary care physician, or “gatekeeper,” to screen patients seeking medical care and effectively eliminate costly and sometimes needless referrals to specialists for diagnosis and management. The gatekeeper is responsible for the administration of the patient’s treatment, and must coordinate and authorize all medical services, laboratory studies, specialty referrals, and hospitalizations. In most HMOs, if an enrollee visits a specialist without prior authorization from the designated primary care physician, the medical services will have to be paid in full by the patient. Generic Drug A chemically equivalent copy designed from a brand-name drug whose patent has expired. Typically less expensive and sold under the common name for the drug, not the brand name. Generic Substitution In cases in which the patent on a specific pharmaceutical product expires and drug manufacturers produce generic versions of the original branded product, the generic version of the drug (which is theorized to be the exact same product manufactured by a different firm) is dispensed even though the original product is prescribed. Most MCOs and Medicaid programs mandate generic substitution because of the generally lower cost of generic products. Group Purchasing Organizations (GPOs) These groups consist of two or more hospitals that at least some of their purchasing through contracts developed by a central office. Proprietary groups/Hospital chains – Organizations that own, manage, or lease member hospitals. “Pure” GPOs – Local or regional groups that exist for the exclusive purpose of providing contract services. Super Groups – Regional and local hospital groups that are bonded together to negotiate contracts on a national scale. Health Care Financing Administration (HCFA) Now called the Centers for Medicare & Medicaid Services, it is the federal agency responsible for administering Medicare and overseeing states’ management of Medicaid. Health Insurance Portability and Accountability Act (HIPAA) of 1996 Also known as the Kennedy-Kassebaum Act, HIPAA intends to provide better portability of employer-sponsored insurance from one job to another. Thus, preventing “job lock,” or the need to stay in the same position because of its health care benefits. The Act also outlaws excluding people from obtaining health insurance because of preexisting conditions and offers tax deductions to those who are selfemployed to help pay for their health benefits. It is widely viewed as a first step in the federal initiative to significantly reduce the number of uninsured people in this country. One of the major provisions of the Act was the implementation of medical privacy rules to protect the confidentiality of patient health information. This includes the appointment of an information privacy officer in every health care organization whose responsibility it is to protect health information in accordance with the guidelines of the Act. Health Maintenance Organization (HMO) A form of health insurance in which its members prepay a premium for health services, which generally includes inpatient and ambulatory care. For the patient, it means reduced out-of-pocket costs (i.e., no deductible), no paperwork (i.e., insurance forms), and only a small co-payment for each office visit to cover the paperwork handled by the HMO. HMO Act of 1973 Federal law that required employers with more than 24 employees to offer an alternative to conventional indemnity insurance in the form of a federally qualified HMO. The main intention of the Act was to encourage HMO development. Inpatient A patient admitted to a hospital who is receiving services under the direction of a physician for at least 24 hours. Integrated Health Care Systems Health care financing and delivery organizations created to provide a “continuum of care,” ensuring that patients get the right care at the right time from the right provider. This continuum of care from primary care provider to specialist and ancillary provider under one corporate roof guarantees that patients get the appropriate care, thus saving money and increasing quality of care. Intermediate Care Facility (ICF) A facility that provides basic nursing care and other restorative services under periodic medical direction. International Classification of Diseases, 9th Edition (Clinical Modification) (ICD-9-CM) A listing of diagnoses and identifying codes for reporting diagnoses of patients. The coding and terminology provide a uniform language that can designate primary and secondary diagnoses and provide for reliable, consistent communication on claim forms. Joint Commission on Accreditation of Healthcare Organizations (JCAHO) A private, nonprofit organization that evaluates and accredits health care organizations that provide inpatient mental health care, ambulatory care, home care, and long term care services. Long-Term Care Services ordinarily provided in a skilled nursing, intermediate care, personal care, supervisory care, or elder care facility. Mail Order Pharmacy A method of dispensing medication directly to the patient through the mail. Mail order drug distributors can purchase drugs in larger volumes than retail or wholesale outlets. Managed Competition One type of health care reform that would correct the inequalities of the health delivery system through increased competition. Health plans would compete on the basis of cost and other factors; health care purchasers would have information at their disposal that would allow them to compare competing health plans across several dimensions of performance. Managed Health Care The sector of health insurance in which health care providers are not independent businesses run by, for example, the private practitioner, but by administrative firms that manage the allocation of health care benefits. In contrast with conventional indemnity insurers, who do not govern the provision of medical services and simply pay for them, managed care firms have a significant say in how services are administered so that they may better control health care costs. HMOs and PPOs are examples of MCOs. Management Services Organization (MSO) A type of integrated health care plan in which the hospital provides administrative services to a physician group and the physician group provides patients to the hospital. Maximum Allowable Cost List A list of prescription medications, established by the health plan and distributed to pharmacies, that will be covered at a generic product level. Medicaid An entitlement program run by both the state and federal governments for the provision of health care insurance to patients younger than 65 years of age who cannot afford to pay for private health insurance. The federal government matches the states’ contribution on a certain minimal level of available coverage. The states may institute additional services, but at their own expense. Medicaid Prudent Pharmaceutical Purchasing Act (MPPPA) Enacted as part of the Omnibus Budget Reconciliation Act of 1990. It provides that Medicaid must receive the best price of any institutional purchaser of pharmaceuticals. In doing so, drug companies provide rebates to Medicaid that are the difference between the discounted price and the price at which the drug was sold. This bill, which was introduced by Senator David Pryor of Arkansas, has resulted in cost shifting throughout the health industry. For example, HMOs, which were previously able to negotiate some of the best discounts with manufacturers and wholesalers, are now given lower discounts by the vendors to compensate for the Medicaid share of discounted revenue. Medical Savings Account (MSA) A method of paying for health insurance, made available through a pilot program mandated by the Health Insurance Portability Act of 1996. The MSA allows a person to place money in an interest-bearing account that can be used to purchase health insurance policies, and to pay co-pays, deductibles, etc. Anything remaining in the account at the end of the year is carried over to the next year, allowing the account to grow. Medicare An entitlement program run by the Centers for Medicare & Medicaid Services (formerly the Health Care Financing Administration) of the federal government through which people aged 65 years or older receive health care insurance. Medicare Part A covers hospitalization and is a compulsory benefit. Medicare part B covers outpatient services and is a voluntary service. Medigap Insurance provided by carriers to supplement the monies reimbursed by Medicare for medical services. Since Medicare pays physicians for services according to their own fee schedule, regardless of what the physician charges, the individual may be required to pay the difference between Medicare’s reimbursable charge and the physician’s fee. Medigap insurance is meant to fill this gap in reimbursement, so that the Medicare beneficiary is not at risk for the difference. MGMA Medical Group Management Association. Nurse Practitioner A registered nurse who has advanced skills in the assessment of physical and psychosocial health status of individuals, families, and groups in a variety of settings through medical history taking and physical examination. Nursing Home A facility for the provision of long-term care to patients with chronic and disabling conditions. Most nursing home patients are elderly and have limited potential for rehabilitation. On-Line Adjudication An electronic assessment of claims at the point of service meant to detect potential problems that should be addressed before drugs are dispensed to patients. Outcomes Management A clinical outcome is the result of medical or surgical intervention or nonintervention. Improved clinical outcomes may increase patient and payer satisfaction while holding down costs. It is thought that through a database of outcomes experience, caregivers will know better which treatment modalities result in consistently better outcomes for patients. Outcomes management will, as a natural consequence, lead to medical protocols. Out-of-Pocket Costs The share of health service payments made by the enrollee. Outpatient A patient who receives health care services without being admitted to a hospital. Over-the-Counter (OTC) Drug A drug product that does not require a prescription under federal or state law in order to obtain it. Participating Provider May apply to either professional or institutional providers who have contracted with a managed care plan. Payer A public or private organization that pays for or underwrites coverage for healthcare expenses. Per Member Per Month (PMPM) A unit of measurement related to each enrollee for each month. Per Member Per Year (PMPY) An amount in reference to each enrolled member each year. Pharmaceutical Care A concept in providing health care; it is a strategy that attempts to utilize drug therapy more efficiently to achieve definite outcomes that improve a patient’s quality of life. A pharmaceutical care system requires a reorientation of physicians, pharmacists, and nurses toward effective drug therapy outcomes. It is a set of relationships and decisions through which pharmacists, physicians, nurses, and patients work together to design, implement, and monitor a therapeutic plan that will produce specific therapeutic outcomes. Pharmacy and Therapeutics (P&T) Committee A group of physicians, pharmacists, and other health care providers from different specialties, who advice a managed care plan regarding safe and effective use of medications. The P&T manages the formulary and acts as the organizational line of communication between the medical and pharmacy components of the health plan. Pharmacy Benefit Management Company (PBM) An organization dedicated to providing prescription benefits to enrollees of managed care plans that utilizes existing community pharmacies. The PBM contracts as a provider group with the managed care organization, so that the individual pharmacies receive negotiating representation in numbers and the prepaid health plan does not have to provide the capital necessary to start, own, and operate their own pharmacy department. Physician Assistant A health care professional certified to perform certain duties, such as history taking, diagnosis, drawing blood samples, urinalysis, and injections under the supervision of a physician. The physician assistant can serve as a primary care provider. Physician-Hospital Organization (PHO) A type of integrated health care system that, in its simplest form, is an organization that collectively commits both the physician and the hospital to payer contracts. They sometimes use existing IPA structures or individual physician contracting. In