High Dependency Care For Obstetric Patients
advertisement

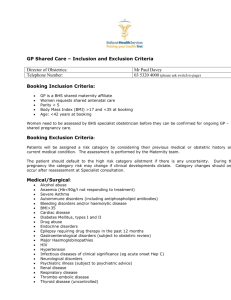
High Dependency Care for Obstetric Patients Content Section 1.0 2.0 3.0 3.1 3.2 3.3 3.4 3.5 4.0 5.0 Content Introduction Aims and objectives Management Admission criteria Responsibility of different staff groups Equipment requirements When to involve clinicians from outside the maternity service Criteria for transfer Audit and Monitoring compliance References Page 3 3 3 3 4 5 6 6 7 8 1.0 INTRODUCTION Whilst most pregnancies and births are normal and without complications, there are some occasions when women will require a higher level of care than that normally provided in a general care setting. In these instances the women should be cared for in a suitable environment by staff able to provide the necessary level of care. Determining what type of care a woman should receive is based on clinical judgement utilising the criteria outlined in the Intensive Care Society’s Standards and Guidelines for the Levels of Critical Care in Adult Patients1. High dependency Care (ICS Level 2 care) High dependency care is required for women needing more detailed observation or intervention including basic support for a single failing organ system, extended post-operative care and those stepping down from higher levels of care. Intensive Care (ICS Level 3 care) Patients requiring a higher level of care than outlined above will need to be stabilised and transferred to an Intensive Care Unit. For example, women requiring support for 2 or more organ systems, artificial ventilation, renal replacement therapy, risk of sudden catastrophic deterioration. Although it is acknowledged that the location of the woman should not determine their level of care - it is expected that within the maternity service women requiring high dependency care will usually be cared for on the Delivery Suite. The LGI site has a designated area within the Delivery Suite for providing HDU care, the SJUH site use a fully equipped delivery room to provide the same level of care as in an HDU unit. If a woman needs ICU care she is transferred to general ICU unit at the respective sites providing that a bed is available. In some circumstances it may be necessary to transfer the woman to another unit providing intensive care services. 2.0 AIMS AND OBJECTIVES The aims and objectives of this protocol are to outline the processes for ensuring that women receive high dependency care / intensive care in a suitable environment. In particular it specifies: Admission criteria The responsibilities for the different staff groups The process for ensuring the availability of equipment in line with national guidance Guidance on when to involve clinicians outside the maternity unit Agreed criteria for transfer to HDU / ICU outside the maternity unit 2 3.0 MANAGEMENT 3.1 CRITERIA FOR TRANSFER 3.1.1 Criteria for transfer to high dependency care These may be met either before or after delivery. The indication for the woman to receive HDU care should be documented in the hospital records or birth record. All women receiving high dependency care should have observations recorded on a modified obstetric early warning chart (MOEWs) in order that deteriorating condition can be identified. Patients who are receiving continuous oxygen therapy are not suitable to step down to level 1 care (ward based) and so will need to remain on delivery suite even if otherwise well. Table 1: Examples of indications Obstetric Indications Non-obstetric Indications Eclampsia Transfer from ICU Sepsis Other surgical procedures or complications related Severe pre-eclampsia to surgical condition Severe asthma Pneumonia/respiratory embarrassment Major haemorrhage (over Hypertension 1500mls) Renal impairment Diabetic ketoacidosis Thyrotoxicosis Thromboembolism Cardiac or neurological co-morbidity HELLP syndrome Morbid obesity (BMI over 40kg/m2) with coPuerperal sepsis morbidities This list is not exhaustive and the need for HDU care should be assessed on an individual basis. When HDU care is required, the midwife/nurse to patient ratio must be no more than one midwife /nurse to two patients. 3.1.2 Discharge Criteria from HDU to Ward This will be when care can be managed on a maternity ward and must take into account staffing levels, skill-mix and workload on the ward to which the patient is being discharged. A written treatment plan, including clear instructions about the continued level of observation and when to call medical staff, must be documented at the time of transfer. Continued support from the obstetric and anaesthetic staff based on the delivery suite may be required and must be provided. Transfer out of HDU should be a joint obstetric and anaesthetic decision made at consultant level unless exceptional circumstances apply and fulfill the following: Patient haemodynamically stable, no further continuous intravenous medication or frequent blood tests required No invasive monitoring required No active bleeding No supplementary Oxygen required Patient mobilized. 