1. Hypertensive crisis was developed in patient. Which drugs can be
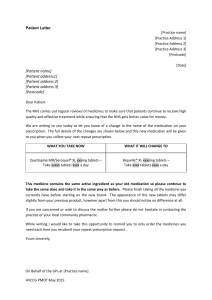
advertisement

MINISTRY OF PUBLIC HEALTH OF UKRAINE MINISTRY OF EDUCATION, SCIENCE, YOUTH AND SPORTS OF UKRAINE SUMY STATE UNIVERSITY 3078 METHODOLOGICAL INSTRUCTIONS for practical training on the topic “DRUGS AFFECTING PERIPHERAL AND CENTRAL NERVOUS SYSTEM” in Pharmacology course for foreign students of speciality 7.110101 «Medical science» full-time training Sumy Sumy State University 2011 3 Methodological instructions for practical training on the topic “Drugs affecting peripheral and central nervous system” / compiler A.A. Kachanova. – Sumy : Sumy State University, 2011. – 46 p. 4 Biological chemistry and pharmacology departmentThematic Module “Drugs Affecting Peripheral Nervous System” Drugs Affecting the Afferent Innervation Topical questions 1. The classification of drugs affecting the afferent innervation. 2. The classification of local anesthetics according to chemical structure. 3. The types of local anesthesia. Primary use of local anesthetics for this or that type of local anesthesia. 4. The mechanism of action of local anesthetics. 5. Expediency of combination of local anesthetics with adrenoceptor agonists. 6. The comparison characteristics of local anesthetics: duration of anesthesia, clinical use, influence on the central nervous system and internals, biotransformation in organism, and side effects. 7. Astringent drugs: classification, mechanism of action, local effects, and clinical use. 8. The characteristic of covering drugs and adsorbents: mechanism of action, local effects, and clinical use. 9. Irritant drugs: mechanism of action, effects, and clinical use. Tasks for prescription Prescribe the following drugs and list the indications for their use: 1. Novocaine (procaine) in ampoules for different types of anesthesia. 2. Anesthesin (benzocaine) in suppositories, powders for internal use, in ointment. 3. Lidocaine in ampoules for different types of anesthesia. 4. Trimecaine in ampoules for different types of anesthesia. 5. Tannin in ointment and in solution for the gastric lavage at a poisoning. 6. Bismuth subnitrate in tablets, ointment and powders for external use. 7. Activated charcoal (Carbo activatus) in tablets and non-dosage powders for internal use. 5 8. Menthol in alcoholic solution and in ointment. Table 1 – Drugs for prescription Drug name Anaesthesinum Novocainum Trimecainum Lidocainum 6 Single dose and mode of administration Orally 0.3 g through rectum 0.05–0.1 g; on the skin 5–10% ointment Drug product Powder; tablets 0.3 g; suppositories 0.05 and 0.1 g; 5% ointment For infiltration anesthesia Ampoules 0.25% and 0.25-0.5% solution; 0.5% solution – 1, 2, for conduction anesthesia 1– 5, 10 and 20 ml; 1% 2% solution; and 2% solution – 1, for permeation anesthesia 2, 5, and 10 ml; 10–20% solution and 5–10% bottle 200 or 400 ml ointment; of 0.25% or 0.5% through rectum – solution; suppository containing 0.1 g suppositories 0.1 g; 5% and 10% ointments For infiltration anesthesia – Ampoules 10 ml of 0.125%, 0.25% or 0.5% 0.25% solution; 2, 5, solution; or 10 ml 0.5% or 1% for conduction anesthesia – solution; 1, 2, 5, or 1–2% solution; 10 ml 2% solution; for permeation anesthesia – 1 or 2 ml 5% solution 2–5% solution; for epidural anesthesia – 1–2% solution; for spinal anesthesia – 5% solution For infiltration anesthesia – Ampoules 10 or 20 ml 0.25% or 0.5% solution; of 1% solution; 2 or for conduction anesthesia – 10 ml of 2% solution; 0.5–2% solution; 2 ml of 10% solution for permeation anesthesia – 1–5% solution Table 1 continuation Tanninum For oral, nasal, a pharyngeal rinsing, and throat gargling – 1–2% water or glyceric solutions; for application on injured surfaces – 3–10% solution or ointment; for gastric lavage – 0.5% solution Bismuthi subnitras Orally – 0.25–0.5 g; on the skin – 5–10% ointment and aspersion Carbo activatus Orally – 1–2 g for meteorism; 20–30 g (in the form of suspension in water) for poisonings Mentholum For applying on the skin – 0.5–2% alcoholic solution, 1% ointment; sublingually – 2–3 drops of 5% alcoholic solution (on a slice of sugar) There are no made forms at the plant. Pharmacist prepares these forms (the prescriptions can be written in short or full forms) Powder; tablets 0.25 or 0.5 g; 10% ointment Powder; tablets 0.25 or 0.5 g 1%, 2% or 5% alcoholic solution; 1% ointment Cholinomimetics. Cholinesterase Inhibitors Topical questions 1. The types of efferent nerves. The peculiarities of structure and physiology of vegetative nervous system. 2. The structure and work of cholinergic synapse. Different types of cholinoceptors and their localization. 3. The classification of cholinergic drugs depending on their influence upon different types of cholinoceptors. 4. Direct M-, N-cholinomimetics: mechanism of action, pharmacological effects, peculiarities of pharmacokinetics, clinical applications, adverse effects. 7 5. Cholinesterase inhibitors: drugs classification, mechanism of action, pharmacological effects, peculiarities of pharmacokinetics, clinical applications, adverse effects. The symptoms and treatment of poisoning with cholinesterase inhibitors. Mechanism of action of cholinesterase regenerators; peculiarities of their use. 6. M-cholinomimetics: mechanism of action, pharmacological effects, peculiarities of pharmacokinetics, clinical applications, and adverse effects. The comparison characteristics of pilocarpine and aceclidine. 7. N-cholinomimetics: mechanism of action, pharmacological effects, peculiarities of pharmacokinetics, clinical applications. The toxicology of nicotine. The treatment of nicotine abuse. Situational tasks in pharmacodynamics and pharmacokinetics 1. An eye was denervated. Describe the carbacholine effects on this eye. 2. An eye was denervated. Describe the proserin effects on this eye. 3. M-cholinoceptor antagonist was administered to animal. Describe the change in its blood pressure owing to the following acetylcholine administration. 4. M- cholinoceptor antagonist was administered to animal. Describe the change in its blood pressure owing to the following proserin administration. 5. The doctor has 3 preparations. All of them are miotic, reduce intraocular pressure, cause bradycardia, and increase glands secretion and tone of smooth muscles. Two preparetions also have an ability to ease the neuromuscular transmission and transmission through autonomic ganglia. But one of them acts in full loss of function, while another – only in decreased function. What groups do these drugs belong to? 6. Patient with poisoning was hospitalized with the following symptoms: profuse sweating, myosis, nausea, vomiting, diarrhea, and bradycardia. Blood pressure is low. What is the cause of poisoning? Institute treatment for this patient. 