its most effective form, the PHO must commit the entire physician and hospital panel, without an output, to the PHO organization. Point of Sale (POS) A term usually used to describe information use for on-line technology. For example, computer terminal at the pharmacist’s counter (i.e., the “point of sale”) connected to an MCO’s information system will be able to inform the pharmacist whether the patient’s prescription is for a formulary product and the requirement co-payment before the prescription is dispensed. HMOs refer to it as point-of-service. Preferred Provider Organization (PPO) PPOs are managed care organizations that offer integrated delivery systems (i.e., networks of providers) that are available through a vast array of health plans and are readily accountable to purchasers for cost, quality, access, and services associated with their networks. They use provider selection standards, utilization management, and quality assessment techniques to complement negotiated fee reductions as an effective strategy for long-term cost savings. Under a PPO benefit plan, covered individuals retain the freedom of choice of providers but are given financial incentives (i.e., lower out-of-pocket costs) to use the preferred provider network. Preferred provider organizations are marketed directly to employers as well as to insurance companies and TPAs, who then market the network to their employer clients. Preferred Providers Physicians, hospitals, and other health care providers who contract to provide health services to persons covered by a particular health plan. Prescription Medication A drug that has been approved by the Food and Drug Administration (FDA) and that can, under federal or state law, be dispensed only pursuant to a prescription order from a duly licensed physician. Primary Care Network A group of primary care physicians who have joined together to share the risk of providing care to their patients, who are members of a given health plan. Primary Care Physician (PCP) Sometimes referred to as a “gatekeeper,” the primary care physician is usually the first doctor a patient sees for an illness. The physician then treats the patient directly, refers the patient to a specialist (secondary care), or admits the patient to a hospital. Often, the family care physician is a family doctor or internist. Prior Authorization The process used to obtain prior approval as to the appropriateness of a service or medication. Prior authorization does not necessarily guarantee coverage. Prospective Payment System (PPS) Mandated by the Balanced Budget Amendments of 1997, the Medicare PPS affects many aspects of care (skilled nursing, outpatient, home health, rehabilitation, etc.). As the name indicates, the PPS seeks to provide preset fees to Medicare providers for care provided to beneficiaries, based on the varying resource needs of the patient. Provider Any supplier of health care services, i.e., physician, pharmacist, case management firm, etc. Registered Nurse (RN) A nurse who has graduated from a formal, accredited program of nursing education, and who has been granted an RN license by the appropriate state authority after passing a licensing examination. Retrospective Review A manner of judging medical necessity and appropriate billing practices for services that have already been rendered. Secondary Care Health care services provided by medical specialists who generally do not have first contact with patients, but are referred to them by primary care and family physicians. Self-Funding Also known as self-insurance is a health care plan funded entirely by employers who do not purchase insurance. Self-funded plans may be self-administered, or the employer may contract with an outside administrator for an administrative-services-only arrangement. Skilled Nursing Facility (SNF) Typically an institution for convalescence or a nursing home, the skilled nursing facility provides a high level of specialized care for long-term or acute illness. It is an alternative to extended hospital stays or difficult home care. Subscriber The person in whose name and individual or family contract is issued. Therapeutic Alternatives Drug products containing different chemical entities but which should provide similar treatment effects, the same pharmacological action, or similar chemical effects when administered to patients in therapeutically equivalent doses. Therapeutic Substitution A drug that is believed to be therapeutically equivalent (i.e., will achieve the same outcome) to the exact drug prescribed by a physician. The drug is substituted by the dispensing pharmacist without the need to obtain permission from the physician. Therapeutic substitution is generally mandated by formulary or cost-containment concerns. Third-Party Administrator (TPA) An organization that is outside of the insuring organization that handles administrative duties and sometime utilization review. Third-party administrators are used by organizations that fund the health benefits but do not find it cost effective to administrate the plan themselves. Third-Party Payer A public or private organization that pays for or underwrites coverage for health care expenses. Tricare The military’s integrated health care delivery system. The Tricare system includes the Civilian Health and Medical Program of the Uniformed Services (CHAMPUS). Tricare gives the regional military treatment facilities control of health care delivery costs and purchasing. The Tricare system splits U.S. military bases into 12 designated regions. One major military health care facility within each of the regions is designated as the “lead agent,” which is responsible for organizing and maintaining an integrated delivery network, including civilian providers. Universal Formulary (National Formulary) Formulary developed by a PBM or large MCO from which participating plans or affiliated MCOs may select drugs for their own plan or local formulary. Urgent Care Center A medical facility where ambulatory patients can be treated on a walk-in basis, without an appointment, and receive immediate, non-emergency care. The urgent care center may be open 24 hours a day; patients calling an HMO after hours with urgent, but not emergent, clinical problems are referred to these facilities. Usual, Customary, and Reasonable (UCR) Fee-for-service payment to physicians based on the usual and customary fee for the same service in the area where the practice is located or on some other judgment of reasonableness, Value-Added Services These services, such as handling complicated paperwork and reimbursement forms, are offered by pharmaceutical manufacturers or drug wholesalers to enhance their competitive edge. Vertical Integration A provider strategy, usually accomplished through partnerships, joint ventures, and contractual agreements, whereby providers establish a local or regional health care delivery network serving a geographically-defined population. This system provides a seamless range of services and delivery settings (clinical, pharmacy, and/or insurance) for patients. Workers’ Compensation A state-governed system that addresses work-related injuries. Under this system, employers assume the cost of medical, occupational, or other treatment and wages losses stemming from a workers’ job-related injury. In return, employees give up the right to sue employers. Managed Care Trends Digest 200110 HMO Demographics Total number of HMOs fall but HMO enrollment continues to rise in 1999 The number of operating HMO plans, dropped 9.1% in 1999 to 820 from 902 in 1998. On the other hand, enrollment in HMOs continued to grow in 1999, topping the 100 million mark when it soared to 104.6 million from 55 million in 1994. Medicare and Medicaid enrollment in HMOs more than doubled and quadrupled, respectively. Medicare enrollees rose from 3 million in 1994 to 6.8 million in 1999. Medicaid enrollees rose from 2.6 million in 1994 to 11.3 million in 1999. HMO Utilization Total increase in physician encounters and ambulatory visits reverses The average numbers of physician encounters and ambulatory visits per member per year (PMPY) for commercial, Medicare, and Medicaid HMO members declined between 1998 and 1999. PMPY for Medicare members rose 84.6% (to 12.0) between 1990 and 1998, but then fell 25.0% in 1999 (to 9.0). The number of ambulatory visits PMPY for commercial members increased 25.0% between 1990 (1.6) and 1998 (2.0), but slipped 20.0% (to 1.6) in 1999. HMO Pharmacy Utilization Share of HMOs using in-house pharmacies doubles over a 10-year period. Between 1990 and 1999, the percentage of HMOs with in-house pharmacies nearly doubled, to 39.1% from 20.0%. From 1994 to 1998, the percentage of HMOs using mail-service pharmacies nearly tripled, to 83.0% from 28.9%, before declining slightly in 1999, to 82.7%. Between 1998 and 1999, HMO premiums for outpatient pharmacy benefits per member per month (PMPM) continued to increase for individuals (up 2.7%, to $17.43 from $16.98) and for families (up 2.0% to $43.42 from $42.49) alike. Integrated System Trends Share of systems defined as the most highly integrated surpasses 50% Of the 585 health care systems in the process of integrating in 2000, just over half (51.1%) were defined by this Digest as the most highly integrated. In 1995, by comparison, just under three-tenths (29.9%) of all systems met this definition. In the five years from 1995 to 2000, the number of highly integrated systems nearly doubled, to 299 from 159. During this period, moreover, highly integrated systems grew larger. In 1995, just 124 systems had four or more delivery components; by 2000 that number rose to 239. Medical Group Practices Medical groups grew in number and size during decade of the 1990s. The number of medical group practices (defined in this Digest as those with at least five physicians) increased by just 70% between 1997 and 2000, while the total number of physicians in those groups rose by more than a third (34.25). The smallest groups, those with five or six FTE physicians, were more numerous than group practices in any other category, by size, for each of the four years profiled. Over this same period, the number of these small groups rose 94.2%, the greatest percentage increase, by size of practice. Long-term Care Nursing home chains continue process of market consolidation. Between 1996 and 2000, the nation’s largest nursing home chains boosted the total number of homes they operated by just over one-fourth (to 4,204 from 3,360). The number of licensed beds in these nursing homes increased comparably during this period, to 489,953 from 392,811. Overall, these largest chains operated 27.4% of all nursing homes in the nation in 2000, up from 21.9% in 1996. Meanwhile, the total number of home health care agencies dropped for the second consecutive year, to 13,067 from the 15,018 in 1998. MEDICAL GROUP PRACTICE DIGEST11 Group Practice Demographics Number of medical group practices surpasses 10,000. In 2000 the number of medical groups practice nationwide with five or more FTE physicians climbed 10.9% to 10,113 from 9,123 in 1999. Growth was greatest (13.2%) among the smallest practices (those with five or six FTE physicians); the number of these increased to 4,366 in 2000 from 3,858 in 1999. The smallest groups accounted for 43.2% of all medical group practices nationally. Medical Group Practices Defined A medical group practice is a formal and legally recognized organization that consists of three or more physicians who are engaged in the practice of medicine, sharing business management, facilities, records and personnel. Full-time-equivalent (FTE) clinical care physicians work at least the minimum number of hours that the group practice considers to be a normal work week (or 1.0 full-time-equivalent). Within this formula, a clinical are physician working half of this minimum number of hours would account for 0.5 FTEs, etc. The number of FTE physicians in medical group practices reached 141,283 in 2000, up 7.3% from 132,124 in 1999. Of this total, 74,207 (52.3%) practiced in groups with 20 more physicians. The number practicing in the smallest groups (five or six physicians) climbed 13.2%, the largest percentage rise in 2000, by size category. MGMA DEMOGRAPHICS MGMA has broad spectrum of members in 2001 It had 17600 members from 9,392 health care organizations, 6,838 of which were medical practices staffed by 150,632 FTE physicians. The 2,554 non-medical practice organizations included hospitals, integrated delivery systems, HMOs, management service organizations, practice management companies and other organizations involved in the management