Type 1 Diabetes and pregnancy 2012
advertisement

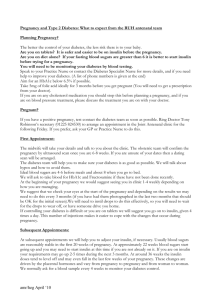
Pregnancy and Type 1 Diabetes: What to expect from the RUH antenatal team Planning Pregnancy? The better the control of your diabetes, the less risk there is to your baby. Aim for an HbA1c below 7% or 50mmol/mol if possible. Take 5mg of folic acid ideally for 3 months before you get pregnant (You will need to get a prescription from your doctor) Speak to your Diabetes Specialist Nurse for more details, and if you need help to improve your diabetes. (A list of phone numbers is given at the end) Pregnant ?: If you have a positive pregnancy test contact the diabetes team as soon as possible. Ring Dr Tony Robinson’s secretary (01225 824530) to arrange an appointment in the Joint Antenatal clinic for the following Friday. If you prefer, ask your GP, Practice Nurse or Diabetes Specialist Nurse to do this. First Appointment: The midwife will take your details and talk to you about the clinic. The obstetric team will confirm the pregnancy by ultrasound scan once you are 6-8 weeks. The diabetes team will help you to make sure your diabetes is as good as possible. We will talk about hypos and how to avoid them. With tighter control they might not be so easy to recognise and you will need to check your blood sugars regularly, especially when you drive. Ideal blood sugars are 4-6 before meals and about 8 when you go to bed. We will ask to take blood for HbA1c and Fructosamine if these have not been done recently. At the beginning of your pregnancy we would suggest seeing you in clinic 1-4 weekly depending on how you are managing. We suggest that we arrange to check your eyes at the start of the pregnancy and depending on the results we may need to do this every 3 months (if you have had them photographed in the last two months that should be OK for the initial screen). Subsequent Appointments: At subsequent appointments we will help you to adjust your insulin as necessary. Usually insulin requirements are reasonably stable in the first 20 weeks of pregnancy, although there may be an initial increase if your control needs tightening. At 12-18 weeks the insulin levels may go down a bit. At approximately 22 weeks insulin requirements start going up and may be double or more what you started with. (Your insulin doses at the start of pregnancy will be noted down in your maternity notes). At around 36 weeks the insulin doses tend to level off and may even fall in the last few weeks of your pregnancy. These changes are driven by the placental hormones and vary from pregnancy to pregnancy and from woman to woman. We normally ask for a blood sample every 4 weeks to monitor your diabetes control. Screening Tests: All pregnant women are offered a screening test to assess the chance of the baby having Down’s syndrome. In this trust we offer a combined blood test and nuchal translucency scan at 11-13 weeks. This is carried out at the dating scan clinic which is held at the Royal United Hospital. The midwife will discuss these tests with you. All pregnant women are offered a scan at around 20 weeks to check how your baby is developing. This is especially important for women with diabetes as poor control may affect the baby’s development. Growth Scans: From 24 weeks we will perform a growth scan every month, to check the baby is growing well and its tummy is not getting too fat (macrosomia) Delivery: All women with diabetes should have their baby in hospital in the Royal United Hospital not a midwifery-led unit. We see you usually every two weeks in the latter half of the pregnancy, although this may vary according the way the pregnancy is progressing. Most pregnant mothers with diabetes will deliver at around 38 weeks, as the baby is considered mature after 37 weeks. There is evidence that leaving the baby beyond 38 weeks may increase the chance of the placenta failing and the baby being stillborn. The obstetricians will discuss the method of delivery .This will depend on how big the baby is and the method of delivery for any previous babies you may have had. Often labour will need to be induced. You will normally have an insulin drip put up during the delivery to control your diabetes, and this will be stopped once the baby is delivered and you feel like eating. Remember to use the doses you used before pregnancy, if you are breast feeding (which we encourage) you will need to reduce the insulin doses further (by approximately 25%). We will discuss this with you nearer the time of your delivery. Your baby has an increased risk of newborn problems, the most common being hypoglycaemia. The best way to avoid this is to keep your control as good as possible right up to the time of delivery. The baby will be observed closely for the first 24 hours or so with blood glucose levels being checked after feeds. If the baby’s sugar levels become very low then he or she will need to be admitted to the newborn special care unit to have a sugar drip. Usually this is not necessary and your baby stays with you on the postnatal ward. However a 3 hour discharge will not be possible for you and the baby even if the delivery itself is straightforward. Diabetes Specialist Nurses Contact Numbers : Helen Griffiths/Ainslie Lang (RUH) 01225 824198 Sally Wylie (Bath) 01225 824173 Bernadette Hall (Trowbridge) 01225 711443 Nikki Hillier (Chippenham) 01249 456483 Martine Saunders (Frome) 01373 454778 Delivery suite 01225 824447/824847 Antenatal clinic 01225 824650/824645