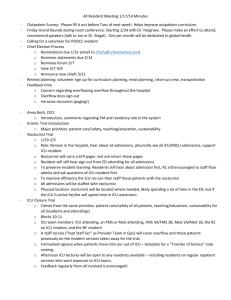
core ICU rotation - CriticalCareMedicine
advertisement

University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program PROGRAM GOALS The Critical Care Training Program at the University of Alberta is an integrated medical/surgical program for the training of residents in adult critical care medicine. It is designed to take residents from their base specialties of Anesthesia, General Surgery, Internal Medicine and subspecialties, Emergency Medicine and Cardiovascular Surgery, and over a two year period provide them with the key competencies and experience necessary to fulfil the role of physician in a community or tertiary general systems intensive care unit or a subspecialty Intensive Care Unit. PROGRAM OBJECTIVES The program provides training according to the objectives outlined in the Royal College of Physicians of Surgeons of Canada (RCPSC) document - “Objectives of Training and Specialty Training Requirements in Adult Critical Care Medicine”. The resident training objectives for the essential roles and key competencies are based on the Royal College CanMEDS roles. The CanMEDS roles focus on the knowledge, skills, and attitudes that are pertinent to the expected roles and competencies of the adult critical care medicine specialist. The CanMEDS competencies include the roles of: Medical Expert/Clinical Decision-Maker Communicator Collaborator Manager Health Advocate Scholar Professional The RCPSC Accreditation document provides general and specific objectives for the CanMEDS roles. Our program documents provide the resident with additional information regarding the training objectives and the clinical experience and knowledge areas to achieve the training objectives. The program uses the following to achieve the training objectives: Core critical care rotations o Rotations occur in the tertiary ICUs at the Royal Alexandra and University Hospitals Elective rotations o Rotations are tailored according to the resident’s career goals Formal education sessions o Seminars, journal club, ICU Grand Rounds o Informal education activities - bedside teaching, management meetings Courses & Conferences University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program TRAINING OBJECTIVES A. Medical Expert/Clinical Decision-Maker General Requirements The adult critical care medicine resident must demonstrate: a. Diagnostic and therapeutic skills for ethical and effective care of the critically ill patient; b. The ability to access and apply relevant information to the practice of critical care; c. Effective consultation services with respect to patient care, education and legal opinions. Specific Requirements A. The adult critical care medicine resident will: 1. Demonstrate detailed knowledge of the generalist and specialist aspects of critical illness; 2. Demonstrate competencies in the safe application of equipment, careful monitoring, judicious use of drugs, and the coordinated provision of multidisciplinary care for effective organ system support; 3. Demonstrate ability to recognize, resuscitate, and stabilize patients sustaining, or at risk of, cardiopulmonary arrest or other life-threatening disturbances; 4. Demonstrate working knowledge of applied clinical physiology and homeostasis and the ability to recognize, prevent, and treat single or multiple organ failure; 5. Demonstrate basic understanding of physiology, pathophysiology, and pharmacology as they pertain to the critically ill patient; 6. Demonstrate both basic and applied knowledge of the following organ dysfunction, disorders and health issues, as outlined below: (see appendix 1 for knowledge topics) a. b. c. d. e. f. g. h. i. j. k. l. m. n. o. p. q. r. s. Respiratory Dysfunction Cardiovascular Dysfunction Neurological Dysfunction Neuromuscular Dysfunction Renal Dysfunction Gastrointestinal Dysfunction Hepatic Dysfunction Hematological/Oncologic Disorders Metabolic - Endocrine Disorders Trauma Septic Illness Intoxication Burns and/or Electrical Injury Nutritional Support Pharmacotherapy Transportation Transplantation End of Life Issues Critical Illness in Pregnancy B. Demonstrate proficiency in the following technical skills: (see appendix 2 for list of technical skills) a. Airway b. Breathing c. Circulation d. Central Nervous System e. Renal f. Gastrointestinal University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program g. Nutrition h. Transport i. Other Program Curriculum The RCPSC Standards document provides an outline of the key competency roles (CanMEDS) to be acquired during training. Our program documents provide comprehensive lists of basic science and clinical science knowledge areas under the competency of medical expert /clinical decision maker that have to be covered. Clinical rotations and formal weekly teaching sessions are organised according to the above curriculum. The formal teaching sessions consist of basic and clinical sciences and sessions on bioethics, research, administration and medicolegal issues. Teaching sessions are either didactic lectures or seminars supervised by faculty (divisional members and invited faculty). The residents are required to read on topics not covered by the teaching sessions. A. Clinical Rotations Twelve months of core critical care clinical training occur in the ICUs at the primary teachings sites. The elective rotations in the specialty ICUs (Neurosciences ICU, Cardiovascular ICU, Pediatric ICU, and Coronary Care Unit) provide clinical experience that may not be available in the general ICUs. Elective rotations in medical subspecialties (Pulmonary, Nephrology, Infectious Diseases) and surgical subspecilaties (Trauma, Thoracic Surgery, General Surgery) are available. B. Formal