of physicians and medical group practices. California had 377 MGMA medical practices and 19,918 physicians practicing in them. In contrast, Wyoming had 16 MGMA medical practices and 126 physicians practicing in them. Distribution of MGMA medical practices by region: Southern – 2,158 (31.6%); Eastern -1,873 (27.4%); Midwestern – 1,494 (21.8%); Western – 1,313 (19.2%). Distribution of MGMA medical practice physicians by region: Southern – 37,412 (24.8%); Eastern – 42,671 (28.3%); Midwestern – 33,867 (22.5%); Western – 36,682 (24.4%). Physicians own majority of MGMA medical practices 56.7% in 2001. A total of 63,224 FTE physicians (41.9% of all MGMA physicians) were part of these practices. Universities and/or medical schools owned just 2.0% of all MGMA practices, but these institutions had more than a fifth (21.0%) of all FTE physicians in MGM<A medical practices. CAPO DEMOGRAPHICS Largest organizations have 25.8% of physicians At midyear 2001, 25.8% of all physicians in reporting California Association of Physician Organization (CAPO) practices were in organizations with more than 750 physicians. These largest organizations made up just 6.3% of all CAPO in 2001. By comparison, organizations with fewer than 100 physicians accounted for 10% of all CAPO organizations and 1.6% of all physicians. Midsize groups have largest percentage of MDs. Of reporting CAPO-member physician organizations in 2001, the greatest share of physicians (36.5%) practiced in organizations with 251 to 500 physicians. Physician organizations of this size accounted for nearly a third (32.5%) of all reporting physician organizations. PHARMACY RISK Smaller percentage of organizations assume Rx risk. Of 15 reporting CAPO-member physician organizations, nine (60%) contracted with health plans to assume financial risk for commercial and Medicare pharmacy benefits in 2000. These organizations underwrote a total of 80 full- or partial-risk contracts. In 1999, 78.9% of reporting CAPO organizations took on financial risk for commercial pharmacy benefits; 63.9% did so for Medicare pharmacy benefits. CAPO organizations post commercial Rx risk gains Commercial pharmacy expenses per member per month (PMPM) on risk contracts for reporting CAPO-member organizations were $14.57 PMPM funding target. As a result these organizations reported a net surplus of $0.48 PMPM, or $498,712 per organization. Medicare + Choice pharmacy risk contract expenses PMPM were $43.65, 22.5% more than the funding target. Reporting CAPO physician organizations posted an actual deficit of $3.19 PMPM on Medicare + Choice pharmacy risk contracts in 2000, which translated to a net per entity loss of $559,639. However, this actual PMPM improved from the $9.70 PMPM loss in 1999. Medicare + Choice pharmacy risk contract costs PMPM fell 18.1% in 2000, to $43.65 from $53.27. A small number of reporting CAPO physician organizations with therapeutic support systems (TSSs) achieved, on average, gains of slightly more than $900,000 on commercial pharmacy risk contracts. This appearance of success, however, was tempered by an average deficit of nearly $830,000 on Medicare + Choice pharmacy risk contracts for the small number of reporting CAPO physician organizations that used TSSs. (The TSS consisted of a pharmacy and therapeutics or formulary committee, a staff or consultant clinical pharmacist, and a preferred rug list or formulary). Number of Rxs PMPM per Medicare contract climbs The average number of prescriptions PMPM on Medicare + Choice pharmacy risk contracts undertaken by reporting CAPO physician organizations rose 4.4% in 2000, to 1.91 from 1.83 in 1989. The average cost per prescription on these contracts increased 6.7%, to $31.77 from $29.77. For commercial contracts, the average cost per prescription climbed 14.1%, to $31.41 from $27.52 in 1999. Commercial Rx contracts often include rebates Two-thirds, or 66.7%, of commercial pharmacy risks contracts with CAPO physician organizations included provisions to share rebates with health plans, up from 51.6% in 1999. By comparison, 63.2% of Medicare + Choice pharmacy risk contracts contained rebate-sharing provisions, down from 71.4% the previous year. CAPO organizations report pharmacy risk deficits Average PMPM expenses on commercial contracts at reporting CAPO medical groups and independent practice associations (IPAs) were less than the PMPM funding targets. As a result, medical groups achieved an average PMPM net surplus of $1.29, while IPAs posted, on average, a net surplus of $0.54. For medical groups, the PMPM surplus translated to $1,186,543 per organization. UTILIZATION REVIEW Utilization review is common among American Medical Group Association (AMGA) groups Of 106 reporting AMGA group practices in 2001, 72.6% had pharmacy utilization programs (data not provided). Of the groups that reported utilization review, 60.3% assumed full responsibility for the review process. Among groups categorized by number of FTE physicians, the largest groups (151 or more FTE physicians) were most likely (74.3%) to assume complete utilization review responsibilities. Utilization review partnerships are most common in the Northeast Among AMGA medical groups categorized by regions, those in the Northeast were most likely (45.5% or reporting groups) to share responsibility for pharmaceutical utilization review with one or more outside organizations. Groups in the Northeast were also more likely to use utilization review than were groups in other regions. More than nine of ten groups in this region undertook partial of full responsibility for utilization review. Utilization review is least common in the Southeast region Among reporting groups, those in the Southeast region were least likely (52.9%) to have utilization review programs. Of groups in the Southeast that reported using utilization review, twothirds took full responsibility for the process. Utilization review process frequently involves 10 or fewer users Among those AMGA medical group practices that undertook responsibility for pharmacy utilization review in 2001, slightly more than 60% involved one to ten users in the review process. Among multi-specialty groups that reviewed pharmacy utilization in 2001, 63.5% used 10 or fewer reviewers, while 36.5% of multi-specialty groups involved 11 or more users in the utilization review process. Outsourcing of utilization review responsibilities is rare for groups Of those groups that did not assume responsibility for in-house review of pharmaceutical utilization, no more than one in seven in any region profiled outsourced the job of reviewing pharmaceutical utilization. In the Northeast and Southwest regions, respectively, 14.3% of reporting groups outsourced utilization review to another organization. No groups in the Southeast reported outsourcing this task. MEDICAL GROUP LEADERS SPEAK OUT On the Limits of Providing Care “At some point, medical groups are going to have a discussion about where the boundaries are for the kind of health care or medicine that they practice. Some groups are going to want to get into everything, while other groups are going to have to restrict themselves to taking care of sick people and they’ll probably be all over the spectrum in their answers.” “But could it be that, as time goes non, people in health care institutions are going to have to think about where the boundaries are in terms of what they participate in? Do they get involved in wellness centers? Do they get involved in nursing homes? Do they get involved in hospitals? Traditional medicine, alternative medicine?” On Successful Strategies for Controlling Costs “The most successful cost-saving strategies without question begin with information sharing. Until everybody’s on the same page about what a cost is, you really can’t get anywhere. The first strategy in our institution has been to let people understand what the information is in terms what costs truly mean, why they are rising, and how we define them. We define the quality of care very carefully, so we aren’t going to sacrifice quality care to reduce costs. And we’ll do everything in our power to find other areas in which to reduce cost without that sacrifice. Aligning our incentives and having responsibility directed to those people who could make the change, whether that be in DRUGS (lecturers’ emphasis), length of stay or implementing best practices, has been effective. We’ve looked at defining cost per encounter. I think some practices have benefited from understanding the power of a group purchasing model. Technology is one of those areas that can either increase or save costs. We’re pushing a lot on electronic eligibility and electronic claims because the data shows that if we can do these better, our staff can be more productive or we might even need less of them.” On Baby Boomers and increasing Medical Utilization on Pharmaceuticals and the Cost of Care “We haven’t even begun to feel the impact of Baby Boomers on health care utilization. As we have more health care needs, we’re going to expect to have them addressed. Quality of Life is more important. Baby Boomers feel more entitled to demand it than the generation before them. We seek treatment for conditions that previous generations might have ignored.” “There is no doubt that DRUGS (lecturers’ emphasis) do reduce the cost of care. But, in a capitated environment, over the last three or four years it’s been a challenge. If we are getting paid to take care of patients and we are not at full risk for the pharmaceutical costs, and the patients are taking their medications, there is no question that these drugs are having a significant impact on the cost of care. And since no matter how you slice it, reducing and avoiding admissions are significant cost savers, clearly some of these drugs are having an impact.” “But, if you’ve been at risk for drugs, you’ve probably been losing money. It’s a very difficult question. Drugs today are far better than drugs were five years ago and tremendously better than drugs were ten years ago. With that, one should expect that prescription drug costs, as an absolute number, are going to increase. But I don’t think physician groups should take risks on prescription drugs. And if they can, they should be carve-outs.” On The Future of Managed Care “The future of managed care depends on what you mean by managed care. Are you defining it as capitation, as a different form of payment, or just managing cost? There are many ways of looking at managed care and defining it. And the work venue in which you work, whether it be outpatient or inpatient, will contribute a little to determine your success as well.” “But if you look at the utilization of antibiotics as an example, where they may not be any financial incentive but a better incentive for quality of care, managed care can help. In this instance, managed health care personnel share information both in terms of what outcomes are and whether other multidisciplines bring to the utilization equation.” “And as a urologic surgeon, for example, work closely with infectious diseases. Part of my group may help me “manage” the best antibiotics and utilize the whole concept of drugs in a better, more efficient fashion.” AFTERWORD Groups seek stability to take on market challenges Medical groups face difficult challenges in an ever-competitive health care environment. Maintaining financial stability, in part by controlling costs, demands expensive investments in information technology, a tall order unless physicians’ share of the health care dollar remains stable. Groups will also seek new ways to deliver care to an aging population asking for high-quality affordable care. Groups face new health care world Medical group practices, particularly those in areas heavily penetrated by managed care, saw big changes in the health care world during the late 1980s and most of the 1990s. Managed care organizations used capitation to shift risk from themselves to physicians. Utilization rates fell, but in states with large managed care presence, so too did the compensation for many physicians. Some medical groups were unable to stay afloat. Worries about cost have not gone away, however. Consumers now are demanding access to an array of life-prolonging technologies and pharmaceuticals. Groups now must negotiate managed care contracts that protect their revenue and ensure the capital to finance equipment investments. Taking on risk prudently may offer some groups a share of the pharmaceutical dollar. Assuming Rx risk offers both opportunities and dangers With the overall costs of pharmaceuticals increasing, many medical group practices have