7. The side effects in digestive system and in bronchi develop in patient suffering from myasthenia that is treated with proserin. What are these side effects? What drug should be administered for prevention of these side effects? 8. A patient suffers from glaucoma. What drugs may be used for reduction of intraocular pressure? Explain the mechanism of drugs action. 8 9. A patient suffers from myasthenia. Choose drugs for treatment of patient. Explain the mechanism of drugs action. Tasks for prescription Prescribe the following drugs and list indications for their use: 1. 2. 3. 4. 5. 6. 7. 8. Proserin in tablets, eye drops, and ampoules. Galantamine in ampoules. Pilocarpine in eye drops and eye ointment. Aceclidine in ampoules, eye drops, and eye ointment. Carbacholine in eye drops. Dipiroxim in ampoules. Lobeline in ampoules. Cytitonum in ampoules. Fill in the following tables Table 2 – Localization of cholinergic synapses and cholinoceptors Synapses localization Receptors localization M-cholinoceptor N-choliniceptor Synapses of sympathetic and parasympathetic ganglia Synapses of sympathetic fibers in adrenal medulla Carotid bodies Synapses of postganglionic parasympathetic fibers in innervated organs Synapses of postganglionic sympathetic fibers in genital glands and vessels of skeletal muscles Synapses of motor nerves in skeletal muscles Synapses of central nervous system 9 Table 3 – Organs reaction upon the excitation of vegetative nerves Organ, tissue, function Change of function owing to excitation of sympathetic nerve parasympathetic nerve Heart: - heart rate; - force of cardiac contraction; - automatism; - conductibility Vessels Smooth muscles: - bronchi; - gastrointestinal tract; - urinary tract; - biliary tract; - uterus; - sphincters of GIT Excretory glands activity Eye muscles: - muscle – sphincter of pupil; - radial muscle; - ciliary muscle Table 4 – Comparison characteristics of M-cholinomimetics Effect Reduction of intraoccular pressure Increase of tone and peristalsis of intestine Increase of tone and contractibility of uterus Increase of secretion of excretory glands Bradycardia Indications for use “+” – weak effect; “++” – moderate effect; “+++” – marked effect 10 Pilocarpine Aceclidine Table 5 – Comparison characteristics of cholinesterase inhibitors Physostigmine Proserin Galantamine Armin Mode of administration Duration of action Indications for use Symptoms of poisoning Antidotes Table 6 – Drugs for prescription Drug name Proserinum Single dose and mode of administration Orally 0.01–0.015 g; subcutaneously 0.0005 g; in eyes 1–2 drops Galanthamini Subcutaneously 0.0025–0.005 g hydrobromidum Pilocarpini In eyes: 1–2% solution (1–2 hydrochloridum drops) or eye ointment Aceclidinum In eyes: 2-5% solution (1–2 drops) or 3–5% eye ointment; subcutaneously 0.002 g Carbacholinum In eyes 1–2 drops of 0.5–1% solution Dipiroximum Subcutaneously, intramuscularly or intravenously 0.15–0.3 g Intravenously slowly 0.005 g Lobelini hydrochloridum Cytitonum Intravenously slowly 0.5 ml Drug product Tablets 0.015 g; ampoules 1 ml of 0.05% solution; eye drops: 0.5% solution Ampoules 1 ml of 0.1%, 0.25%, 0.5% or 1% solution Eye drops: 1% or 2% solution in bottles 5 or 10 ml; 1% or 2% eye ointment 2-5% solution of eye drops; 3% and 5% eye ointment; ampoules 1 or 2 ml of 0.2% solution Eye drops: 0.5% or 1% solution in bottles 5 or 10 ml Ampoules 1 ml of 15% solution Ampoules 1 ml of 1% solution Ampoules 1 ml 11 M-Cholinoceptor Antagonists Topical questions 1. Types and localization of M-cholinoceptors. The effects of excitation of different M-cholinoceptors types. 2. Classification of М-cholinoceptor antagonists. 3. The mechanism of action of М-cholinoceptor antagonists. 4. Influence of М-cholinoceptor antagonists upon the eye. 5. Influence of М-cholinoceptor antagonists upon cardiovascular system. 6. Influence of М-cholinoceptor antagonists upon the smooth muscular organs (the gastrointestinal tract, bronchi, and urinary ways). 7. Influence of М-cholinoceptor antagonists upon the functions of excretory glands. 8. Central effects of М-cholinoceptor antagonists (influence upon CNS). 9. The comparison characteristics of М-cholinoceptor antagonists (peculiarities of atropine, scopolamine, platyphyllin, methacin). 10. Indication for application of М-cholinoceptor antagonists. 11. Adverse effects of М-cholinoceptor antagonists and contraindications to their use. 12. The symptoms and treatment of poisoning with М-cholinoceptor antagonists. Situational tasks in pharmacodynamics and pharmacokinetics 1. An eye was denervated. Describe the effects of pilocarpine and atropine on this eye. 2. A child with poisoning was hospitalized with the following symptoms: tachycardia, marked mydriasis, dry mouth, agitation, and hallucinations. What substance is the cause of poisoning? Institute treatment for this child. 3. A patient suffers from spastic pain owing to urolithiasis. What drugs may be used for pain relief of spasm? Explain mechanism of drugs action. 4. A patient suffers from atrioventricular blockade. What drugs may be used for improving of conductivity? 5. A patient with ulcer disease suffers from hypersecretion and pain owing to pylorus spasm. Propose drugs for treatment of this patient. Explain the mechanism of drugs action. 12 Fill in the following table Table 7 – Comparison characteristics of М-cholinoceptor antagonists effects Effects Drug Atropine Scopolamine Platyphyllin Methacin Relaxation of bronchi Decrease of bronchial and digestive glands secretion Reduction of spasm of intestine, biliary and urinary tracts Degree of М-cholinoceptor antagonists action Direct myotropic antispasmodic action Tachycardia Reduction of vestibular disturbances Antiparkinsonian action Mydriasis Duration of paralysis of accommodation Indications for use “+” – weak action; “++” – moderate action; “+++” – marked action. Tasks for prescription Prescribe the following drugs and list indications for their use: 1. Atropine in tablets, ampoules, eye ointment, and eye drops. 2. Dry extract of belladonna. 3. Scopolamine in powders, ampoules, and eye drops. 4. Platyphyllin in ampoules and tablets. 5. Methacin in tablets and ampoules. 6. “Aeron” in tablets. 