Pulmonary Nodules
advertisement

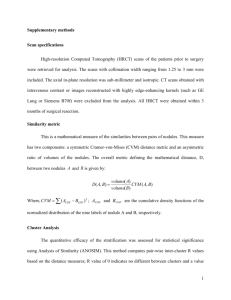
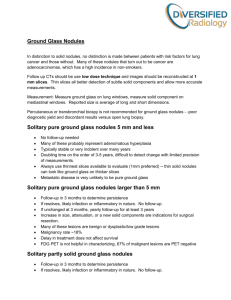
PULMONARY NODULES Mita Sanghavi Goel, M.D. January 22, 2003 Overview Pulmonary nodules are lesions which range from as small as 5mm to as large as 4-6 cm. Anything larger is considered a “mass,” and predicts higher probability of malignancy It is important to distinguish between single and multiple pulmonary nodules, as this may affect the workup. Solitary Pulmonary Nodule General Information Common entity and was found in 1 out of 500 serial cxrs in one study. Characteristic Appearances Size: The larger the lesion, the more likely it is to be malignant. Border: Benign nodules tend to have smooth, sharp borders and malignant nodules tend to be larger with irregular, fuzzy margins Calcification: Central, diffuse, laminated, and popcorn patterns indicate benign lesions. Eccentric or multiple fleck patterns may be more indicative of malignancy. Cavitation: Can occur with both benign and malignant lesions Differential Diagnosis Malignant Tumors (25-50%) Variation in incidence is due to geographic variation in prevalence of granulomatous diseases (histoplasmosis, coccidioidomycosis, tuberculosis, cryptococcosis in immunocompromised) Probability of malignancy increases with size. Most common malignancies are bronchogenic carcinoma, bronchial adenoma (carcinoid), and solitary metastatic lesions (sarcoma, colon, breast, kidney, testicular). In patients with a history of extrapulmonary malignancy, solitary pulmonary nodules are metastatic disease in 25-50% of cases. Doubling time of 20-400 days, whereas benign lesions are usually <20 or >400 days. Benign Tumors (3%) Hamartoma: Popcorn calcifications (sharply circumscribed lobulated margins) Infectious Granulomatous Diseases (up to 50%) Tuberculoma: Decreasing in incidence over time in the United States Histoplasmoma Coccidioidoma PCP Non-infectious Granulomatous Diseases (3%) Rheumatoid nodules Wegener’s granulomatosis Paraffinoma Other Causes (4%) Pulmonary infarcts Amyloidoma Hematoma Dirofilaria (dog heartworm) nodule: present as noncalcified, pleural-based nodule. Pseudotumors Spherical pneumonias Workup History/Physical: Age, smoking status, occupational exposure, immune status, and prior cancer history and medical history are important to elicit. Look for physical signs of systemic illnesses that may present as pulmonary nodules (such as rheumatoid arthritis). CT: To evaluate calcification pattern and look for additional nodules and lymphadenopathy Biopsy: Bronchoscopy has lower yield than FNA. VATS is another option. Assess patient’s preference for treatment/additional evaluation. Beth Israel Deaconess Medical Center Residents’ Report Multiple Pulmonary Nodules Differential Diagnosis Malignant Tumors Metastatic Disease (80%) o Most commonly testicular, ovarian, kidney, breast, anal, melanoma, and sarcoma. o Hematogenous: Lower lobe predominance, range from 0.5-10cm and occasionally have cavitation. If calcifications present, think of osteogenic sarcoma or condrosarcoma. Wide range in size of nodules is suggestive of this. o Lymphogenous: Lower lobe predominance, not calcified and rarely cavitated. Most often secondary lymphoma. Look for associated lymphadenopathy. Multicentric Alveolar Carcinoma Lymphoma: Non-Hodgkin’s has lower lobe predominance. Multiple primary neoplasms (bronchogenic carcinomas, adenomas) Plasmacytomas Kaposi’s sarcoma: Peribronchovascular distribution and often >1cm at diagnosis. Benign Tumors Hamartomas Juvenile papillomatosis Chondromas (Carney’s syndrome) Benign metastasizing leiomyomas Other benign causes Infectious o Granulomas (see list for solitary pulmonary nodules). o Abscesses associated with bacteremia are generalized but more numerous in lower lobes and are well defined 0.5-3cm lesions with thick walls and occasional cavitation. o Septic emboli have a predilection for the periphery of the lower lobes. Cavitation and thin walls are often seen. o Invasive aspergillosis has no set pattern of distribution, but often has a surrounding ground glass appearance (halo sign) because of local hemorrhage, or later, cavitation with air crescents. Noninfectious granulomas (sarcoid, Wegener’s, rheumatoid, paraffinomas, lymphomatoid granulomatosis). o Wegener’s is widely distributed and lesions may be as large as 10cm. 1/3 to 1/2 have cavitations. They are often thick-walled and have focal areas of air-space consolidation. o Sarcoid is widely distributed and are 0.5-3cm large. They do not typically have calcification or cavitation. Parasitic (paragonimiasis, hydatid cysts, dirofilariasis): paragoniomiasis has a predilection for the lower lobes, usually in the periphery. May also have linear shadowing from burrow tracts. AVMs: lower lobe predilection and are well-defined oval lesions ranging from 1-several centimeters. Diagnosed by spiral CT which can identify feeding artery and draining vein) Bronchial lesions (cystic bronchiectasis, mucoid impaction syndrome, ABPA) Mycetomas Amyloidomas Pneumoconioses: Upper lobe predominance. Does not have calcification, but occasionally has cavitation. Often has a background of diffuse nodular or reticulonodular shadows. May see compensatory hyperinflation. Silicosis: Upper lobe predominance with “angels’ wings” (lateral margin parallel to chest wall), with occasional cavitation. May see other changes of silicosis as well. Pseudometastases Workup H&P Spiral CT scan: Standard for detection of nodules because of ability to reduce respiratory motion, perform 3D reconstruction. Also can detect 1-2 mm peripheral nodules and differentiate between tubular and spherical structures in cine view. Biopsy: May not be required if history, radiographs, and non-invasive studies provide diagnosis (i.e. Wegener’s). Choose between CT-guided, transbronchial forcep or needle biopsy, and thoracoscopy based on location and size of lesion. Beth Israel Deaconess Medical Center Residents’ Report