shied away from taking on full risk for pharmacy benefit contracts negotiated with managed care organizations. CAPO-member organizations responding to a pharmacy risk survey undertook a total of 80 commercial and Medicare pharmacy risk contracts, but just three were full risk, while the remainder required that the physician organization take no more than 50% of the risk. Some medical groups undeniably have lost great amounts of money in assuming risk for pharmacy benefits. However, evidence exists that groups can assume pharmacy risk and still profit, particularly on commercial HMO members. For example, the 42 commercial benefit risk contracts analyzed in the CAPO risk survey produced a median surplus per member per month (PMPM) of $0.65, good for $96,287 per pharmacy contract. Medical groups unwilling to take on full risk can negotiate contracts that pay flat rates or that yield a percentage of premium. So-called tiered benefit plans shift risk to the patient. The CAPO survey revealed that a very small percentage of the physician organizations surveyed agreed to globally capitated contracts, which put physicians at greatest risk of economic loss. HMO-PPO/MEDICARE-MEDICAID DIGEST12 The HMO-PPO/Medicare-Medicaid Digest provides an overview of the managed care industry in a single, comprehensive resource that reports of HMOs, PPOs, and Medicare/Medicaid managed care.This Digest monitors trends, establishes benchmarks and identifies opportunities for managed care organizations. HMO Industry Summary Consolidation reduced the number of licensed, individual HMOs operating in the U.S. by 23.8% in 2000, to 625 from 820 in 1999. However, the total HMO enrollment fell just 5.1%, to 99.3 million from 104.6 million the year before. HMO penetration declined to 35.3% of the U.S. population in 2000 from 37.9% in 1999. The 25 largest individual HMOs enrolled 33.9 million members, up from 30.6 million in 1999. Enrollment in these HMOs accounted for 34.2% of all HMO members nationally. Thirty-seven corporate HMOs enrolled 85.9 million members (up from 82.6 million in 1999), or 86.5% of HMO enrollment nationwide. HMOs affiliated with a total of 4,384 physician providers per plan in 2000, up 14.0% from 4,384 physician providers per plan in 2000, up 14.0% from 3,844 in 1999. The number of PCPs per plan rose 16.8%, to 1,421 from 1,217 the previous year, while the number of specialists grew 11.6%, to 2,963 per plan from 2,656. Enrollment in point-of-service (POS) plans grew 5.2% in 2000, to 19.4 million members from 18.5 million in 1999. IPA-model HMOs continued to enroll a notably higher number of members in POS plans than other HMO types in 2000, with 12.l million, or 62.5% of total POS enrollment. The share of HMOs using fee-for-service to compensate physicians rose overall in 2000 (to 88.6% from 83.7% in 1999) and in every HMO category. For the second straight year, the share of HMOs using capitation to pay physicians grew significantly, to 81.5% from 76.7% the previous year. Of the 625 HMOs in 2000, 421 (67.4%) were IPA-model plans (by far the highest share by model type), 118 (18.9%) were network-model plans and 67 (10.7%) were group model plans. The number of hospital days and hospital admissions per 1,000 Medicare HMO members fell in 2000. Average length of stay (ALOS) for Medicare HMO members was unchanged. More than a third of all HMOs are 15 years old or older. The percentage of licensed HMOs 15 years of age or older was 34.4% in 2000, up notably from 23.3% in 1999 and the highest share by age. HMOs that were 10 to 14 years of age accounted for 20.2% of all HMOs, down from 27.4% the previous year and the lowest percentage by age. Older HMOs are most likely to offer POS plans. The share of HMOs 10 to 14 years of age that offered point-of-service (POS) plans was 73.0%, up from 62.7% in 1999 and the highest share by age. By comparison, the share of HMOs under five years old offering POS plans was 41.8%, up fractionally from 41.6% in 1999 and the lowest share by age. HMO Pharmacy Summary Average premium rates per month rose 2.4% for individuals, to $159.71 from $155.93 in 1999, and 2.5% per family, to $462.48 from $451.42 the previous year. Between 1999 and 2000, the average co-payment per prescription climbed 42.7% for formulary brand name drugs and 31.3% for non-formulary brand name drugs. By comparison, the average copayment requirements for generic drugs increased 11.5% from the year before. The share of reporting HMOs using physician withholds or risk pools dropped in 2000, to 15.3% from 22.7% in 1999. Of HMOs that used formularies in 2000, 53.5% used the largest formularies of 1,000 or more drugs, a slight percentage decline from 54.6% in 1999. The percentage of HMOs that used drug formularies was 99.0%, up from 96.9% in 1999. However, formularies developed by PBMs were the controlling document at 17.5% of these HMOs, down substantially from 25.0% the previous year. Average overall HMO drug expenditures PMPY increased 19.6%, to $243.42 from $203.52 in 1999. Pharmaceutical expenditures accounted for 13.4% of total HMO operating costs in 2000, unchanged from 1999. The 37.6% of HMOs with in-house pharmacies employed an average of 27.2 pharmacists in 2000, down notably from an average of 30.7 the year before. The share of HMOs that contracted with retail drug chains for pharmacy services climbed to 84.4% from 70.1% in 1999. Meanwhile, the share of HMOs that contracted with PBMs to handle prescription services increased to 94.9% from 90.1% The share of HMOs that covered OTC medications rose sharply, to 29.0% from 12.3% in 1999. The share of HMOs that required generic substitution when generic products were available grew to 82.1% in 2000 from 76.9% in 1999, while the share of HMO members subject to generic substitution increased to 85.2% from 82.4%. Drug costs share of total operating costs holds steady. Pharmaceutical expenditures as a percentage of total HMO operating costs was 13.4% in 2000, unchanged from 1999 HMOs under five years of age reported that drug costs accounted for 14.3% of total operating costs in 2000, up from 13.8% in 1999 and the highest percentage by HMO age. PHARMACY BENEFIT STRUCTURE Nearly all HMOs offer outpatient prescription benefits The overall share of HMO plans that offered outpatient prescription benefits was 99.8% in 2000, compared to 98.8% in 1999. However, the share of HMO enrollees covered by prescription benefits declined slightly, to 93.0% from 94.1% the previous year. Meanwhile the share of HMOs with no deductible for prescription drugs declined for the second consecutive year, to 94.8% from 95.7% in 1999. HMO benefit coverage of certain prescription drugs dips HMOs were less likely in 2000 than in 1999 to include in their pharmacy benefit programs prescription drugs that fell into the four categories of experimental drugs, cosmetic aids, smoking cessation drugs and fertility drugs. However, HMOs were more likely than the previous year to cover in their pharmacy benefit programs prescription drugs included in the two categories of anorexiants and oral contraceptives. Co-payments on formulary brand name drugs climb The average co-payment per prescription on formulary brand name drugs jumped 42.7% in 2000, to $12.90 from $9.04 in 1999. On average, this co-payment covered 27.4% of the prescription cost, a moderate increase from 25.4% the previous year. By comparison, the average co-payment for nonformulary brand drugs was $22.97 (up 31.3% from $17.50 in 1999), or 39.9% of the prescription cost. Meanwhile, the average co-payment for generic drugs rose 11.5%, to $6.67 from $5.98 the year before. Share of HMOs that cover OTC medications jumps The share of HMOs covering over-the-counter (OTC) medications increased sharply, to 29.0% from 12.3% in 1999. Of the model types, the share of IPA-model HMOs that covered OTC medications rose most notably, more than tripling to 30.7% from 9.1% the previous year. The share of staff-model HMOs covering OTC medications climbed to 31.3% from 19.0% in 1999, while the network-model HMO share grew to 27.6% from 20.5%. Drug coverage of IPA-Model HMOs trail others Except for cosmetic aids and oral contraceptives, IPA-model HMOs were less likely than HMOs of other model types to cover in their pharmacy benefit programs prescription drugs from every category profiled. By comparison, staff-model HMOs were more likely than HMOs of other model types to cover in their pharmacy benefit programs three categories of prescription drugs (experimental drugs, anorexiants and rugs for smoking cessation). Newest HMOs cut prescription drug coverage in 2000 The share of HMOs less than five years of age that included certain drugs in their pharmacy benefit programs dropped sharply from the year before in two categories: experimental drugs (down to 2.4% from 7.4%) and cosmetic aids (down to 1.2% from 6.7%). Drugs sometimes excluded from pharmacy benefit programs DESI (Drug Efficacy Study Implementation) drugs are drugs that were reclassified by the FDA in 1962 as proven safe but not fully efficacious under today’s regulations; Diabetic Supplies; Fluorides; Growth Hormones; OTC Drugs; Prenatal Vitamins; Hair Growth; and Self-administered Injectables. Note: DESI (Drug Efficacy Study Implementation) drugs are drugs that were re-classified by the FDA in 1962 as proven safe but not fully proven efficacious under today’s regulations. Coverage is sometimes extended to some categories of DESI drugs that have undergone some tests for efficacy, but DESI drugs are usually excluded. PHARMACY BENEFIT PREMIUMS HMOs boosts premiums for outpatient pharmacy benefits HMO premiums PMPM for outpatient pharmacy benefits increased 8.5% for individuals (to $18.91 in 2000 from $17.43 in 1999) and 1.6% for families (to $44.00 from $43.32). Although their rates continued to be lowest by HMO model type, staff-model HMO plans raised individual premiums 10.00% to $13.27 from $12.06 in 1999, and 14.5% for family premiums to $35.51 from $31.02, the most by each model type. DRUG UTILIZATION REVIEW Share of HMOs with drug utilization review increases The percentage of reporting HMOs that had formal drug utilization review (DUR) programs continued to rise in 2000, to 96.2% from 93.9% in 1999 and from 92.6% in 1998. Enrollment in HMOs that used DUR programs was 90.7 millions or 97.4% of enrollees in all reporting HMOs. In 1999 by comparison, HMOs with DUR programs had 91.5 million members, representing 97.6% of enrollees in all plans. PHARMACY UTILIZATION Average number of prescriptions by HMOs increases The average number of prescriptions dispensed per non-Medicare HMO member per year rose 5.6% in 2000, to 7.5 from 7.1 in 1999, while the average number of Medicare members increased 5.5% to 19.1 from 18.1. In 2000, network-model HMOs dispensed the most prescriptions per member per year (PMPY), model type, for non-Medicare (7.7) and Medicare (19.7) members alike. PHARMACY AND PHYSICIAN CONTROLS Share of HMO plans using financial incentives drops The share of HMOs that used financial incentives to influence physician prescribing practices declined considerably in 2000, to 23.1% from 39.3% in 1999. HMO use of practice guidelines to influence physician prescribing practices also fell, to 70.6% from 73.2% the previous year. In 2000, 73.7% of HMOs influenced prescribing patterns through quality assurance methods, down from 74.8% in 1999. PHARMACY PROVIDERS Use of contract pharmacies by HMO plans increases Contract pharmacies were used for prescription services by 94.8% of HMOs in 2000, up from 92.8% in 1999. By comparison, the percentage of HMOs that offered members prescription services through in-house pharmacies declined slightly, to 36.0% from 37.0%, the previous year. The percentage of HMOs offering in-house pharmacies only was virtually unchanged from the year before, at 2.7% HMO plans often use retail drug chains for Rx services The share of HMOs contracting with retail drug chains for pharmacy services rose significantly in 2000, to 84.4% from 70.1% in 1999. Similarly, 94.9% of HMOs contracted with pharmacy benefit managers (PBMs) to handle prescription services, up from 90.1% the previous year, while the percentage of HMOs contracting with independent pharmacies increased to 64.7% from 61.9%. Share of HMOs using mail-service (mail order pharmacy) plans hold steady The share of HMOs that used mail-service pharmacies was 82.8% in 2000, virtually unchanged from 82.7% in 1999. IPA-model HMOs were once again the model type most likely to use mailservice pharmacies, although the share that did so fell to 85.9% from 87.4% the previous year. Staffmodel HMOs were again