13 Table 8 – Drugs for prescription Drug name Atropini sulfas Extractum Belladonnae siccum Scopolamini hydrobromidum Platyphyllini hydrotartras Methacinum Tablets “Aeronum” 14 Single dose and mode of administration Orally 0.00025–0.0005 g 1-3 times daily; subcutaneously or intramuscularly 0.00025– 0.0005 g 1-2 times daily; intravenously 0.00025– 0.0005 g; in eyes: 1% ointment or 1–2 drops of 0.5–1% solution (once daily) Orally 0.02–0.04 g 2-3 times daily; Through rectum 0.02–0.04 g 1–2 times daily Orally or subcutaneously 0.00025g; in eyes: 1–2 drops of 0.25% solution 1–2 times daily Orally 0.003–0.005 g 2–3 times daily; subcutaneously 0.002–0.004 g 1-2 times daily; in eyes: 1–2 drops of 1–2% solution Orally 0.002–0.004 g 2–3 times daily; subcutaneously, intramuscularly or intravenously 0.0005–0.001 g 1–2 times daily Orally 1–2 tablets before or during travel (for treatment or prevention of motion sickness) Drug product Tablets 0.0005 g; ampoules 1 ml of 0.1% solution; eye drops: 0.5% or 1% solution; 1% eye ointment Powders for internal use; suppositories 0.02 or 0.04 g Powders for internal use; ampoules 1 ml of 0.05% solution Tablets 0.005 g; ampoules 1 ml of 0.2% solution; eye drops 1% or 2% solution Tablets 0.002 g; ampoules 1 ml of 0.1% solution Tablets (10 tablets in package) N-Cholinoceptor Antagonists: Ganglionic Blocking Drugs and Skeletal Muscle Relaxants Topical questions 1. Types and localization of N-cholinoceptors. 2. Classification of ganglionic blocking drugs. 3. The mechanism of action of ganglionic blocking drugs. 4. Pharmacological effects of ganglionic blockers: - influence on the cardiovascular system; - influence on the smooth muscular organs (digestive tract, bronchi, and urinary ways); - influence on the eye functions; - central effects of ganglionic blocking drugs (influence on CNS). 5. Indications for application of ganglionic blocking drugs. 6. Adverse effects of ganglionic blockers and contraindications to their use. 7. The classification of skeletal muscle relaxants. 8. Characteristics of nondepolarizing muscle relaxants: mechanism of action, clinical use, and adverse effects. 9. Characteristics of depolarizing drugs: peculiarities of mechanism of action, clinical use, and adverse effects. Situational tasks in pharmacodynamics and pharmacokinetics 1. Benzohexonium was administered to animal. Describe the effects of the following aceclidine administration to this animal. 2. Benzohexonium was administered to animal. Describe the influence of cytitonum on blood pressure and respiration. 3. Benzohexonium was administered to animal. Describe the influence of atropine on bronchi and intestine. 4. A doctor administered proserin to patient with overdose of dithylinum. Were his actions correct? Why? 5. A doctor administered proserin to patient with overdose of tubocurarin chloride. Were his actions correct? Why? 15 Fill in the following tables Table 9 – Comparison characteristics of ganglionic blockers Hygronium Benzohexonium Pachycarpine Mode of drug administration Duration of action Penetration power through blood-brain barrier Indications for use Side effects Table 10 – Comparison characteristics of peripheral myorelaxants Dithylinum Tubocurarin chloride Peculiarities of chemical structure Mechanism of action Interaction with cholinesterase inhibitors Duration of action Mode of administration Indications for use Side effects Tasks for prescription Prescribe the following drugs and list indications for their use: 1. Benzohexonium in tablets and ampoules. 2. Pirilenum in tablets. 3. Pentaminum in ampoules. 16 4. Hygronium in ampoules and bottles. 5. Tubocurarine in ampoules. 6. Dithylinum in ampoules. Table 11 – Drugs for prescription Drug name Benzohexoniu m Pirilenum Pentaminum Hygronium Tubocurarini chloridum Dithylinum Single dose and mode of administration Orally 0.1–0.2 g 3–6 times daily; subcutaneously or intramuscularly 0.025 g 1–2 times daily Orally 0.0025–0.005 g 2–5 times daily Intramuscularly 0.05–0.1 g 2–3 times daily; intravenously slowly 0.01–0.025 g (before administration, single dose should be mixed with 20 ml of sterile isotonic sodium chloride solution or glucose solution) Intravenous drop by drop 0.04– 0.08 g (as 0.1% solution) Drug product Tablets 0.1 g; ampoules 1 ml of 2.5% solution Tablets 0.005 g Ampoules 1 or 2 ml of 5% solution Ampoules or bottles 0.1 g of dry medicinal remedy Intravenously 0.0004–0.0005 g/kg Ampoules 1 ml of 1.5% solution Intravenously 0.0015–0.002 g/kg Ampoules 5 or 10 ml of 2% solution 17 Adrenomimetic and Sympathomimetic Drugs Topical questions 1. The structure and functions of adrenergic synapse. 2. The types of adrenoceptors. The basic localization and physiological meaning of different types of adrenoceptors. 3. Classification of drugs stimulating adrenergic receptors. 4. Pharmacological characteristics of adrenaline: - mechanism of action; - influence on cardiovascular system; - influence on eye; - influence on smooth-muscular organs (gastrointestinal tract, bronchi, uterus); - influence on metabolic processes; - influence on CNS; - peculiarities of pharmacokinetics; - indication for application; - adverse effects and contraindications. 5. Pharmacological characteristic of noradrenaline. 6. Classification of α-adrenomimetics according to influencing on different subtypes of α-adrenoceptors. Pharmacological effects and clinical use of α-adrenomimetics. 7. Classification of β-adrenomimetics according to influencing upon different subtypes of β-adrenoceptors. Pharmacological effects, clinical use, and adverse effects of β-adrenomimetics. 8. The characteristics of sympathomimetic drugs. Features of the mechanism of ephedrine action. Force and duration of ephedrine effects in comparison with adrenaline. Tachyphylaxis concept. The indications and contraindications to use. Situational tasks in pharmacodynamics and pharmacokinetics 1. What groups and certain drugs are used for prevention of bronchial asthma attacks? Explain your answer. 2. What groups and certain drugs are effective in atrio-ventricular blockage? Explain your choice. 3. A patient suffers from glaucoma. The use of cholinomimetics is contraindicated owing to concomitant ulcer disease of stomach. What drugs may be used for treatment of glaucoma in this patient? Explain the mechanism of drugs action. 18 4. A patient with frequent bronchial asthma attacks used inhalations of adrenomimetic agent for its reduction. In several days, patient began to complain of tachycardia, chest pain, tremor, and headache. Which drug does cause such complications? Explain the mechanism of complications development. 