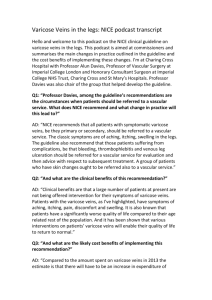
Varicose Veins
advertisement
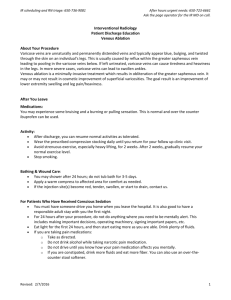
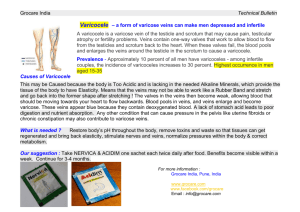
Varicose Veins Varicose veins are dilated, tortuous veins in the leg. Most varicose veins are primary; the remainder are secondary to other disorders such as deep venous thrombosis or pelvic occlusion. Varicose veins occur in young adults and incidence increases with age to 80% at 60 years. Women are affected more frequently than men. Varicose veins are asymptomatic in the majority of people, yet remain one of the most common reasons for surgical referral in the developed world. Prominent varicosities usually develop slowly, over a period of 10-20 years. In most cases, the process begins in the groin with failure of the sapheno-femoral valve. The long saphenous system is involved in 90% of cases; the short system, in 10%. Causes Congenital: absence of valves in the iliac veins abnormal vein wall elasticity arteriovenous fistulae e.g. Robertson's giant limb Acquired: obesity in women (but not in men) prolonged standing parity - women are affected six times more often than men, the majority of cases following a second or third pregnancy; important factors may include: o impaired venous return, due to pressure on the iliac veins from the pregnant uterus o high level of progesterone which alters collagen structure, sometimes irreversibly, and relaxes smooth muscle previous deep vein thrombosis - valves damaged when the veins recanalise It is currently thought that the wall of the vein is weak in patients with varicose veins and that valvular incompentence follows rather than causes the dilatation of the vein. This theory is supported by the observation that early dilatation is usually distal to an incompetent valve not proximal as might be expected if the damaged were caused by a descending valve incompetence. There are three types of varicose veins: trunk varicosities are large varicose veins which lie along the path of the long or short saphenous veins reticular varicosities are small dilates veins which lie away from the path of the main saphenous veins telangiectasiae are very small dilatations also called spider veins Incompetent valves commonly develop: in the groin, where the long saphenous vein joins the femoral vein in the lower medial thigh, where the mid-thigh perforator joins the deep system at the adductor canal behind the knee, where the short saphenous vein joins the popliteal vein behind the medial border of the tibia, where several veins perforate the deep fascia of the calf Symptoms disfigurement: o patients are frequently disturbed by the poor cosmetic appearance of their legs o both their concern and their symptoms may worsen in the summer when the legs are warm and exposed pain: o o o legs frequently ache, especially after prolonged standing patients often describe a dull, heavy, "burning" sensation that becomes more severe as the day progresses in women, symptoms may worsen in the few days prior to menstruation itching: o the skin over the varices may itch o may be associated with varicose eczema heaviness worry: o patients may present because of concern about possible complications such as ulceration Examination: varices appear on standing and disappear when recumbent positive Brodie-Trendelenburg test doppler flow studies identify 'backflow' through incompetent valves Investigation Ideally all patients with varicose veins would have colour duplex ultrasound scanning to determine the characteristics of blood flow in the leg. Unfortunately this is not possible and so duplex scanning is reserved for the following groups of patients with: recurrent varicose veins a history of superficial thrombophlebitis a history of DVT varicose eczema haemosiderin discolouration lipodematosclerosis venous ulceration Treatment of varicose veins may be indicated to relieve discomfort, to prevent or ameliorate complications, or for cosmetic reasons. Methods: conservative surgical: o sclerotherapy - permanent obliteration of varices o open operation - removal of varices with ligation of incompetent perforaters o alternatives to the current operative techniques are being introduced (1) endovenous obliteration using radiofrequency (diathermy) or laser has been devised to close the long saphenous vein, an alternative to the traditional "stripping." "powered phlebectomy" - this is another new technique that obviates the need for multiple "phlebectomies" to avulse calf varicosities, thus giving a more cosmetically favourable outcome. About one-third of cases can be managed by offering common sense advice as to how to take care for their legs. Complications caused by the varicose ulcers themselves include: haemorrhage: o bleeding may be profuse because of the high venous pressure superficial thrombophlebitis Complications caused by associated venous hypertension include: ankle oedema varicose eczema lipodermatosclerosis: atrophie blanche severe excoriation from scratching venous ulceration