academic activities residents are required to attend. Critical Care Teaching Sessions (Wednesday 1:30 - 3:30 PM) - weekly at UAH or RAH ICU Teleconference Grand Rounds (Tuesdays 4:30-5:30PM) - monthly ICU Joint Practice Meeting (Thursdays 2:00-3:00PM, UAH rotation) – weekly ICU Mortality, Morbidity, Quality Improvement Meeting (UAH rotation) – 8 times/year Faculty wide CanMEDS sessions (3 to 4 times a year) Critical Care Residents Day & Toronto Critical Care Symposium – all1st yr , some 2nd yr National ACES Course – all 1st year trainees attend Journal Club (every second month) – all attend Canadian Critical Care Review Course – final year residents attend ATLS – all complete C. Other recommended organized scholarly activities Alberta Society of Intensive Care Physicians Meeting at Lake Louise Teaching Enhancement Course (when course offered) Internal Medicine CanMEDS Workshop (when positions are available) Pediatric teaching sessions Combined Obstetrics and Gynecology teaching sessions Trauma Rounds (monthly on Thursday 4:30-5:30PM at UAH) Quality Improvement Lectures - Capital Health (twice a year) “Putting Evidence into Practice Workshop” (annually) Evaluation For clinical skills, including knowledge base: Qualitatively, during the ICU rotations: o ICU bedside rounds, ICU admissions, ICU consultations Quantitatively, using the o In training written and case scenario exams (twice a year) o SCCM MCCKAP Exam (yearly) For technical skills: Qualitatively, residents are supervised during the following situations: o ACES Course (Acute Critical Events Simulation) University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program o Bronchoscopy and Anesthesia elective rotations. o Performance of tracheostomies in the ICU. o ICU rotations - procedures are supervised until the resident is able to proceed by himself. Quantitatively, a “skills log” of procedures performed is maintained by the residents. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program B. COMMUNICATOR (from RCPSC training requirements) General Requirements The adult critical care medicine resident must be able to: a) Establish relationships with patients/families; b) Listen effectively; c) Obtain and synthesize relevant history from patients/families/communities; and d) Discuss appropriate information with patients/families and the health care team. Specific Requirements a) Assess, communicate with, and support patients and families confronted with critical illness. b) Explain life-sustaining therapies, in clear language, and describe the expected outcome of such therapies in view of the patient’s goals and wishes. c) Know and understand the consequences of the language used to impart information. d) Be acquainted with the unique stressful environment of the critical care milieu for patients and their families. e) Demonstrate respect and understanding for the role of other team members in communicating and facilitating decision-making with critically ill patients and their families. f) Communicate effectively with families who may be dysfunctional, angry, confused, or litigious. g) Explain the concept of brain death and organ donation, in clear language. Learning Opportunities and Evaluation During the ICU rotations there is daily interaction with patients, families, consulting physicians and ICU team members, including: nurses, respiratory therapists, dieticians, pharmacists, social workers and chaplains. The resident observes how ICU attending staff conducts ICU team meetings, ICU bedside rounds and family conferences. Residents participate initially as observers in family conferences where end of life issues is discussed. During their second year of training, residents often lead the discussion at family conferences with attending staff present. The following instances are used to assess the resident’s communication skills: During patient or family conferences, when the resident leads the discussion on the following issues: o End-of-life decision making, difficult consents, breaking bad news o Residents are expected to complete at least three guided self evaluations during each core ICU rotation. During team meetings and bedside rounds During telephone consultations with peripheral hospitals. Residents are expected to complete at least two evaluation feedback forms during each of their core ICU rotations. During academic presentations During written communication: o Clinical notes, consultation reports, discharge summaries During simulated situations: o Case scenario in-training exams where communication with a referring physician occurs o At the ACES Course when residents are observed/videotaped during acute critical events simulation o During scheduled simulation sessions The evaluations of communications skills are witnessed interactions by the preceptors. These are documented on the in training evaluation report (ITER). Feedback is provided at the end of the rotation or at the six monthly meeting with the Program Director. If significant concern exists, the ICU attending and or Program Director addresses the issue during the rotation. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program C. COLLABORATOR (from RCPSC training requirements) General Requirements The adult critical care medicine resident must be able to: a. Consult effectively with other physicians and health care professionals; and b. Contribute effectively to interdisciplinary team activities. Specific Requirements a. Contribute to productive communication and cooperation among colleagues in all aspects of education, service, and research, as they impact on the critical care environment, recognizing the multi-disciplinary nature of the specialty. b. Demonstrate knowledge and skill in preventing and resolving conflict. c. Demonstrate leadership in the continuing education of members of the multi-disciplinary health care team. Learning Opportunities and Evaluation The model of care in the ICU is team based and multidisciplinary. There are daily ICU team meetings and ICU bedside ward rounds that involve the medical staff, nurses, respiratory therapist, pharmacist, dietician, and occupational therapist. The attending staff or critical care resident generally “leads” the ICU team discussion on ICU bedside rounds. The daily interaction with ICU team members and supporting services provide ample opportunities for the resident to learn (by observation of the attending staff) and to be evaluated by the attending staff. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program D. MANAGER (from RCPSC training requirements) General Requirements The adult critical care medicine resident should be able to: a. Allocate finite health care resources wisely; b. Work effectively and efficiently in a health care organization; c. Utilize information technology to optimize patient care, life-long learning, and other activities d. Utilize personal resources effectively to balance patient care, learning needs, and outside activities. Specific Requirements a. Be familiar with the administrative organization required to operate an Intensive Care Unit (ICU) within an acute urban or rural hospital. b. Be knowledgeable regarding unit staffing requirements, skills, education, and organization. c. Be able to evaluate and cooperatively determine unit equipment requirements. d. Be able to manage the clinical, academic, and administrative affairs of an ICU e. Demonstrate the ability to acquire, interpret, synthesize, record, and communicate f. (written and verbal) clinical information in managing health problems in the critical care setting. Effective lead a team of residents through the day to day operations of the critical care unit. Learning Opportunities and Evaluation The residents are provided with teaching sessions on ICU administration. CanMEDS topics are regularly included in the educational program at the national critical care residents’ day, During the ICU rotation the resident has ample opportunities to “manage the ICU as a junior consultant” and to make daily triage decisions regarding ICU admissions and discharges (allocation of scarce clinical resources). At UAH the following meetings occur: Weekly joint practice meetings where day to day management issues such as ICU staffing, new equipment, policies and procedures, clinical protocols and point of care testing are discussed Mortality, Morbidity & Quality Improvement Rounds (8 times a year) where mortality cases are reviewed, concerns raised by other departments are discussed, and quality improvement projects are initiated. When on ICU rotation at UAH, residents are required to attend the joint practice meetings, and to present cases at the mortality, morbidity and quality improvement meetings. The resident also participates in the following: Scheduling of the city wide journal club Scheduling and conflict resolution of the junior residents on the ICU team An elective rotation is available to gain experience at a community hospital ICU. Evaluation of the “Manager Role” occurs in the above settings and is documented on the in training evaluation report. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program E. HEALTH ADVOCATE (from RCPSC training requirements) General Requirements The adult critical care medicine resident should be able to: a. Identify the important determinants of health affecting patients; and b. Contribute effectively to the improved health of patients and communities. Specific Requirements a. Understand, in general, the diverse determinants of health, disease, and illness, and relate occupational and environmental exposures, socio-economic factors, and life style factors to critical illness. b. Understand, in general, the health care system and more specifically the structure, function, and financing of critical care units. c. Understand the importance of medico-legal considerations for the critically ill. d. Be able to communicate to the general population critical care issues and their impact on the maintenance and improvement of health care. Learning Opportunities and Evaluation During the ICU rotation the resident is provided with opportunities to advocate for individual patients under their care, for example: In relation to resource allocation: When discussing with a radiologist why a CT scan is required during a weekend for the management of his patient or a specific laboratory test is required on an urgent basis In relation to obtaining appropriate support following discharge When seeking the appropriate consult service to provide follow up for a patient discharged from the ICU, such as a consult to a psychiatrist for a suicidal patient In relation to awareness of financial barriers to care Use of expensive medications and technology The resident has the opportunity to advocate for individual patients or for all patients in the ICU at: ICU team meetings and ICU bedside rounds where the individual patient’s care is discussed Joint practice meetings where ICU policies and procedures are discussed Mortality, Morbidity and Quality Improvement Meetings During attendance at provincial and national society meetings (where policy statements for the critical care patient population in general are formulated) the resident has the opportunity to advocate for the ICU population at large. The resident is assessed subjectively when acting as an “advocate” in the following settings: During ICU bedside rounds when requesting tests, procedures or consultations, for individual patient under his care During joint practice meetings when requesting policy changes and ICU equipment/technology for all patients the in the unit The role of “Health Advocate” is assessed by the rotation preceptors during the above settings and documented on the rotation in training evaluation report. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program F. SCHOLAR (from RCPSC training requirements) General Requirements The adult critical care medicine resident should be able to: a. Facilitate the learning of patients/families, house staff/students and other health professionals; b. Contribute to the development of new knowledge; and c. Develop, implement, and monitor a personal continuing education strategy. Specific Requirements a. Demonstrate the expertise necessary for rational use of the principles of “evidence based medicine” in both clinical and research settings. b. Demonstrate the expertise to competently appraise: o Levels of evidence; Interventions; Diagnostic tests; Prognosis; and o Integrative literature (meta-analyses, practice guidelines, decision and economic analyses). c. Demonstrate a basic understanding of biostatistics, study design, protocol writing, and manuscript preparation. d. Demonstrate the ability to efficiently access information from the medical literature using current information retrieval tools. e. Practice the principles of adult learning and help others learn by providing guidance constructive feedback. f. Be familiar with the concepts of basic applied research and epidemiology, in order to capably evaluate newer forms of therapy. Learning Opportunities and Evaluation 1. Teaching Skills Residents attend a workshop on teaching enhancement skills. The two-day work shop topics include: o o o Teaching behaviours, educational objectives, classroom lecture questioning, Lecturing to large classes, problem-based learning, bedside teaching Oral and poster presentations, technology in learning, designing audience response items It is expected that the resident will teach the junior residents, medical students, and nurses during the ICU rotation (ICU bedside rounds, ICU admissions, supervision of procedures, ICU Grand Rounds and mortality case presentations). 2. Biostatistics and critical appraisal relevant to the interpretation the literature: Residents are provided with: o Teaching sessions and funding to attend workshops – “Putting Evidence into Practice” Residents: o Prepare and present at journal club o Submit journal reviews for the Canadian Journal of Anesthesia “Best Evidence in Critical Care Medicine” 3. Development of skills in self-assessment and self-directed life-long learning Residents are encouraged to “research” and read on specific topics during the course of providing care for their patients in a manner similar to the “Structured Learning Project” of the Royal College MOCOMP process. University of Alberta Division of Critical Care Medicine Adult Critical Care Medicine Resident Training Program G. PROFESSIONAL (from RCPSC training requirements) General Requirements The adult critical care medicine resident should be able to: a. Deliver the highest quality care with integrity, honesty, and compassion; b. Exhibit appropriate personal and interpersonal professional behaviours; and c. Practice medicine ethically consistent with the obligations of a physician. Specific Requirements a. Be aware of, and understand, moral and ethical issues as they impact on patients, their families, and critical care providers. b. Understand the role and responsibilities of the critical care physician at the local, regional, and national levels. c. Develop and demonstrate use of a framework for recognizing and dealing with ethical issues in clinical and/or research practice including truth-telling, consent, conflict of interest, resource allocation, and end-of-life care. Learning Opportunities and Evaluation Biomedical ethics Teaching sessions on biomedical ethics that are critical care specific are provided. The seminar supervisors include a critical care physician with a specific interest in clinical bioethics and a clinical ethicist for the University Hospital. Ethics Committee members are also available for ICU consultations as requested. Medical legal issues Specific teaching sessions are arranged with the University of Alberta, Legal Faculty. Teaching sessions also occur at the following resident education programs and meetings: Alberta Society of Intensive Care Physicians (Lake Louise) National Critical Care Residents Day Attendance at conferences Residents are funded to attend a national or international conference and usually attend the annual national Critical Care Residents Day and the Toronto Critical Care Medicine Symposium. The resident may also choose to attend other conferences such as SCCM, ACP, ATS or the International Symposium of Intensive Care and Emergency Medicine in Brussels. If the resident is presenting a research paper an additional conference is funded. Residents are also funded to attend the annual Alberta Society of Intensive Care Physicians Meeting in Lake Louise, Alberta. Participation in national and international professional societies The residents are encouraged to participate in the following societies: Alberta Society of Intensive Care Physicians Canadian Critical Care Society Royal College of Physicians and Surgeons of Canada Societies related to the resident’s base specialty (e.g. American College of Chest Physicians) The resident’s behaviour and professional attitudes during ICU rotations is observed by the preceptors and senior nursing staff (charge nurse) and a qualitative assessment is recorded on the in training evaluation report. Learning Resources Bioethics: http://rcpsc.medical.org/ethics/index.php