5. Acute vascular insufficiency was developed in a patient. For improvement of this state, doctor has the following drugs: cytitonum, adrenaline, and noradrenaline. Which drug should be administered? Why? Which mode of drug administration should be chosen? Tasks for prescription Prescribe the following drugs: 1. Adrenaline in ampoules and eye drops. 2. Noradrenaline in ampoules. 3. Ephedrine hydrochloride in ampoules and tablets. 4. Mesatonum (phenylephrine) in ampoules and tablets. 5. Naphthizin in drops for nose. 6. Isadrinum in tablets and solution for inhalations. 7. Salbutamol in tablets and aerosol. Fill in the following tables Table 12 – Effects of excitation of alpha- and beta-adrenergic receptors Tissue, organ Excitation Alpha-adrenoceptor Beta-adrenoceptor Heart Bronchial smooth muscles Smooth muscles of vessels Smooth muscles of intestine Uterus Radial muscle of iris Bladder Salivary glands Liver Adipocytes Platelets 19 Table 13 – Comparison characteristics of adrenomimetics Drug Alpha-adrenomimetic action Beta-adrenomimetic action Noradrenaline Adrenaline Mesatonum Isadrinum Ephedrine Table 14 – Comparison characteristics of pharmacological effects of adrenomimetics Effect Cardiac pacing Influence on blood pressure Broncholytic action Influence on carbohydrate metabolism Excitation of CNS 20 Adrenaline Noradrenaline Mesatonum Isadrinum Ephedrine Table 15 – Drugs for prescription Drug name Adrenalini hydrochloridum Noradrenalini hydrotartras Ephedrini hydrochloridum Mesatonum Naphthyzinum Isadrinum Salbutamol Single dose and mode of administration Subcutaneously or intramuscularly 0.0003– 0.00075 g; in eyes: 1-2 drops of 1–2% solution Intravenously drop by drop 0.004–0.008 g in 1 L of 5% glucose solution Orally, subcutaneously, intramuscularly or intravenously 0.025 g 2–3 times a day Orally 0.01–0.025 g 2–3 times daily; subcutaneously or intramuscularly 0.003–0.005 g 1-2 times daily; intravenously 0.001–0.003 g with 40 ml of sterile isotonic NaCl solution; in eyes: 1–2 drops of 1–2% solution In nose 1–2 drops of 0.05– 0.1% solution 3 times daily Sublingually 0.005 g; inhalationly: 1–2 inhalations of 0.5-1% solution Orally 0.002 g 3 times daily; inhalationly: 1–2 inhalations 3 times daily Drug product Ampoules 1 ml of 0.1% solution; eye drops: 1% or 2% solution Ampoules 1 ml of 0.2% solution Tablets 0.025 g; ampoules 1 ml of 5% solution Powders for internal use; ampoules 1 ml of 1% solution; eye drops 1% or 2% solution Bottles 10 ml of 0.05% or 0.1% solution Tablets 0.005 g; bottles 25 ml or 100 ml of 0.5% or 1% solution Tablets 0.002 g; aerosol 10 ml 21 Adrenoceptor Antagonists Topical questions 1. The structure and function of adrenergic synapse. 2. The types of adrenoceptors. The basic localization and physiological meaning of different types of adrenoceptors. 3. Classification of adrenoceptor blocking drugs. 4. Pharmacological characteristics of -adrenoceptor blocking drugs: classification according to influence on different kinds of -adrenoceptors, mechanism of action, phenomenon of “epinephrine reversal”, influence on cardiovascular system, indications for application, adverse effects. 5. Pharmacological characteristics of -receptor antagonists: classification according to influence on different kinds of -adrenoceptors, mechanism of action, influence on cardiovascular system, metabolic processes, and eye, indications for application, adverse effects. The concept of intrinsic sympathomimetic activity and membrane-stabilizing action of -adrenergic antagonists. 6. -, -adrenergic antagonists: representatives, mechanism of action, pharmacological effects, clinical use, and adverse effects. 7. Sympatholytics: representatives, mechanism of action, pharmacological effects, indications for use, and adverse effects. Situational tasks in pharmacodynamics and pharmacokinetics 1. Hypertensive crisis was developed in patient. Which drugs can be used for quick blood pressure reduction? 2. A patient suffers from obliterative endarteritis. Which drugs should be prescribed to him for reduction of vascular spasm? Explain your answer. 3. Administration of which groups of drugs may trigger asthma attacks? 4. An elderly patient suffers from ischemic heart disease with marked atherosclerosis of coronary vessels. Which drugs should be prescribed to him for prevention of heart strokes? Substantiate your answer and explain mechanism of drugs action. 22 Fill in the following tables Table 16 – Comparison characteristics of adrenoceptor antagonists and sympatholytics Drug name Main effects Indication for use Side effects Phentolamine Tropaphenum Propranolol Octadinum Reserpine Tasks for prescription Prescribe the following drugs: 1. Phentolamine in tablets. 2. Tropaphenum in ampoules. 3. Prazosin in tablets. 4. Propranolol in tablets and ampoules. 5. Metoprolol in tablets and in ampoules. 6. Talinolol in dragee. 7. Octadinum in tablets. 8. Reserpine in tablets. Table 17 – Drugs for prescription Drug name Phentolamini hydrochloridum Tropaphenum Prazosinum Single dose and mode of administration Orally 0.05 g 3–5 times daily Subcutaneously or intramuscularly 0.01–0.02 g 1–3 times daily; intravenously 0.01 g Orally 0.0005–0.002 g 3–4 times daily Drug product Tablets 0.025 g Ampoules 0.02 g of dry medicinal remedy (before administration, substance of 1 ampoule should be dissolved in 1–2 ml of sterile water) Tablets 0.001, 0.002 or 0.005 g 23 Table 17 continuation Anaprilinum Orally 0.01–0.04 g 3–4 times daily; intravenously slowly 0.001 g Metoprololum Orally 0.05–0.1 g 2–4 times daily; intravenously slowly 0.005– 0.015 g Talinololum Orally 0.05–0.1 g 3 times daily Octadinum Orally 0.025–0.05 g once daily Reserpinum Orally 0.00005–0.0001 g 1-3 times daily Tablets 0.01 or 0.04 g; ampoules 1 or 5 ml of 0.1% solution Tablets 0.05 or 0.1 g ampoules 5 ml of 1% solution Dragee 0.05 g Tablets 0.025 g Tablets 0.0001 or 0.00025 g General Anesthetics Topical questions 1. What is “general anesthesia”? The characteristics of general anesthesia stages. 2. The different types of general anesthesia: initial anesthesia, basis anesthesia, combined anesthesia. 3. The classification of general anesthetics. 4. Peculiarities of mechanisms of action of different drugs from general anesthetics group. 5. The characteristics of some drugs for inhalational anesthesia: ether, halothane, nitrous oxide. 6. The characteristic of some drugs for intravenous anesthesia: propanidid, ketamine, predionum, thiopental sodium, hexenalum, sodium oxybutiras. Situational tasks in pharmacodynamics and pharmacokinetics 1. During the introduction of a patient to general anesthesia with ether, the bradycardia up to cardiac arrest was observed. What is the cause of cardiac arrest in the first stage of ether action? What drugs are used for prevention of this complication? 