3 There is a named consultant anaesthetist responsible for all HDU patients 24 hours per day. When transferring a woman from HDU to the postnatal ward a personal handover of care should be given from the midwife handing over care to the receiving midwife utilising the SBAR principle for communication. This should be person to person the woman should be accompanied to the postnatal ward as there may be significant complications that require a more detailed handover and should always be done face to face to the receiving midwife by either a midwife , nurse or doctor. 3.1.3 Criteria for transfer to ICU Care Women requiring ICU care are generally transferred to an ICU within the Trust. Following assessment of the woman’s condition, the decision for transfer will be made by the Consultant Obstetrician and the Consultant Anaesthetist in liaison with other specialties as required. The reason for transfer should be clearly documented in the Hospital records and/or birth record Women who may require ICU care have usually more than one organ failure including: Women requiring advanced respiratory support (ventilation) Women requiring invasive renal support Women requiring inotropic support would be considered Exacerbation of pre-existing medical problem. Plans would be made between the Consultant Obstetric anaesthetist, Consultant Obstetricians and the Intensive Care Consultant again using the SBAR principle for communication. On going care for these women must include daily conference between these key personnel. Discharge from ICU is a consultant level decision and should be back to an obstetric HDU in the first instance unless otherwise directed. The outreach team may need to provide advice and support following discharge from ICU but this will be at the discretion of the Consultant Anaesthetist and Consultant Obstetrician and will depend on the original indication for admission to ICU. Again the transfer should be made person to person the woman should be accompanied to the HDU area as there may be significant complications that require a more detailed handover and should always be done face to face to the receiving midwife by either a midwife, nurse or doctor. 4 3.2 Responsibilities of the different staff groups The table below outlines the key roles and responsibilities of staff involved in the care of women requiring level 2 care or above. ROLE Obstetricians RESPONSIBILITIES Attend & review woman at least 3 times/24hours (as a minimum on ward rounds at change of shift) review of investigations and actions as appropriate communicate with other staff about plan of care and escalate if more senior review required Respond to an abnormal MOEWs score Documentation Individual plan of care in hospital records Discussing care with woman and/or partner Document discussions in records Liaise with MDT regularly regarding appropriate level and place of care Document discussions in hospital records Be aware of transfer criteria as stated in guidance and arrange transfer as appropriate Anaesthetists Ensure patient is physiologically stable and that appropriate monitoring is in place Be immediately available to review woman if her condition deteriorates Document reason for change in level of care and personnel required to undertake transfer Document plan of care (may be part of ward round documentation from obstetric team as above) Liaise with ICU/outreach team if woman requires level 3 care Accompany woman to ICU and handover care to receiving team Midwifery Staff Document discussions in hospital records Document handover of care including name of person taking over care To undertake physical observations Documentation on the for women and report any change in MOEWs chart score to medical staff To provide support for women and their partners/family 5 photocopy birth records and hospital records if transferring outside the Trust Accompany woman to ICU and handover care to receiving team Document handover of care including name of person taking over care using SBAR sticker or SBAR headings 3.3 Equipment requirements HDU care should be conducted in the appropriate care setting with staff skilled and trained in this area. The basic equipment available in both the HDU and in delivery suite rooms to provide HDU care is: equipment available