Scientists crack peanut code in children
advertisement
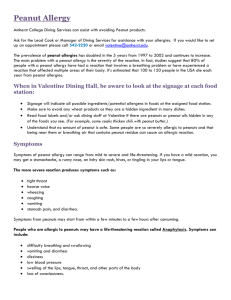
Press Release Embargoed: 00:01 hrs Monday January 11, 2010 SCIENTISTS CRACK PEANUT CODE IN CHILDREN Clinicians and scientists at UHSM (University Hospital South Manchester), the University of Manchester, and Phadia AB in Uppsala, Sweden have developed a new and significantly more accurate blood test for peanut allergy, which predicts whether an allergic reaction to peanuts will develop with more than 95 per cent certainty. Peanut allergy is one of the most common food allergies in children, with recent reports suggesting that it is on the increase. It can be severe - and in extreme cases fatal. Unlike other food allergies, which appear early in life and are usually outgrown by school age (e.g. cow’s milk or egg), peanut allergy tends to be lifelong. Professor Adnan Custovic led the research team which examined the prevalence of peanut allergy in almost 1,000 eight year olds who belong to the Manchester Asthma and Allergy Study. This group of children were recruited before they were born and have been followed up at regular intervals since birth. In this study, children with suspected peanut allergy were challenged with peanuts in a safe, controlled environment. Research has shown a huge false positive rate for current standard blood or skin tests for sensitivity to peanuts. Although approximately 1 in 10 children had positive skin or blood test results to peanut, on the basis of the oral peanut challenge, only 1 in 50 had peanut allergy. The findings, just published*, confirm that the majority of children with positive skin or blood tests to peanut do not have clinical peanut allergy, and describe a new blood test which accurately identifies those children at real risk. Professor Adnan Custovic, said: “Avoiding peanuts is the best way of managing allergic / anaphylactic reactions to peanuts. Complete avoidance is difficult to achieve due to the widespread use of peanuts in prepared foods, and accidental exposures are common and may be life-threatening. The fear of possible reaction markedly reduces the quality of life amongst peanut-allergic patients and their families. However, avoiding peanuts only makes sense if a child is really allergic. . “Parents are often anxious to find out whether their child diagnosed with another food allergy will react to peanut, or whether siblings of their peanut allergic child have peanut allergy. The lack of specificity of current tests when used in isolation indicates many patients will inappropriately be given the diagnosis. The new diagnostic test which accurately discriminates peanut allergy from tolerance will mean we can target avoidance to those patients really at risk, and remove the considerable stress that comes from the many false positive sensitivity tests. ”Patients must be able to receive expert help to determine real allergy to peanuts. New diagnostic tests combined with expert advise on treatment will be a major step forward in management of patients with peanut allergy”. Professor Ashley Woodcock, Head of the National Institute for Health Research (NIHR) Translational Research Facility in Respiratory Medicine at UHSM commented: “This is just one example of the sort of translational research for patient benefit that NIHR funding is now driving”. *Journal of Allergy and Clinical Immunology January 2010 edition – Ends – For more information Contact Susan Osborne, Director of Communications at UHSM on 0161 291 4972 or mobile 07836 229208. The study was also supported by a charitable donation from Jackie and Carl Michaelsen. Notes to Editors Methods: Within a population-based birth cohort, the team ascertained peanut sensitisation by skin tests and IgE measurement at age 8 years. Amongst sensitised children they determined peanut allergy versus tolerance by oral food challenges. They used open challenge amongst children consuming peanuts (n=45); others underwent double-blind placebo-controlled challenge (n=34). They compared sensitisation profiles between peanut-allergic and peanut-tolerant children using microarray with 12 pure components (major peanut and potentially cross-reactive components, including grass allergens). Results: Of 933 children, 110 (11.8%) were peanut-sensitised. Nineteen were not challenged (17 no consent). Twelve with a convincing history of reaction(s) upon exposure, high specific peanut IgE≥15kUa/L and/or positive peanut skin test≥8mm were considered allergic without challenge. Of the remaining79 children who underwent challenge, seven had ≥2 objective signs and were designated peanut-allergic. The team estimated the prevalence of clinical peanut allergy amongst sensitised subjects as 22.4% (95% CI 14.8%–32.3%). Using component-resolved diagnostics, we detected marked differences in the pattern of component recognition between peanut-allergic (n=29; group enriched with 12 allergic children) and peanut-tolerant (n=52) children. The peanut component Ara h 2 was the most important predictor of clinical allergy. Conclusions: The majority of children considered peanut sensitised based on standard tests do not have peanut allergy. Component-resolved diagnostics may facilitate the diagnosis of peanut allergy.