24 2. During surgical operation, the symptoms of asphyxia were developed in patient. Explain the cause of this complication and propose drugs for its prevention. 3. A patient with traumatic brain edema and hypoxic convulsions was admitted to a hospital. What general anesthetic may be used for relief of convulsions? Explain your answer. 4. Bradycardia and reduction of blood pressure was developed in patient during halothane anesthesia. Anesthesiologist administered to him noradrenaline. Did the doctor make the right choice? Suggest pressor drugs for restoration of blood pressure and explain your choice. 5. A patient with amputation of leg needs dressing. What general anesthetics may be used for analgesia in this case? Explain your answer. Fill in the following tables Table 18 – Comparison characteristics of inhalational anesthetics Characteristics Diethyl ether Halothane Nitrous oxide Degree of anesthetic action Speed of introduction in anesthesia Severity of anesthesia stages Severity of excitement stage Irritating action Relaxation of skeletal muscles Influence on cardiovascular system Hepatotoxicity and nephrotoxicity Indications for use 25 Table 19 – Comparison characteristics of intravenous anesthetics Characteristics Propanidid Ketamine Thiopental sodium Speed of anesthesia development Duration of anesthesia Influence upon respiration Influence on cardiovascular system Tolerance of brain to hypoxia Indications for use Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 26 Propanidid in ampoules. Thiopental sodium in bottles. Hexenalum in bottles. Sodium oxybutiras in ampoules. Ketamine in ampoules. Sodium oxybutiras Table 20 – Drugs for prescription Drug name Propanididum Single dose and mode of administration Intravenously 0.005–0.01 g/kg Thiopentalumnatrium Intravenously 0.4–0.5 g Hexenalum Intravenously 0.5–0.7 g Natrii oxybutyras Intravenously 0.07–0.12 g/kg Orally 0.1–0.2 g/kg (for general anesthesia); 2-3 table spoons before sleep (for treatment of insomnia) Ketaminum Intramuscularly 0.006 g/kg; intravenously 0.002 g/kg Drug product Ampoules 10 ml of 5% solution Bottles 0.5 g or 1.0 g of dry substance (should be dissolved before administration in 50 ml of sterile 0.9% solution of sodium chloride) Bottles 1.0 g of dry substance (should be dissolved before administration in 50 ml of sterile 0.9% solution of sodium chloride) Ampoules 10 ml of 20% solution Bottles 400 ml of 5% syrup Bottles 10 ml of 5% solution; or 20 ml of 1% solution 27 Hypnotic Drugs. Ethyl Alcohol Topical questions 1. The physiology of sleep: characteristics of recovering and sleeping system; REM and nonREM sleep. 2. Types of sleep disorders. 3. Classification of hypnotic drugs. 4. Characteristic of hypnotic drugs from group of benzodiazepine: mechanism of action, influence on the CNS, peculiarities of drugs pharmacokinetics, indications for use, adverse effects, and possible complications. 5. Zolpidem and zopiclone: mechanism of action and advantages of their use for treatment of insomnia. 6. Characteristic of hypnotic drugs – derivatives of barbituric acid: mechanism of action, influence on the CNS, peculiarities of drugs pharmacokinetics, indications for use, adverse effects, and possible complications. The signs of acute barbiturates poisoning and treatment of this condition. 7. Pharmacological and toxicological characteristic of ethyl alcohol. The use of ethyl alcohol in medical practice. The signs of acute and chronic ethyl alcohol poisoning (alcoholism). The treatment of this condition. Mechanism of action of teturamum (desulfiram). Situational tasks in pharmacodynamics and pharmacokinetics 1. A patient with insomnia suddenly stops the use of phenobarbital after regular drug intake during 1.5 months. The following symptoms develop after drug withdrawal: anxiety, irritability, fear, vomiting, visual disturbances, convulsions, orthostatic hypotension, and cardioinhibitory reflex. Explain the cause of symptoms observed in patient. Suggest the drugs for treatment of this pathological state. 2. Patient took phenobarbital on the background of evident alcohol intoxication. Death occurred at night during sleep. Explain why combination of ethyl alcohol and phenobarbital resulted in death. 28 Fill in the following table Table 21 – Comparison characteristics of hypnotic drugs Characteristics Phenobarbital Nitrasepam Sodium oxybutiras Speed of sleep development Duration of sleep Mechanism of action Influence on sleep structure Indications for use Side effects and complications Tasks for prescription Prescribe the following drugs: 1. Nitrazepamum in tablets. 2. Phenobarbital in tablets. 3. Aethaminalum-natrium in tablets. 4. Zolpidem in tablets. 5. Natrii oxybutiras in syrup for internal use. 6. Teturamum in tablets. Table 22 – Drugs for prescription Drug name Nitrazepamum Phenobarbital Aethaminalumnatrium Zolpidem Natrii oxybutiras Teturamum Single doses and mode of Drug product administration Orally 0.005–0.01 g before Tablets 0.005 or 0.01 g sleep) Orally 0.1 g before sleep Tablets 0.05 or 0.1 g Orally 0.1–0.2 g before sleep Tablets 0.1 g Orally 0.01 g before slee Orally 2–3 table spoons before sleep Orally 0.5 g once a day Tablets 0.01 g Bottles 400 ml of 5% syrup Tablets 0.25 g 29 Antiepileptic and Antiparkinsonian Drugs Topical questions 1. Classification of antiepileptic drugs according to their mechanisms of action and their clinical use for treatment of different types of epilepsy. 2. Drugs which block the sodium channel: mechanism of action; characteristics of some drugs (clinical use in epilepsy and adverse effects). 3. Drugs which activate GABA-system in brain (the derivatives of benzodiazepine, phenobarbital): mechanism of action, clinical use for treatment of different types of epilepsy, adverse effects. 4. Agents that block calcium channels (mechanism of action, clinical use and adverse effects of ethosuximide). 5. Drugs which are used for discontinuance of epileptic status. 6. The causes of Parkinson’s disease (pathological changes in mediators balance). 7. Classification of antiparkinsonian drugs according to their mechanism of action. 8. Levodopa: mechanism of action, clinical use and adverse effects. Expediency of combination the levodopa with inhibitors peripheral DOPA decarboxylase (carbidopa and benseraside). 9. Agonists of dopamine receptors. 10. Drugs that inhibit MAO-B. 11. Drugs from group of central cholinergic antagonists. 