least likely to use mail-service pharmacies, but the share that did so climbed to 58.8% from 32.0% in 1999. Largest HMOs use mail-service pharmacies most HMOs with 250,000 or more members were most likely, by membership size, to use mail-service pharmacies, and the share that did so rose to 91.8% from 87.5% in 1999. Conversely, HMOs with 15,000 or fewer members were least likely, by membership size, to use mail service plans, and the share that did so fell to 72.4% from 74.8% the previous year. Meanwhile, HMOs nine years of age or younger were, in general less likely to use mail-service pharmacies in 2000 than plans 10 years of age or older. FORMULARIES Nearly all HMO plans use drug formularies in 2000 The percentage of HMOs that used drug formularies was 99.0% in 2000, up from 96.9% in 1999. For the third consecutive year, all staff-model HMOs used drug formularies, as did, for the first time, all IPA-model HMOs. For the sixth straight year, drug formularies were used by all corporatemanaged HMOs. In 2000, all corporate-affiliated and hospital-owned HMOs used drug formularies as well. All of the largest HMOs use drug formularies in 2000 All HMOs with 250,000 or more members used formularies in 2000, up from 98.9% in 1999. Similarly, all reporting HMOs with 100,000 to 249,999 members used formularies, compared with 98.8% the previous year. The share of HMOs with fewer than 15,000 members that used formularies was 97.3%, up from 92.6% in 1999. The share of HMOs using formularies rose between 1999 and 2000, regardless of HMO size. Fewer HMOs use drug formularies developed by PBMs Formularies developed by pharmacy benefit managers (PBMs) were the controlling document at 17.5% of HMOs that used formularies, down substantially from 25.0% in 1999. Similarly, proprietary formularies were the controlling document at 59.1% of HMOs using formularies, a notable decrease from 67.2% the previous year. Modified PBMs were the controlling pharmaceutical formulary at 13.4% of HMOs using formularies. Share of Rxs filled within formulary rises slightly HMOs with formularies indicated that 89.7% of member prescriptions were filled using formulary drugs, up fractionally from 89.0% in 1999. At 93.1%, staff-model HMOs had the highest share, by model type, of prescriptions filled within formularies. Meanwhile, independently owned HMOs had 93.0% of member prescriptions filled within approved formularies, the greatest share by owner type. About half of HMOs used closed drug formularies Of HMOs that employed formularies, 49.6% used closed formularies, up fractionally from 49.4% in 1999. Not-for-profit HMOs (52.1%) were more likely to follow closed drug formularies than forprofit HMOs (48.4%), a revcrsal from the previous year. NOTE: An open formulary allows prescribers to use non-formulary drugs without penalty. A closed formulary commonly requires pre-authorization of non-formulary drugs and sometime involves a financial penalty for the physician and/or the patient. HMOs with closed formularies, particularly staff-model HMOs, often cover non-formulary drugs by exception. 81% of HMOs use formularies with 750 or more drugs Of HMOs that used formularies in 2000, 80.9% had approved drug lists that contained 750 or more drugs, up from 79.8% in 1999. More than half of all HMOs, or 53.5%, used the largest formularies of 1,000 or more drugs, down slightly from 54.6% the previous year. Meanwhile, the share of HMOs that used formularies with fewer than 500 drugs increased, to 10.4% from 10.2% in 1999. Share of HMOs reviewing formularies annually grows The share of HMOs that reviewed their drug formularies on an annual basis increased to 25.1% from 17.5% in 1999. Formularies were reviewed quarterly by 39.3% of HMOs, up notably from 35.1% the previous year. At 28.7%, IPA-model HMOs were most likely, by model type, to review drug formularies annually; at 53.5%, a network-model HMO plans were most likely to conduct quarterly reviews. Share of PBMs serving on drug committees slips Pharmacy benefit managers (PBMs) were named as members of drug formulary committees by 46.1% of HMOs down from 51.9% in 1999. Similarly HMO administrators were members of formulary committees at just 22.6% of HMOs, a significant drop from 30.5% the previous year. Other members of the formulary committee mentioned by HMOs were pharmacy directors, laypeople and outside pharmacy consultants. GENERIC SUBSTITUTION Share of HMOs requiring generic substitution swells The share of HMOs that required generic substitution when generic products were available rose substantially in 2000, to 82.1% from 76.9% in 1999. In consequence, the overall percentage of HMO members subject to generic substitution increased to 85.2% from 82.4% the year before. Corporateaffiliated HMOs required generic substitution for 94.8% of their members, up from 86.6% in 1999. Share of HMOs allowing choice of brand name Rxs dip The share of HMOs permitting members a choice between generic and brand name drugs dipped in 2000, to 95.3% from 95.8% in 1999. IPA-model HMOs were more likely than plans of other model types to permit members this option, but the share that did dropped from 96.9% from 97.5%. The share of HMOs with in-house pharmacies allowing members the option of brand name drugs decreased to 92.5%from 95.7% in 1999. THERAPEUTIC INTERCHANGE Share of HMOs allowing therapeutic interchange rises The share of HMOs allowing therapeutic interchange (the substitution of a therapeutically equivalent drug for the one prescribed) increased substantially in 2000, to 44.6% from 37.5% in 1999. Of the model types, the share permitting therapeutic interchange was highest among group-model HMOs (to 57.6% from 35.6% the previous year) and lowest among IPA-model HMOs (to 39.2% from 35.2%. DRUG-STEP THERAPY Share of HMOs using step-therapy continues to rise Pharmaceutical step-therapy procedures were in place at 74.7% of HMOs in 2000, up from 70.4% in 1999. Step-therapy is a prescription pattern based on the stage of illness; the drug believed to be the most cost-effective is used first. Corporate-managed HMOs were most likely to use step-therapy in 2000 (100.0%), whereas independent HMOs were least likely to do so. Share of HMOs with step-therapy at the pharmacist level plummets Of HMOs using pharmaceutical step-therapy, the overall share implemented through pharmacists dropped dramatically to 32.8% from 58.1% in 1999. The share of HMOs that initiated step-therapy through physicians also declined significantly, to 87.8% from 93.4% the previous year. In 2000, HMOs 10 to 14 years of age were most likely, by age category to allow physicians (92.4%) and pharmacists (35.9%) to initiate step-therapy. DRUG EXPENDITURES Annual drug expenses per member for HMOs increases Median overall HMO drug expenditures PMPY climbed 19.6% in 2000, to $243.42 from $203.52. IPA-model HMOs had the highest median drug expenses by model type, at $274.64, up 29.1% from $212.70 the previous year. Median drug costs were $274.44 PMPY at corporate owned HMOs in 2000, an increase of 27.9% from $214.54 in 1999 and the highest median cost by ownership type. DRUG PURCHASING Share of HMO pharmacies using GPOs (Group Purchasing Organization) decreases Of the 37.6% of HMOs with in-house pharmacies 80.4% bought pharmaceuticals through GPOs in 2000, down from 83.3% in 1999. By comparison, the share of HMOs that purchased pharmaceuticals from prime vendors or wholesalers rose to 35.3% from 32.6% the previous year, while 32.0% bought pharmaceuticals through contract bids, a slight drop from 33.0%. More HMOs with no pharmacies are in rebate programs The share of HMOs without in-house pharmacies that participated in pharmaceutical manufacturer rebate and charge-back programs climbed to 95.1% from 81.5% in 1999. By comparison, the share of HMOs with in-house pharmacies that participated in these programs grew to 92.4% from 91.7% the year before. Overall, the share of HMOs that participated in rebate and charge-back programs rose notably, to 94.15 from 85.5% in 1999. HMO AFTERWORD Enrollment in licensed, operating HMOs decreases Total enrollment in HMOs nationwide fell by just over 5% between 1999 and 2000, the first such drop since this digest began tracking membership in 1987. In accordance, the HMO market penetration rate fell nationally (2.6 percentage points) and across all eight regions. Intense media scrutiny of the managed care industry and the passage of numerous managed care reform laws have contributed to this trend. Co-payments on formulary brand name drugs grow Average co-payment requirements for outpatient prescriptions continued to rise dramatically between 1999 and 2000 across all components of the three-tier pharmacy benefit. In this period, the average co-payment per prescription jumped nearly 43% on formulary brand name drugs. By comparison, the average co-payment for generic drugs rose a comparatively slight 11% from the previous year. HMO drug plans are commonly structured to encourage the use of lower-cost generic drugs when members purchase prescription drugs. Indeed, HMOs go to great lengths to increase the percentage of prescriptions filled with generics instead of brand name drugs. Generic drugs account for 40% of all outpatient prescriptions, approximately the same percentage as in 1995, and make up about 9% of total prescription drug sales, down from more than 12% in 1995. Growth in HMO enrollment and Rxs dispensed has an impact on pharmacist role The sustained increase in the number of prescriptions dispensed PMPY over the past decade has contributed to growing concern about the availability of pharmacists to fill vacant pharmacy positions and intensified scrutiny of pharmacy operations. Between 1999 and 2000, the average number of prescriptions dispensed PMPY rose 5.6% for non-Medicare (commercial) HMO members. Meanwhile, the approximately 38% of HMOs with in-house pharmacies (to cite one point of access to pharmaceutical services) employed an average of 11% fewer pharmacists in 2000 (27.2) than the previous year (30.7). A number of recent studies have suggested that, as a consequence, pharmacy functions have diminished some in traditional areas and increased in new areas. The reallocation of pharmacy resources was especially evident in the model types in which pharmacy activities were comparatively greater. Among the efforts to stabilize the pharmacy service role is legislation in Congress currently under consideration to recognize pharmacists as health care providers and allow them to bill for services. MEDICARE/MEDICAID INDUSTRY SUMMARY Overall Medicare HMO enrollment growth, which had been slowing steadily since the midnineties, reversed itself in 2000. Of the nation’s 39.9 million Medicare beneficiaries in 2000, 6.7 million (16.8%) were enrolled in licensed HMOs down from 6.8 million (17.2%) in 1999. Of these 35.9% were covered by Pacific region plans. Pharmacy costs accounted for 11.1% of total operating expenses for HMOs that enrolled Medicare beneficiaries, down from 13.3% in 1999. Between 1999 and 2000, the number of hospital days per 1,000 Medicare members, number of physician encounters per Medicare HMO member and Average Length of Stay (ALOS) per hospital admission fell. HMOs enrolling Medicare beneficiaries has 11.9 PCPs per 1,000 HMO members, up 17.8% from 10.1 in 1999. The number of specialists for these HMO plans increased to 25.8 from 25.0 the previous year. Expenditures for Medicare beneficiaries covered by MCOs ($39.8 billion) accounted for 18.5% of all Medicare benefit payments ($214.9 billion) in 2000, up from 17.9% in 1999. The total number of Medicaid recipients in Managed Care organizations (MCOs) rose 5.0% in 2000, to about 18.0 million from 17.1 million in 1999. Of these, 11.5 million (63.9%) were enrolled in HMO plans. The number of hospital days per 1,000 Medicaid members in HMOs dropped again, to 392 days from 398 in 1999. Medicare HMO enrollment dips Enrollment of Medicare beneficiaries in HMO plans dropped fractionally in 2000, to 6.7 million from 6.8 million in 1999. Meanwhile, MCOs enrolled 18.0 million Medicaid recipients, a 5.0% rise from 17.1 million enrolled the previous year. MEDICARE PHARMACY Medicare HMO Rx cost part of operating expenses drop Pharmacy costs accounted for 11.1% of total operating expenses in 2000 for HMOs that enrolled Medicare beneficiaries, down significantly from 13.3% in 1999. This ratio was considerably higher for proprietary HMOs with Medicare beneficiaries (12.7%) than for not-for-profit HMOs with these members (10.0%). HMOs overall has 19.6 prescriptions per Medicare member per year PMPY), up from 19.1 PMPY in 1999. MEDICAID