to monitor vital signs including, pulse, blood pressure, and oxygen saturation (eg SPACELAB / Dynamap) Oxygen supply with masks and tubing Suction with Yankauer catheter and tubing with various size suction catheters Ambubag and masks of different sizes. Emergency intubation equipment and drugs (on Crash trolley) Minitrach tracheostomy set (on crash trolley) Assorted cannula for intravenous access / drip stands Wound dressings , tape Gloves (Sterile / unsterile in various sizes) / Aprons In addition there is daily stock check of drugs and fluids. Equipment and algorithms required for resuscitation and care of HDU patients are included in Trust Basic HDU Competencies document. To ensure the availability of all necessary and functioning equipment, an inspection is undertaken on a daily basis by the duty Operating Department Practitioner (ODP) and/or Delivery Suite Midwife. If any defects/ faults are found in the equipment at inspection then it is removed from service and reported promptly to Medical Physics (LGI ext: 23492, SJUH ext 66167). A note will be made in the communication book and the information passed on at each shift change so that all staff are aware. Extra equipment is available in the theatre store cupboard if required. This equipment is checked on a regular basis by Medical Physics 3.4 Guidance on when to involve clinicians outside the maternity unit Transfer out of Obstetric HDU care requires the woman to be assessed jointly by a senior anaesthetist and a senior obstetrician and in some cases other disciplines that have been involved in the woman’s care e.g. renal, cardiac. Senior clinicians from other specialties will be involved in the care of women where there is: 6 1. Failure of more than one system 2. Disease whose management is out-with the expertise of the obstetric or anaesthetic team e.g. i renal failure, other than the impairment associated with pre-eclampsia ii hepatic failure iii respiratory disease especially that requiring ventilatory support iv cardiac disease, pre-existing or of recent onset v neurological conditions vi endocrine disease including diabetes mellitus vii non-obstetric surgical problems The referral will be at Consultant level and ideally such women will be reviewed by the Consultant from the appropriate specialty. The reason for referral and who the referral is made to should be documented in the Hospital records and/or Birth record The outreach team should be consulted if there is a transition to or from the ICU or for help with a specialised problem e.g. high flow oxygen therapy. Once the patient is deemed to have stabilised sufficiently to be nursed on a postnatal ward, this will be communicated to the midwife responsible for her care as well as the co-ordinating midwife. There should be a clear plan of on-going care and observations documented on the MOEWS chart once the HDU chart is no longer necessary. 4.0 AUDIT AND MONITORING COMPLIANCE A clinical incident report will be completed for all women admitted to intensive care or transferred to high dependency care outside the maternity unit. Each case will be reviewed at the weekly risk management meeting who will decide if any further action is required including a level 2 investigation. A multidisciplinary annual audit will be carried out in accordance with the Maternity Services Audit Plan. Auditable standards include: Number of women cared for in HDU Length of stay Admission and discharge criteria involvement of clinicians outside the maternity service responsibilities of different staff groups availability of medical equipment documentation requirements Audit results will be presented at the Women’s Services Clinical Governance and Audit meeting and an action plan developed as necessary. A lead will be appointed for monitoring of the action plan, including re-audit, and the status of the action plan reported to the Women’s Services Clinical Governance and Risk management Forum quarterly. Audit results will be included in the Maternity quarterly risk 7 management report and any resulting changes disseminated via the Maternity Services Forum, Team Leaders Forum, Supervisor’s Forum. 