12. Midantanum. Situational tasks in pharmacodynamics and pharmacokinetics 1. Tonoclonic spasms periodically develop in patient after cranial trauma. What drugs should be prescribed to him for prevention of spasms? 2. Generalized convulsions developed in patient owing to unknown substance intoxication. Prescribe the drugs for its cessation. Explain the choice of mode of drugs administration and mechanism of drugs action. 3. Periodical short loss of consciousness is observed in patient after encephalitis. Simultaneously, contractions of muscles of the right half of face and neck are observed. Prescribe the drugs for its cessation. Explain the choice of mode of drugs administration and mechanism of drugs action. 4. The increased striated muscles tone, rigidity, and tremor are developed in patient due to long-term treatment with haloperidol. Explain 30 the mechanism of development of these complications and suggest drugs for their reduction. Fill in the following tables Table 23 – Comparison characteristics of antiepileptic drugs Drug Group name Antiepileptic activity Mechanism of action Side effects Phenobarbital Dipheninum Carbamazepine Ethosuximide Lamotrigine Sodium valproate Clonazepam Table 24 – Comparison characteristics of antiparkinsonian drugs Cyclodolum Mechanism action Side effects Midantanum Levodopa of Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 5. 6. 7. 8. Dipheninum in tablets. Carbamazepinum in tablets. Phenobarbital in tablets and powders for internal use. Ethosuximidum in capsules. Levodopa in tablets and capsules. Midantanum in coated tablets. “Nacom”. Cyclodolum in tablets. 31 Table 25 – Drugs for prescription Drug name Single dose and mode of administration Dipheninum Orally 0.117 g 3 times a day Carbamazepinum Orally 0.2–0.4 g 2 or 3 times a day Phenobarbitalum Orally 0.05 g 2 times a day Ethosuximidum Orally 0.25 g 3 times a day Clonazepamum Orally 0.001–0.002 g 3–4 times a day Levodopa Orally 0.25–1.0 g 3 times a day Midantanum Orally 0.1–0.2 g 2–4 times a day “Nacom” 1 tablets 1–4 times a day Cyclodolum Orally 0.001–0.005 g 2-3 times a day Drug product Tablets 0.117 g Tablets 0.1, 0.2 or 0.4 g Tablets 0.05 or 0.1 g Capsules 0.25 g Tablets 0.001 g Tablets 0.25 or 0.5 g; capsules 0.25 or 0.5 g Coated tablets 0.1 g Tablets Tablets 0.001, 0.002 or 0.005 g Opioid Analgesics Topical questions 1. The physiological mechanism of pain perception: nociceptive and antinociceptive systems. The concept about opioid receptors and their endogenous ligands. 2. The classification of drugs that influence opioid receptors (agonists, partial agonists, and antagonists). 3. The mechanism of analgesic action of opioid analgesics. 4. The characteristics of other effects of opioid analgesics (byway of example of morphine): influence on the CNS and peripheral organs and systems. 5. The comparion characteristics of other drugs from group of opioid analgesics. Peculiarities of promedolum, omnopon, fentanyl, pentazocine. 6. The indications for use of opioid analgesics. 32 7. The adverse effects of opioid analgesics. Contraindications to their use. 8. The signs of acute opioid analgesics poisoning. The treatment of this poisoning. Use of antagonists of opioid receptors. 9. Phenomena that can develop as a result of long-time use of opioid analgesics. The causes of opioid analgesics dependence. The treatment of dependence. Situational tasks in pharmacodynamics and pharmacokinetics 1. A woman with pathological pregnancy needs analgesia of delivery. What opioid analgesic may be used? Why? 2. A patient with acute morphine poisoning is admitted to a hospital. Suggest treatment for this patient. Explain your choice of drugs. 3. A patient with acute pain owing to biliary colics is admitted to a hospital. What opioid analgesic may be used for pain relief in this patient? Explain your answer. 4. A doctor prescribed Talamonal to patient with acute myocardial infarction. What is Talamonal? Were his actions correct? Fill in the following tables Table 26 – Influence of morphine upon the systems and organs System, organ Central nervous system Nociceptive system Cough center Respiratory center Vomiting center Vasomotor center Oculomotor center Vagal center Center of thermoregulation Peripheral tissues and organs Cardiac rhythm Blood pressure Tone of urinary and biliary tracts Intestinal tone Diuresis Morphine 33 Analgesic activity Duration of action Drug dependence Inhibition of respiratory center Spasm of smooth muscles Indications for use Notation: “+++”– pronounced effect; “++” – moderate effect; “+” – weak effect; “-“ – depressing effect. Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 5. 6. 7. 34 Morphine in ampoules. Omnopon in ampoules. Promedolum in ampoules and tablets. Phentanyl in ampoules. Pentazocine in tablets. Pentazocine in ampoules and rectal suppositories. Naloxone hydrochloridum in ampoules. Codeine Pentazocine Fentanyl Promedolum Omnopon Morphine Table 27 – Comparison characteristics of opioid analgesics Table 28 – Drugs for prescription Drug name Morphini hydrochloridum Omnoponum Promedolum Phentanylum Pentazocini lactas Pentazocini hydrochloridum Naloxoni hydrochloridum Single doses and mode of administration Orally 0.01 g; subcutaneously 0.01 g Drug product Powders; ampoules 1 ml of 1% solution Orally 0.01–0.02 g; Powders; subcutaneously 0.01–0.02 g ampoules 1 ml of 1% or 2% solution Orally 0.025 g Tablets 0.025 g subcutaneously 0.01–0.02 g ampoules 1 ml of 1% or 2% solution Intramuscularly or ampoules 2 ml or 5 ml intravenously 0.00005– of 0.005% solution 0.0001 g Subcutaneously or Ampoules 1 ml of 3% intramuscularly 0.03 g solution; through rectum 0.05 g suppositories 0.05g Orally 0.05 g Tablets 0.05 g Subcutaneously, intramuscularly or intravenously 0.0004– 0.0008 g Ampoules 1 ml or 2 ml of 0.04% solution Nonopioid Analgesics Topical questions 1. The classification of nonopioid analgesics. 2. The mechanism of action of nonopioid analgesics. The concepts of COX-1 and COX-2. 3. The main effects of nonopioid analgesics: analgesic, antiinflammatory, and antipyretic. 35 4. The characteristics of the salicylic acid derivatives: therapeutic effects, influence on internal organs and systems, indications for use, adverse effects, and signs of overdose. 5. The characteristics of pyrazolone derivatives drugs effects, indications for use, and adverse effects. 6. The characteristics of p-aminophenol derivatives. Advantage and disadvantage of paracetamolum. 