DEMOGRAPHICS Enrollment in Medicaid MCOs approaches 18 million The total number of Medicaid recipients enrolled in managed care nationwide increased 5.0% in 2000, to just under 18 million from 17.1 million in 1999. Of these Medicare MCO members, 11.5 million (63.9%) were enrolled in licensed HMOs. California enrolled more than 2.5 million Medicaid recipients in HMOs, considerably more than any other state. Three other states – Florida, Michigan and Tennessee – had in excess of 1 million Medicaid recipients in MCOs. Tennessee had 1.3 million Medicaid MCO members, all of whom, for the third straight year, were enrolled in HMOs. Meanwhile, Georgia again, had the highest number of enrollees in Primary Care Case Management Programs (PCCMs), at 603,438, or 13.2% of the 4.6 million Medicaid recipients in PCCMs in 2000. MCOs in every state but two enroll Medicaid recipients At midyear 2000, MCOs in 48 states and the District of Columbia enrolled Medicaid recipients; only Alaska and Wyoming reported no such enrollment. HMOs in 40 states and D.C. enrolled Medicaid recipients in 2000, compared with 43 states and D.C. in 1999. Of the nation’s 33.5 million Medicaid recipients, 1.7 million (5.2%) were enrolled in Prepaid Health Plans (PHPs); just over twofifths of these were in Washington (352,614) and Michigan (351,402). South Central Medicaid HMO enrollment increases South Central MCOs enrolled 3.5 million Medicaid recipients in 2000, second most of the eight regions and 12.8% more than the 3.1 million in 1999. By comparison, MCOs in the Pacific region enrolled 3.8 million Medicaid recipients, the most by region for the fourth consecutive year, and up slightly from 3.7 million in the year before. New England MCOs had the smallest number of Medicaid members (1.0) million. Three states have high HMO and Medicaid penetrations Of the 10 states with the highest HMO penetration of their total populations in 2000, three – Oregon (seventh), Utah (eight) and Tennessee (tenth) – were also listed among the top 10 leaders in MCO penetration of the Medicaid population. Colorado, ranked thirteenth overall in HMO penetration in 2000, was also among the top 10 states in MCO penetration of the Medicaid population. 60% of Medicaid MCO members are in three regions Of the 18.0 millions Medicaid recipients enrolled in MCOs nationwide in 2000, 10.6 million (59.1%) were in the three regions – Pacific, South Central and South Atlantic. In 1999 these three regions accounted for 9.9 million (58.0%) Medicaid MCO members. Three other regions – Mountain, West North Central and New England – enrolled just 3.3 million Medicaid members (18.3%), up from 3.2 million (18.6%) the previous year. MEDICARE/MEDICAID AFTERWORD Medicare/Medicaid MCO enrollment growth continues Although the number of Medicare beneficiaries enrolled in HMOs nationwide fell slightly between 1999 and 2000, combined enrollment of Medicare beneficiaries and Medicaid recipients in HMOs and other MCOs in this period rose to 24.7 million from 23.9 million. The number of Medicare HMO members is expected to increase over the next decade, although at a significantly slower rate than was previously projected. One in four Medicare HMO members lives in California Of the nation’s 39.9 million Medicare beneficiaries in 2000, 6.7 million (16.8%) were enrolled in HMOs, compared with 6.8 million (17.2%) in 1999. Medicare HMO members remain concentrated in a few states, with nearly one in four (1.6 million) Medicare HMO members nationwide in California. Although only about one in four HMOs with Medicare beneficiaries had 250,000 or more members in 2000, these largest HMOs enrolled more than two of three Medicare HMO members (67.0%), the third consecutive year in which they have enrolled a greater majority share of these beneficiaries than in 1999. More Medicaid recipients enroll in managed care In spite of growing concern about the unwillingness of managed care organizations (MCOs) to participate in state Medicaid programs, Medicaid MCO enrollment nationwide increased 5.0% in 2000, to 18.0 million from 17.1 million in 1999. Meanwhile, the number of HMOs serving Medicaid recipients dropped to 220 in 2000 from 267 in 1998 (after steadily rising from 201 in 1995), as an increasing number of commercial plans began to exit the Medicaid market. PREFERRED PROVIDER ORGANIZATION (PPO) INDUSTRY Most PPOs continue to be insurance company-owned Insurance companies owned 553 PPOs in 2000; although this number fell from the year before , the share of all PPOs owned by these companies rose to 56.0% from 53.4% in 1999 (576 of 1,079 PPOs). Of the 988 operating PPOs, 78 were owned by hospital alliances, up from 32 the previous year. These plans accounted for 7.9% of all operating PPOs; in 1999, the hospital alliance PPO share was just 3.0% PPO industry summary Nearly all (98.8%) reporting PPOs used a managed pharmacy program in 2000, up sharply from the share reported in 1999 (83.5%) and in 1998 (79.8%). In 2000, 86.5% of PPOs used a PBM, compared with 83.7% that did so in 1999. Among these plans, 94.7% used PBMs to handle mail service and administrative services, while 93.4% relied on PBMs to process pharmaceutical claims. The percentage of PPOs using drug formularies climbed three percentage points in 2000, to 86.2% from 83.2%. Eight-nine percent of PPOs used PBMs for formulary management in 2000 up notably from 82% in 1999. Of those PPOs holding direct contracts with pharmacy providers, 67.7% offered a card program in 2000, the third consecutive year that this percentage has risen. After increasing by 35.0% between 1997 and 1999, the number of medical/surgical specialist contracts per PPO rose just 1.2% between 1999 and 2000, to 5717 from 5651. The share of PPOs holding risk contracts with providers fell to 11.4% from 24.5% in 1999. Just 7.6% of plans assumed shared-risk-only contracts, down from 19.0% the previous year. MANAGED PHARMACY PROGRAMS Nearly all PPOs have a managed pharmacy program In 2000, 98.8% of reporting PPOs used a managed pharmacy program, up more than 15 percentage points from 83.5% in 1999. All PPOs in eight of 11 ownership categories had a managed pharmacy program. The exceptions were physician/hospital joint ventures (95.7%), independent investors (93.8%) and hospital alliances (93.5%), but the percentages for all three rose from the year before. Employee number in PPO-managed Rx programs soars The number of eligibles in PPOs with a managed pharmacy program grew 54.8% to 102.5 million from 66.2 million in 1999. Insurance company-owned PPO plans had 45.4 million eligibles in such programs, up slightly more than half from 30.2 million such eligibles in 1999. PPOs over 3 years old had 98.7 million eligibles in managed pharmacy programs, up 53.2% from the 64.4 million eligibles reported by these PPO plans the previous year. Use of carve-outs by PPOs with Rx programs slips Of PPOs with a managed pharmacy program, 79.1% offered specialty services through carve-out programs in 2000, down slightly from 80.7% in 1999. Of those plans with 20,000 to 99,999 eligibles, 58.6% offered carve-outs, compared with 51.2% in 1999; this was the only category of plan, by size, to post such an increase from the year before. Carve-out programs offer specialty services to payers, usually at reduced rates. Share of plans with pharmacy benefit managers grows Overall, the share of PPOs that used a PBM continued to increase, to 86.5% in 2000 from 83.7% in 1999. Since 1995, the share has risen more than 30 percentage points. All reporting HMO-owned PPOs used a PBM, the highest share by owner type, while 98.3% of insurance company-owned PPOs and 95.7% by third-party administrator-owned PPO plans did so. Greater percentage of PPOs use formularies in 2000 Of all reporting PPOs, 86.2% used a drug formulary in 2000, up three percentage points from 83.2% in 1999 and nearly 15 percentage points from 71.6% in 1998. Insurance company-owned PPOs enrolled 38.0 million of the 56.1 million eligible employees (67.7%) in formulary-using PPOs; 97.2% of plans owned by insurance companies used a formulary compared with 92.0% the previous year. PHARMACY PROVIDERS Percentage of plans with direct pharmacy contracts falls In 2000, 70.0% of reporting PPOs had contracts with local pharmacy provider networks, down more than three percentage points from 73.2% in 1999. Despite this overall percentage slip, the share increased in six of 11 ownership categories. Plans owned by HMOs and by third-party administrators were most likely in 2000 to establish contracts with pharmacy providers (98.8% and 91.3%, respectively). Share of largest PPOs with direct Rx contracts rises Nearly 69% of reporting PPOs with 1 million or more members held direct contracts with pharmacy providers in 2000, up from just over 64% in 1999. The percentage of PPOs with 500,000 to 999,999 members that held such contracts also rose, to 78.6% from 68.8% in 1999. The share plans with direct pharmacy contracts decreased for all PPO size categories of fewer than 500,000 members. The percentage drop was most notable for plans with 100,000 to 499,999 members (to 55.1% from 67.0% the previous year). Share of youngest plans with direct contract slips Of PPOs three years old and younger, 55.9% held direct contracts with pharmacy providers, down from 62.7% in 1999, and third straight year in which a percentage decline has occurred. By comparison, the percentage of plans more than three years old that directly contracted with pharmacy providers declined, to 70.6% from 73.9% the year before, halting two consecutive years of increases. Percentage of plans with a card program moves higher The percentage of PPOs holding direct contracts with pharmacy providers and having a card program grew to 67.7% in 2000 from 66.6% in 1999, the third straight year of increase. More than 90.0% of plans in three uniquely identified ownership categories (HMOs, independent investors and third-party administrators)used card programs; for HMO-owned plans, the share fell slightly, to 96.3% from 97.1% in 1999. Share of PPOs that use mail-service still high in 2000 Of those PPOs with direct contracts with pharmacy providers, the percentage that used mailservice pharmacies was 97.9% in 2000, down slightly from 98.4% in 1999, but still by far the highest percentage of any of the four pharmacy provider categories profiled. All reporting PPOs in six ownership categories held mail-service pharmacy contracts, and at least 98.0% of plans in two other ownership categories (independent investors and insurance companies) held such contracts in 2000. Share of PPOs with local pharmacy contracts falls The percentage of PPOs directly contracting with pharmacy providers and also holding contracts with local pharmacies dipped in 2000, to 75.9% from 76.3% in 1999. Still, just three of the 11 PPO ownership categories saw a decline in the share of plans holding local pharmacy contracts (physician/medical group practices, multi-ownership and insurance companies). PPO AFTERWORD Number of PPO eligibles grows as number of plans falls Preferred provider organizations (PPOs) continued to achieve impressive growth in the number of enrolled eligible employees in 2000, even as the number of plans fell for a second consecutive year. The number of eligibles rose 4.3%, to 111.4 million while the number of plans fell 8.4%, to 988. Expect PPOs to continue to gain market share and consumers chafe against restrictions HMOs demand PPOs target pharmaceutical costs with various strategies PPOs have not been reticent to use available tools to manage pharmaceutical costs. Nearly all reporting plans used some type of managed pharmacy program in 2000; as recently as 1998, not quite 80% of PPOs did so. The percentage of plans that used pharmacy benefit managers (PBMs) rose to nearly 87% in 2000 from 54% in 1995, another indication of the effort by PPOs to manage pharmaceutical expenditures. Use of PBMs was nearly universal among insurance company-owned PPOs, which accounted for 56.0% of all plans in 2000. INTEGRATED HEALTH SYSTEMS DIGEST13 HMOs In Integrated Systems* Number of prescriptions per system HMO member rises HMOs in highly integrated systems averaged 8.3 prescriptions per non-Medicare member in 2000, up 6.4% from 7.8 in 1999, and 23.0 prescriptions per Medicare member, a 9.0% increase from 21.1. By comparison, non-system HMOs averaged 7.4 prescriptions per non-Medicare member, a 5.7% gain from 7.0 the previous year, and 18.4 prescriptions per Medicare member, a 6.7% gain from 17.3. Pharmacy expenses PMPY increase for system-tied HMOs Per member per year (PMPY) pharmacy expenses for HMOs in highly integrated