5.0 Evidence Base ICNARC (Obstetric) 2010 The Joint Standing Committee of the RCoA and RCOG, in collaboration with the OAA, commissioned ICNARC to introduce fields for “currently pregnant” and “recently pregnant” into their well established Case Mix Programme from February 2006. http://www.oaaanaes.ac.uk/content.asp?ContentID=323 Sabir N, Vaughan DJA, Lucas DN, Chan I, Bhuptani S, Robinson PN. A survey of obstetricians' knowledge of aspects of acute care in maternity HDU patients. Int J Obstet Anaesth 2009; 16: S21. Swanton RDJ, Al-Zawi S, Wee MYE. Obstetric Early warning scoring systems- an OAA approved national postal survey IJOA 2008 O14 Srinivas K, Yadthore S, Collis RE. Obstetric high dependency facilities: a survey of current practice. Int J Obstet Anaesth 2007;16: S45. Rathinam S, Khan A, Rupasinghe M. Preparation of midwives for high risk care: viewpoint of the midwife (Abstract). Int J Obstet Anesth 2007; 16: S50. Harrison DA, Penny JA, Yentis SM, Fayek S and Brady AR. Case mix, outcome and activity for obstetric admissions to adult,general critical care units: a secondary analysis of the ICNARC Case Mix Programme Database Critical Care 2005 Vol 9 No Suppl 3 Gatt S. Pregnancy, delivery and the intensive care unit: need, outcome and management. Curr Opin Anaesthiol 2003; 16: 263-7in Ryan M, Hamilton V. The role of high dependency unit in a regional obstetric hospital. Anaesthesia 2000; 55: 1155-8 Cordingley JJ, Rubin AP. A survey of facilities for high risk women in consultant obstetric units. Int J Obstet Anesth 1997; 6 General, Outreach/MEWS Department of Health. Comprehensive Critical Care: a review of adult critical care services. London: DoH, 2000. www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4006 585<http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidanc e/DH_4006585> An Acute Problem? A Report of the National Confidential Enquiry into Patient Outcome and Death. www.ncepod.org.uk<http://www.ncepod.org.uk> 2005. Out of our reach?: Assessing the Impact of introducing a critical care outreach service. Pittard A.J. Anaesthesia 2003; 58: 882-885. Knaus WA, Draper EA, Wagner DP, Zimmerman JE (1985). "APACHE II: a severity of disease classification system". Critical Care Medicine 13: 818–29. PMID 3928249<http://www.ncbi.nlm.nih.gov/pubmed/3928249>. Stenhouse C, Coates S, Tivey M, Allsop P, Parker T. Prospective evaluation of a modified Early Warning Score to aid earlier detection of patients developing critical illness on a surgical ward. British Journal of Anaesthesia 2000; 84: 663 McQuillan P, Pilkington S, Allan A, et al. Confidential enquiry into quality of care before admission to intensive care. British Medical Journal 1998; 316: 1853-8. Goldhill DR, Worthington L, Mulcahy A, Tarling M, Sumner A. The patient-at risk team: identifying and managing seriously ill ward patients. Anaesthesia 1999; 54: 853-60. Morgan RJM, Williams F, Wright MM. An early warning scoring system for detecting developing critical illness. Clinical Intensive Care 1997; 8: 100. Physiological values and procedures in the 24h before ICU admission from the ward. Goldhill et al. Anaesthesia 1999; 54: 529-34. 8 Protocols relating to care of Obstetric Women requiring High Dependency Care (HDU) / Intensive Care (ICU) Author(s) Audrey Quinn (Consultant Anaesthetist); Katie-Sue Leech (Midwife) Contact name Audrey Quinn (Audrey.quinn@leedsth.nhs.uk) Approval Maternity Services Forum process for amendments First Issue Date September 2010 Reviewed July 2012 Version no: 2.0 Review Date: July 2015 Ratified by Maternity services Clinical Management forum (27/08/2010) Amendments approved by MSF 22/06/2012 Ratified by Governance and Risk Consultation Process Maternity Services Guideline Group / Maternity Services Forum, Maternity Services Clinical Governance and Risk Management Forum / Obstetricians / Team Leaders / Supervisors of Midwives Scope of guidance Clinical condition High Dependency/Intensive Care for Maternity Patients Patient Group All women delivering within LTHT requiring High Dependency/Intensive Care All Health Care Professionals involved in the provision of maternity care within the Leeds Teaching Hospitals NHS Trust Professional Group Distribution List Consultant Obstetricians Obstetric Anaesthetists Head of Midwifery Midwifery matrons Midwifery Team Leaders (for distribution to midwives within their areas) Supervisors of midwives Dissemination Via Risk Management Midwife Audit and Monitoring Will be carried out in accordance with Maternity Services Audit Plan Equity and Diversity Leeds Teaching Hospitals NHS Trust believes in fairness, equity and above all values diversity in all dealings, both as providers of health services and employers of people. The Trust is committed to eliminating discrimination on the basis of gender, age, disability, race, religion, sexuality or social class. We aim to provide accessible services, delivered in a way that respects the needs of each individual and does not exclude anyone. By demonstrating these beliefs the Trust aims to ensure that it develops a healthcare workforce that is diverse, non discriminatory and appropriate to deliver modern 9 healthcare. 10