7. The comparison characteristics of derivatives of anthranilic, indoleacetic, phenylacetic, phenilpropionic, and naphtylpropionic acid. The peculiarities of ketorolac. 8. The COX-2 inhibitors. Situational tasks in pharmacodynamics and pharmacokinetics 1. A patient suffers from pain owing to inflammation of knee-joint. What drugs may be prescribed to him? Why? 2. A student complains of a headache during classes. What drugs can you suggest him? Why? Fill in the following tables Traumatic pain Neuralgia, myositis Spastic pain Headache Myocardial infarction Analgesia of delivery Rheumatoid arthritis 36 Butadione Analgin Aspirin Pentazocine Fentanyl Promedol Indication for use Morphine Table 29 – Clinical use of analgesics Table 30 – Comparison characteristics of non-opioid analgesics Drug Chemical structure Indications for use Side effects Acetylsalicylic acid Analgin Butadione Indometacin Ortophen Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 5. Acetylsalicylic acid in tablets. Analgin in tablets and ampoules. Butadione in tablets and ointment. Diclofenac-sodium in tablets and ampoules. Paracetamol in tablets. Table 31 – Drugs for prescription Drug name Single dose and mode of administration Acidum Orally 0.25–1.0 g 3-4 acetylsalicylicum times a day Tablets 0.1, 0.25 or 0.5 g Analginum Tablets 0.5 g; Butadionum Diclofenacnatrium Orally 0.25–0.5 g 2-3 times a day; intramuscularly or intravenously 0.25–0.5 g 2–3 times a day Orally 0.1–0.15 g 2–4 times a day; for external application as 5% ointment Orally 0.025–0.05 g 1-3 times a day; intramuscularly 0.075 g once a day Drug product ampoules 1 or 2 ml of 25% or 50% solution Tablets 0.15 g 5% ointment Coated tablets 0.025 g Ampoules 3 ml of 2.5% solution 37 Table 31 continuation Paracetamolum Orally 0.2–0.4 g 2–3 times a day Tablets 0.2 g Neuroleptic and Antidepressant Drugs Topical questions 1. The classification of neuroleptics. 2. The mechanism of action of neuroleptics (influence on different types of CNS receptors). 3. The main effects of neuroleptics: antipsychotic and sedative; their clinical displays. 4. The characteristic of other effects of neuroleptics: hypnotic, myorelaxation, hypothermic, antiemetic, hypotensive, and antispasmodic. 5. The peculiarities of different antipsychotic drugs – phenothiazine derivatives: aminazinum, triftazinum, phthorphenasinum. The typical adverse effects of phenothiazine derivatives. 6. The characteristics of derivatives of butyrophenone, thioxanthene. 7. The characteristics of “atypical” neuroleptics: sulpiride and clozapine. Advantage of “atypical” neuroleptics. 8. The indications for use of neuroleptics. 9. Antidepressant drugs. Drugs which inhibit the neuronal reuptake of monoamines: classification, mechanisms of action of different subgroups, clinical use, adverse effects. 10. MAO inhibitors: classification, mechanism of action, clinical use, and adverse effects. Situational tasks in pharmacodynamics and pharmacokinetics 1. A patient suffers from psychosis with psychomotor excitement. Which neuroleptics should be prescribed to him? Why? 2. A pregnant woman suffers from gestosis with frequent vomiting. Which neuroleptics may be used for interruption of vomiting? Explain mechanism of drug action. 3. Together with other drugs, aminazine was prescribed to patient with ulcer disease of stomach. Which pharmacological effects of aminazine are useful in this case? 38 Fill in the following tables Table 32 – Comparison characteristics of neuroleptics Effect aminazine Degree of effect chlorprothixene haloperidol Antipsychotic Decrease of motor activity Sedative Hypnotic Analgesics and general anesthetics potentiation Antiemetic Hypotensive Extrapyramidal disorder Tasks for prescription Prescribe the following drugs and list indications for their use: 1. 2. 3. 4. 5. 6. 7. 8. Aminazinum in dragee and ampoules. Triftazinum in tablets and ampoules. Haloperidolum in tablets and ampoules. Droperidolum in ampoules. Imizinum in tablets and ampoules. Amitriptylinum in tablets and ampoules. Fluoxetine in tablets. Lithii carbonas in tablets. 39 Table 33 – Drugs for prescription Drug name Single dose and mode of Drug product administration Aminazinum Orally 0.025–0.05 g 1–3 Dragee 0.025, 0.05 or times a day; 0.1 g; intramuscularly 0.1 g 1–3 ampoules 1, 2, 5 or 10 ml times a day; of 2.5% solution intravenously 1–2 ml of 2.5% solution with 20 ml of 40% glucose solution (in case of acute psychomotor agitation) Triftazinum Orally 0.005–0.01 g once a Tablets 0.001, 0.005 or day; 0.01 g; intramuscularly 0.001–0.002 g 1 ampoules 1 ml of 0.2% once a day solution Haloperidolum Orally 0.0015–0.005 g 3 times Tablets 0.0015 or 0.005 a day; g; intramuscularly 0.002–0.005 g ampoules 1 ml of 0.5% solution Droperidolum Intramuscularly or Ampoules 5 or 10 ml of intravenously 0.0025–0.005 g 0.25% solution Imizinum Orally 0.025-0.05 g 1–3 times Tablets 0.025 g; a day; intramuscularly 0.025 g 1–3 ampoules 2 ml of 1.25% times a day solution Amitriptylinum Orally 0.025–0.05 g 3–4 times Tablets 0.025 g; a day intramuscularly or ampoules 2 ml of 1% intravenously 0.025–0.04 g 3– solution 4 times a day Fluoxetinum Orally 0.02 g 1–2 times daily Capsules 0.01 and 0.02 g 40 Tranquilizers. Lithium Salts. Sedative Drugs Topical questions 1. The classification of tranquilizers. 2. The mechanism of action of tranquilizers – derivatives of benzodiazepine. 3. The main effects of benzodiazepine derivatives: tranquilizing, sedative, hypnotic, myorelaxation, and anticonvulsive. 4. The indications for use of benzodiazepine derivatives. 5. The side effects of benzodiazepine derivative. The sings of overdosage and treatment of this condition. 6. The characteristics of “daily” anxiolytics: buspirone, propranolol, nootropil. Clinical use of these drugs. 7. Lithium salts: representatives, mechanism of action, pharmacological effects, clinical use, and adverse effects. 8. The characteristics of sedative drugs: mechanism of action, effects, clinical use. The cause, sings, and treatment of bromism. Situational tasks in pharmacodynamics and pharmacokinetics 1. A patient complains of anxiety, fear, and internal tension. What drugs should be prescribed to him? Explain the mechanism of drugs action. 2. An airport manager, came to consult a doctor with complaints of anxiety, internal tension, and fear. Doctor prescribed diazepam 3 times a day. Did doctor prescribe drug correctly? Give necessary explanations. Fill in the following tables Table 34 – Comparison characteristics of tranquilizers Effect Degree of effect chlozepidum diazepam buspirone Anxiolytic Sedative Hypnotic Analgesics potentiation Muscular relaxation Anticonvulsive Amnestic amizylum 41 Table 35 – Comparison characteristics of psychotropic drugs, which inhibit central nervous system Effect Antipsychotic Sedative Inhibition of vegetative reflexes Analgesics and general anesthetics potentiation Relaxation of skeletal muscles Anticonvulsive Antiemetic Hypotonic Iatrogenic parkinsonism Neuroleptics Tranquilizers Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 5. 