systems jumped 29.8% in 2000, to $263.52 from $203.08 in 1999. Such expenses more slowly for non-system HMOs (to $278.50 from $244.77, or 13.8%), but still exceeded those of system HMOs by 5.7%. Per-Rx ingredient cost grows for system-tied HMOs The ingredient cost per prescription for HMOs in highly integrated systems rose 10.0% in 2000, to $33.52 from $30.48 in 1999. Conversely, such costs fell 7.7% during the same period for non-system HMOs, to $30.87 from $33.43. Meanwhile, pharmacy benefit premiums per system HMO member rose 8.3% (to $19.14 from $17.68 in 1999), while such premiums for non-system members increased 8.6% (to $18.87 from $17.38). Systems seek to balance Rx costs and benefits Pharmacy expenditures were one key element of the total cost equation for highly integrated systems in 2000. For example, HMOs in highly integrated systems spent nearly 30% more per member per year on drugs in 2000 than in 1999. Pharmacy expenditures consumed just over 14 cents for each operating dollar for these plans in 2000, up more than 40% from just under 10 cents in 1996. However, between 1996 and 2000, the average number of prescriptions per commercial and Medicare members is system HMOs climbed by more than 30%, respectively. Drug cost management will remain a key system goal, but equally important will be efforts to assess through data gathering and analysis to role of drugs in lowering overall medical costs. *HMOs are considered to be in integrated health systems if they are part of a system by virtue or ownership or or contractual arrangements. HMOs are not considered to be in integrated systems if they hold only provider network contracts with systems. INSTITUTIONAL DIGEST14 Multi-hospital System (MHS) Pharmaceutical Expenses Pharmaceutical expenses rise at selected MHSs Between 1999 and 2000, pharmaceutical expenses per discharge and per staffed rose for hospitals in each of three multi-hospital system ownership categories. The increases were most notable for facilities in 12 government MHSs, in which pharmaceutical expenses per discharge climbed 7.7%, to $463 from $430 in 1999, while such expenses per staffed bed grew 4.5%, to $13,959 from $13,354. Per-discharge Rx expenses increase for MHS hospitals Pharmaceutical costs per discharge grew just 2.6% overall for multi-hospital system hospitals, to $349 from $340 in 1999. For non-MHS hospitals, such costs also rose moderately to $370 from $359 the previous year. Facilities in for-profit MHSs held these expenses to $330 in 2000, up only fractionally from the $327 for hospitals in eight of these systems reported the previous year. Pharmaceutical costs per bed rise for MHS hospitals Hospitals in MHS paid pharmaceutical expenses of $12,473 per staffed bed in 2000, up 9.8% from $11,355 in 1999. By comparison, non-MHJS facilities spent $9,539 per staffed bed on pharmaceuticals, up a more moderate 5.8% from the year before. Facilities in seven for-profit MHSs reported pharmaceutical expenses of $11,552 per staffed bed in 2000, up just 1.5% from $11,382 reported for hospitals in eight proprietary MHSs in 1999. Midsize MHS hospitals stabilize drug costs per discharge Pharmaceutical costs per discharge for MHS hospitals with 50 to 119 beds and 120 to 249 beds rose just 1.2% and 0.6%, respectively, between 1999 and 2000. Over the same period, such costs increased 5.2% for system facilities with fewer than 50 beds, the greatest increase by size of hospital. Pharmaceutical costs per discharge were highest ($400) for system hospitals with 250 or more beds. Largest MHSs have highest Rx costs per staffed bed Pharmaceutical costs per staffed bed in MHS facilities with 250 or more beds jumped 15.1% in 2000, to $15,255 from $13,250 in 1999. Such costs for these facilities exceeded the average for all hospitals ($10,857) by 40.5%. Among system hospitals categorized by number of licensed beds, the rise in pharmaceutical costs per staffed bed in 2000 was smallest (2.6%) for those facilities with 50 to 119 beds to $8,853 from $8,625 in 1999. Heavy Surgical load means high Rx costs for MHSs MHS facilities that performed 10,000 or more surgeries yearly had higher per-discharge and perstaffed-bed pharmaceutical costs in 2000 than system facilities in any other surgery volume category. For example, pharmaceutical costs per staffed-bed for these high utilization facilities were $17,327 in 2000, at least 27.2% higher than such costs for system hospitals in any other surgery volume category. WOMEN’S HEALTH IN DEPTH15 Managed Care Takes Steps to Encompass the Whole Woman For the most part, medical science and the healthcare industry have ignored women and only now are many in the industry beginning to realize that steps need to be taken to remedy this imbalance. V.Villagra,MD, V.P.for Quality Improvement, CIGNA, noted: “There are many aspects of women’s health that have not been paid attention to as closely as they have for men.” DRUG BENEFIT CARDS Drug Benefit Card (DBC) – a pharmacist’s ally or adversary? Employers have traditionally provided benefits to their employees. Among these is a health care benefit system. Pharmacies have participated in providing pharmaceuticals to every patient that has a valid prescription order. Patients have procured their pharmaceutical needs from their trusted provider. Many employers entered into contracts with pharmacies as willing providers. Many contracts required the patient to pay the contracted price based upon a fee-for-service concept. The total price as agreed upon is usually the cost of the drug plus a professional fee. In most cases the contract price is lower than the Usual & Customary (U & C) price that is charged to other clients. When the DBC came into being, it was a simple card which was the authorization from the payer that the person in possession of the card is the beneficiary. The entry of PBMs resulted in a system that was ‘complicated’ due to the fact that each PBM had a different formula for different plans. The original system required the pharmacy to sign a contract with the PBM which in essence was a nonnegotiable instrument. From the manual system of filing claims evolved the electronic claims processing system. The system required a Point of Sale (POS) adjudication process. The pharmacy did not have to sign any contract with the payer. The processor electronically adjudicates the claim based upon the parameters that were set-up by the payer and the PBM/processor. The pharmacy is billed a processing fee based upon a per claim system. Pharmacy operations became more complicated – technology has come into play. Think of the additional investment – new hardware, software and communications systems. If a pharmacy does not participate in the system, it will cease operation. The DBC has become a nightmare for the community pharmacy operators. With the rising costs of health care PBMs/Payers have instituted a co-pay system. With numerous drugs now available in generic versions a Maximum Allowable Cost (MAC) was put into effect. The MAC was also applied to brand name drugs. Dispensing fees or professional fees are a fixed value without considering the cost of investment (COI). The cost (AWP) of the drug is also discounted – this varies from one PBM to another. Multi-tier co-payments 3-tier designs have shown mixed results. Since their inception in the late 90s there have been mixed opinion. These were designed by pharmacy directors and PBMs to give the consumer an awareness of drug costs, an alteration of prescribing patterns and having patients accept preferred drugs. PBMs have compiled formularies listing the preferred drugs. In some plans the dispensing of a preferred drug is mandatory. The pharmacist is required in many states to consult the prescriber to make the change. Higher co-pays has shifted part of the cost of pharmaceuticals to the patient. This resulted in some savings to the payer. But with the increasing cost of newer drugs the cost savings are not what as dramatic as predicted. Some employers and PBMs have started higher tiered co-pays. It is highly possible that a co-pay of 50% can become a reality. The rising out-of-pocket costs of prescriptions have made consumers inquisitive. Many patients discuss their concerns with the prescriber as well as the pharmacist. It is not uncommon that pharmacists process a prescription and the patient decides not to get the prescription filled. This puts an additional burden on the pharmacy operation. REFERENCE-BASED PRICING RBP: A Tiered Co-payment Plan in Disguise? 16 RBP refers to any system that establishes a common reimbursement level for a group of comparable or interchangeable drugs. The premise is that RBP reduces drug costs by the use of less expensive but equally efficacious drugs while maintaining the freedom of patients and physicians to choose the product they prefer. Under the RBP programs the insurer or health plan reimburses the dispensing pharmacy based on the cost of the reference agent and the member pays any additional cost for a higher-cost agent in the same therapeutic category. Patients or physicians can generally apply to receive authorization for the higher-cost agent at no additional cost if they can show that the lowercost agent has been tried and failed. In some countries where RBP has been implemented, there are reports that manufacturers of higher-cost agents have reduced their prices to the reference level in order to curb the movement of market share to lower-priced reference agents. The concept was implemented in 1995 by the British Columbian (BC) government referencing 3 initial drug classes: H2 antagonists, nitrates, and NSAIDs. In 1997, 2 additional therapeutic classes were added: angiotensin-converting enzyme (ACE) inhibitors, and calcium channel blockers. One year after the BC program was implemented there were significant reductions in prescription expenditures, with little or no corresponding reduction in the use of prescriptions within the affected drug classes. The cost of H2 antagonists dropped 38% - from $23.9 million to $14.8 million – with a reduction in use of only 5.2% in 1996. Similarly, 1 year after implementation of the BC program, the cost of ACE inhibitors showed a $6 million savings after factoring in the increased physician costs for additional visits to titrate doses. Under the current benefit designs, member co-payments are minimal in many plans and plans must continually raise both co-payments and premiums to keep pace with inflation in benefit costs. Three-, 4-, and 5-tiered plans and mandatory generic substitution have helped to some extent, but utilization tides still flow toward newer agents that are more expensive and do not have generic alternatives. The prime reason for failure is that the co-payment levels are not broad enough to have an impact on cost between the generic or preferred brand and other agents in the class or that the member perceives the difference in price to be less than or equal to the product’s therapeutic value. Agents are not placed in tiers based on therapeutic value but typically placed based on the agent’s price. With the number of co-payment tiers and options in benefit designs today, we can no longer say that our programs are not confusing to the member or easy to administer. Why don’t we just make things easy for everyone and simply charge a flat percentage co-payment on every product or a flat dollar amount toward any prescription and be done with it? Knowing that the health plan will only pay 70% or $30 of any prescription cost is easy for the patient to understand and makes the fight over getting coverage for a more expensive agent or one in a higher tier nonexistent. INCENTED FORMULARY Three-Tier Co-payments Facilitate Cost and Utilization Management17 The type of formulary gaining the most popularity is the one associated with 3-tier plans – known as an “Incented” formulary. In 2000 39% of employers used an incented formulary, up from 25% in 1999. Overall, the use of formularies increased from 74% in 1999 to 85% in 2000. The shift toward more employee control an input is evidenced by an increase in 3-tier retail copayments which allow patients the choice of either paying a lower co-payment for a generic drug or a higher co-payment for a preferred brand. The highest co-payment results in the patient paying approximately the same as if he or she had paid the difference in price between the generic and the brand-name drug. Typically, generic drugs are the first tier and the lowest co-payment. In a 3-tier the second tier is for preferred brands or single-sources drugs; and the third tier is for non-formulary or multiple-source brand-name drugs, depending on the design. Average Retail co-payment amount according to level are: Maximum – first tier $20.00; second tier $40.00 and third tier $51.00. Average - $7.17; $14.14 and $27.35, respectively. Minimum - $0.0 for first and second tier and $10.00 for third tier. OTHER DRUG-COST SAVINGS PLANS Panel Session – “What Pharmacy Providers Are Doing to Heal Your Programs” 18 B.Hawes,R.Ph.,health care consultant, Towers Perrin: “ drug expenditures have been rising at a much steeper rate than health costs in general, noting that the nation’s drug bill rose 206% in the 1990s, compared with a 97% growth for health costs. L.Karger,M.D., private practitioner: “raising co-pays might be one way to foster patients’ perceptions of what drugs really cost. To pay $10.00 for $250.00 worth of pharmaceuticals doesn’t make too much sense. There has to be a middle ground. Most patients can realize the value of drugs to their lives. So paying $30.00 or $40.00 instead of $10.00 for $285.00 worth of drugs is not all that reasonable.” D.Joyner, Sr.V.P.,Caremark Rx – “ you’d be amazed at the number of employers who still choose not to mandate generic drugs. If you can maximize generic utilization there will be significant savings.” Drug Firms Shuffle Rx Discount Cards19 Seven drug companies have paraded the Together Rx card. Up to 11 million Medicare enrollees will be eligible for the free Together Rx card, offering discounts of up to 40% on more than 150 medications. Abbott Laboratories, AstraZeneca, Aventis Pharmaceuticals, Bristol-Myers Squibb, GlaxoSmithKline, Johnson and Johnson, and Novartis Pharmaceuticals are backing the program. Discounts ranging from 20% to 40%, depending on the drugs, will be paid for by drug companies, not by participating pharmacies. The entire amount of the discounts will be passed through top cardholders. Pharmacies will be reimbursed at AWP minus 8.867% plus a $2.50 fee. The Together Rx card will be administered by McKesson Corp., which worked with the pharmaceutical firms to fashion the program. In addition to enrolling participants and issuing them cards, McKesson will contact applicants who may be eligible for even cheaper or free medications through patient-assistance programs offered by the drug manufacturers or the foundations. McKesson will work with participating pharmacies to adjudicate the Rx transactions covered by the card. Medicare enrollees who do not have public or private Rx insurance and whose annual income does not exceed $28,000 for singles or $38,000 for couples are eligible for the bright yellow card. The discounted medications treat a variety of conditions, including diabetes, hypertension, and hypercholesterolemia. Eli Lilly & Co. and Pfizer, Inc. had already jumped on the discount Rx card bandwagon. Continuing a tradition of going its own way, Merck & Co. rejected Rx discount cards but announced that its patient-assistance program will offer home delivery and will no longer require patients on chronic meds to get new Rxs every 90 days. The Together Rx program was applauded by Craig Fuller, chairman/CEO of the National Association of Chain Drug Stores (NACDS), who said his group stands ready to help spread the word so seniors can take advantage of the savings. He pointed out that all of the various Rx cards could be offered through PharmacyCareOneCard, an NACDS initiative to eliminate the discount card clutter threatening to make life even more difficult for chain R.Ph.s. Other Discount Card Issuers: 1. 2. 3. 4. 5. 6. 7. 8. 9. American Association of Retired Persons (AARP) Farmers Mutual Insurance Co. Mutual of Omaha Farm Bureau Cooperatives Numerous Banks – both regular, savings and credit unions Life Insurance companies Mortgage companies Blue Cross/Blue Shield companies YOU NAME IT – INCLUDING CREDIT CARD COMPANIES Discount cards are used to attract people to use their services and indicating that business establishments including pharmacies will honor the card and extend discounts. DRUG REBATES When is a Rebate a Kickback? 20 Discounts by pharmaceutical companies are under fire. More than 70% of American with private health insurance buy their drugs indirectly through Pharmacy Benefit Managers (PBMs). Working for employers and insurance companies, PBMs provide a wide range of services, including lower cost generics and running mail order pharmacies. Most important, however, they extract rebates from pharmaceutical manufacturers in exchange for putting the manufacturers’ products on their list of approved drugs. Critics say these secret payments add up to 10 percent of the $122 billion Americans spend on prescriptions drugs every year. The power of PBMs – the top four companies earn $57 billion a year in revenue – rests in their ability to decide which drugs an employer will pay for. In theory, PBMs push drugs that are not only effective but also less expensive. In practice, however, prescribing decisions are often driven not by the price of a drug but rather by how much the drug company is paying the PBM to recommend it. Critics say drug companies are paying ever bigger chunks of money to PBMs to boost sales of expensive drugs that are no better than cheaper alternatives. PBMs once earned most of their revenue from the administrative fees paid by corporate health plans. But these days, PBMs are more reliant on drug-maker rebates. Medco, the nation’s secondlargest PBM, reported that it would not have been profitable for the past three years had it not been for rebates. But now that these payments have come under fire, critics say the companies have started hiding them from clients and auditors by calling them by other names. They might label them “educational grants,” for instance, or “data sales fees,” or “health management fees.” Hiding the rebates also helps pharmaceutical companies maintain artificially high prices. By law, drug companies must give Medicaid their lowest price. This so-called best price must take into consideration the rebates and other incentives that manufacturers give PBMs. The more rebates a drug company has to pay, the lower the price of the drug. But if the manufacturers don’t call their rebates “rebates.” They don’t have to factor them into their best-price calculations. The projected spinoff of Medco by its parent company Merck has been delayed after questions were raised whether the unit inflated its size by claiming $12 billion in revenue (between 1999 and 2001) from co-payments by consumers to pharmacies – money that Medco never touched. How do other PBMs compare? All PBMs get rebates from manufacturers. The amount varies from one manufacturer to another and from one PBM to another. It all depends upon the volume generated thru the use of formularies. Some PBMs explain in their plan descriptions given to subscribers that they MAY get a rebate and they keep it for paying administrative expenses. In addition, contracts they sell to employers may also have specific provisions for administering the plan. PHARMACISTS’ ROLE IN COST-CONTAINMENT Health care in the U.S. is a complex entity. Much has been done by PBMs to ‘control,’ the cost of prescription drugs by design. In the process the pharmacy portion of the pie has become smaller and has not kept pace with the increase in the cost of drugs and other factors. Payers see the pharmacist, not as a professional but a dispenser of pharmaceuticals. With the tremendous growth in the number of prescriptions written by prescribers, pharmacists do not have enough time to perform additional functions, such as explaining to the patient or care giver how the medication is to be taken or administered. In the absence of diagnosis indications on the prescription the pharmacist has to rely on the patient what complaint he had when he saw the physician. However, there are instances where the patient does not even know the name of the prescriber (as happens when the patient was seen at a training hospital) and the pharmacist cannot decipher the signature on the prescription. This lack of clarity in the way prescriptions are written can lead to errors in dispensing. Pharmacists should rely more on trained technicians to do the mechanics of entering the prescription in the computer for electronic processing. Pharmacists need the support of owners or managers of drug chains to create an environment conducive to giving the pharmacist better use of his training. Patients have long been recipient of free information, no matter how scant, that is limited by the environment. Pharmacists can indirectly contribute to cost-containment by providing services that lead to better results of the treatment that is envisioned from the physician to the patient and augmented by the pharmacists. Pharmacists should get out, as time permits, to counsel patients as completely as possible so that they get better outcomes. Patients with asthma will be able to function as close to normal as possible if the pharmacist can reinforce the routines of medication use. The number of visits to emergency rooms can be reduced when pharmacists are able to help patients understand the need for taking medications properly. By reducing the number of sick days the productivity of the employee can be increased. These would seem to be intangibles but the monetary savings can be substantial. People with diabetes can be helped with proper instructions on how to use glucometers. Emphasizing the need for diet, exercise and taking medications properly will help promote the wellness of the patient. Asking patients about their condition between prescription fillings and giving suggestions when indicated will contribute towards the reduction in the cost of health care. Volunteering to be available to answer questions over the telephone will boost the morale of the patient. References: 1. Survey of Pharmacy Law, National Association of Boards of Pharmacy, 2001-2002 Ed. 2. Levy S Physician Dispensing, Drug Topics, 2001;145;41-46 3. Grauer DW, New Legislation Regarding Prescribing Authority: How Will It Affect Pharmacy? Managed Competition and Pharmaceutical Care; 1996, 148-153 4. Hepler CD, Strand LM, Opportunities and Responsibilities in Pharmaceutical Care; Am J Hosp Pharm 1990;47;533-542 5. Scott DM, Overview of Health Care in the United States, Pharmacy and the U.S.Health Care System,2nd Ed.;1997;9-27 6. Maine LL, Managed Competition: The Role of the Pharmacist, Managed Competition and Pharmaceutical Care;1997;41-55 7. Bobula JD, A New Era in Pharmaceutical Pricing; Managed Competition and Pharmaceutical Care;1997;89-99 8. Anonymous, Executive Care Directory, 2002 Eleventh Edition; Managed Care Interface 9. Anonymous, A thru Z Managed Care Terms 2001/2002; Medicom International 10. Aventis Pharmaceuticals, Bridgewater, N.J.; Managed Care Trends Digest 2001;Managed Care Digest Series 2001 – SMG Marketing Group Inc., Chicago, IL; Medical Group Management Association, Engelwood, CO; & American Medical Group Assn. Alexandria, VA 11. Aventis Pharmaceuticals, Bridgewater, N.J.; Medical Group Practice Digest; Managed Care Digest Series 2001 – Forte Information Resources LLC, Denver, CO., The Medical Group Management Assn., Engelwood, CO.; SMH Marketing Group Inc., Chicago, IL.; The American Medical Group Assn., Alexandria, VA.; & The California Assn. of Physician Organizations (CAPO), Los Angeles, CA 12. Aventis Pharmaceuticals, Bridgewater, N.J.; HMO-PPO/Medicare-Medicaid Digest; Managed Care Digest Series 2001 – Forte Information Resources, Denver, CO.; SMG Marketing Group, Chicago, IL 13. Aventis Pharmaceuticals, Bridgewater, N.J.; Integrated Health Systems Digest; Managed Care Digest Series 2002 – Forte Information Resources, Denver, CO.; SMG Marketing Group, Chicago, IL 14. Aventis Pharmaceuticals, Bridgewater, N.J.; Institutional Digest; Managed Care Digest Series 2002 – Forte Information Resources, Denver, CO.; SMG Marketing Group, Chicago, IL 15. Targovnik D, Women’s Health in Depth, Managed Healthcare News, May 1999, 15; 5; 1 16. Reissman D, Pharm D., Reference-Based Pricing: A Tiered co-payment Plan in Disguise?, Drug Benefit Trends; Dec.2001; 13; 12; 37 &34. 17. Anonymous, Three-Tier Co-payments Facilitate Cost and Utilization Management; Drug Benefit Trends; Feb. 2002; 14;2; 7 18. Buckley B , There’s room for employers to trim their drug costs; Drug Topics; 146, 5, Mar.4,2002; 74 19. Ukens C., Drug Firms Shuffle Rx Discount Cards, Drug Topics; 146, 9, May 6,2002; 26-27 20. Barnes JE, When is a Rebate a Kickback? U.S.News & World Reports ; 133, 6, Aug.12,2002, 31-33 Presented at the 19th Asian Congress of Pharmaceutical Sciences, Federation of Asian Pharmaceutical Associations, October 6, 2002, Seoul, Korea