6. 7. 42 Diazepam in tablets and ampoules. Phenazepam in tablets. Nitrazepam in tablets. Lithium carbonate in tablets. Sodium bromide in tablets. Tincture Valeriana. Tincture Leonurus. Sedative drugs Table 36 – Drugs for prescription Drug name Diazepamum Phenazepamum Nitrazepamum Gidazepamum Lithii carbonas Natrii bromidum Tinctura Valerianae Tinctura Leonuri Single doses and mode of administration Orally 0.005–0.015 g 3 times a day; intramuscularly or intravenously 0.01–0.02 g 1-3 times a day Orally 0.00025–0.001 g 1–2 times a day Orally 0.005–0.01 g 1–2 times a day Orally 0.02–0.05 g 3 times daily Orally 0.3–0.6 g Orally 0.5–1.0 g 3–4 times a day Orally 20–30 drops 3–4 times a day Orally 30–50 drops Drug product Tablets 0.005 g; ampoules 2 ml of 0.5% solution Tablets; 0.0005 or 0.001 g Tablets 0.005 or 0.01 g Tablets 0.02 or 0.05 g Tablets 0.3 g Tablets 0.5 g Tincture 30 ml Tincture 25 ml Psychostimulants. Nootropic Drugs. Analeptics. Adaptogens Topical questions 1. The classification of psychostimulants. 2. The mechanism of action of psychostimulants – derivatives of phenylalkylamine, piperidine, and sidnonimine. Their pharmacological effects. 3. The mechanism of action of caffeine. Influence of caffeine upon different organs and systems. 4. The indications for use of psychostimulants. Side effects and contraindications for their use. 5. Nootropic drugs: mechanism of action, effects, indications for use. 6. The classification of analeptics. Mechanisms of action and pharmacological effects. Clinical use of analeptics. 7. Adaptogens: mechanism of action, effects, and indication for their use. 43 Tasks for prescription Prescribe the following drugs: 1. 2. 3. 4. 5. 6. 7. 8. Sydnocarbum in tablets. Coffeinum-natrii benzoas in tablets and in ampoules. Pyracetamum in tablets, capsules, and ampoules. Bemegridum in ampoules. Cordiaminum in ampoules. Camphora in ampoules. Aethimizolum in ampoules. Sulfocamphocainum in ampoules. Table 37 – Comparison characteristics of psychostimulants Degree of effect Psychostimulative Decrease of need for sleep Rise of blood pressure Increase of heart work Indications Side effects Phenaminum Sydnocarbum Caffeine Table 38 – The main effects of analeptics Effect Stimulation respiratory center Stimulation vasomotor center Awakening effect Convulsive action 44 Caffeine of of Bemegride Lobeline Table 39 – Drugs for prescription Drug name Sydnocarbum Coffeinumnatrii benzoas Pyracetamum Bemegridum Cordiaminum Camphora Single dose and mode of administration Orally 0.005–0.025 g 1–2 times a day (in the first part of day) Orally 0.1–0.2 g 1-2 times a day; subcutaneously 0.1–0.2 g 1–2 times a day Orally, intramuscularly or intravenously 0.4–1.2 g 3 times a day Intravenously slowly 0.01–0.05 g Subcutaneously, intramuscularly or intravenously 1 ml Subcutaneously 0.2–1 g Aethimizolum Intravenously or intramuscularly 0.03– 0.06 g 1–2 times daily Sulfocampho- Subcutaneously, cainum intramuscularly or intravenously 0.2 g 2–3 times daily Drug product Tablets 0.005, 0.01 or 0.025 g Tablets 0.1 or 0.2 g; ampoules 1 or 2 ml of 10% or 20% solution Tablets 0.2 g; capsules 0.4 g; ampoules 5 ml of 20% solution Ampoules 10 ml of 0.5% solution Ampoules 1 ml Ampoules 1 or 2 ml of 20% oil solution Ampoules 3 or 5 ml of 1% or 1.5% solution Ampoules 2 ml of 10% solution 45 REFERENCES 1. Chekman I.S. Pharmacology: Textbook / I.S. Chekman, N.O. Gorchakova, N.I. Panasenko, P.O. Bekh. – Vinnytsya : NOVA KNYHA Publishers, 2006. – 384 p. 2. Kresyun V.A. General pharmacology: Cource of Lectures / V.A. Kresyun, D.Yu. Andronov, K.F. Shemonaeva. – Odessa : OSMU, 2005. – 215 p. 3. Polevik I.V. Lectures on Pharmacology: For the Foreign Students Being Educated in English / I.V. Polevik, A.I. Beketov, M.G. Kurchenko. – Simferopol, 2003. – Part 1. – 100 p. 4. Polevik I.V. Lectures on Pharmacology: For the Foreign Students Being Educated in English / I.V. Polevik, A.I. Beketov, M.G. Kurchenko. – Simferopol, 2003. – Part 2. – 108 p. 5. Stefanov O. Pharmacology with General Prescription: Textbook for English-speaking medical students / O. Stefanov, V. Kurcher. – К. : Вид-во «Ельіньо». – 2004. – 156 p. 6. Pharmacology with General Prescription: Text-book for Englishspiking medical students. / O. Stefanov, V. Kurcher. – К. : Вид-во «Ельіньо». – 2007. - 318 p. 7. Газій T.В. Study guide to basic pharmacology. Навчальний посібник з фармакології / T.В. Газій. – Харків : “Факт”, 2005. – 126 c. 8. Harvey R.A. Pharmacology / Richard A. Harvey, Pamela C. Chempe – 2nd edition. – Lippincott Williams & Wilkins, 1997. – 564 p. 9. Goodman. The pharmacological basis of therapeutics. / Goodman, Gilman’s. – 9th edition. – McGraw-Hill, 1996. – 1811 p. 10. Bertram G.K. Basic and Clinical Pharmacology: Textbook / Bertram G. Katzung. – 10th edition. – McGraw-Hill Companies, 2007. – 1200 p. 11. Vysotsky I.Yu. Medical Prescription (for foreign students being educated in English) / I.Yu. Vysotsky, R.A. Chramova, A.A. Kachanova. – Sumy : Sumy State University Publishers, 2008. – 40 p. 12. Vysotsky I.Yu. Drugs affecting peripheral nervous system: for foreign students being educated in English / I.Yu. Vysotsky, R.A. Chramova, A.A. Kachanova. – Sumy : Sumy State University Publishers, 2009. – 62 p. 46 CONTENTS P. Drugs Affecting the Afferent Innervation……………………………....... …..3 Cholinomimetics. Cholinesterase inhibitors……………………………... …..5 M-cholinergic antagonists………………………………………………... ….10 N-cholinergic antagonists: Ganglion Blocking Drugs and Skeletal Muscles Relaxants……………………………………………………...... ….13 Adrenomimetics and Sympathomimetics………………………………... ….16 Adrenergic Antagonists……………………………………………….......….20 General Anesthetics…………………………...………………………..... .…22 Hypnotic Drugs. Ethyl Alcohol ……………………………………….... .....26 Antiepileptic Drugs. Antiparkinsonian Drugs ………………………….. ….28 Opioid Analgesics……………………………………………………....... ….30 Nonopioid Analgesics…………………………………………………..... ….33 Neuroleptics and Antidepressants ……………………………………...... ….36 Anxiolytic Drugs. Lithium Salts. Sedative Drugs …………………….....….39 Psychostimulants. Nootropic Drugs. Analeptics. Adaptogens ………...... ….41 REFERENCES……………...…………………………………………….….44 47