Antithrombotic Scena.. - Evidence Based Clinical Pratice
CLINICAL PRACTICE GUIDELINE UNIT
GUIDELINE for the MANAGEMENT of PULMONARY EMBOLISM:
THROMBOLYSIS or NO THROMBOLYSIS
Objective
At the end of this unit the learner should be able to assess the validity of a practice guideline and it’s applicability in patient care.
Part 1
Clinical Scenario:
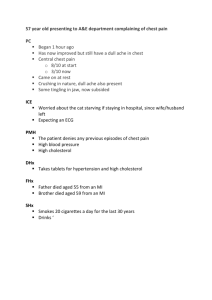
During the course of a 2 month rotation as an SMR you see the following two patients.
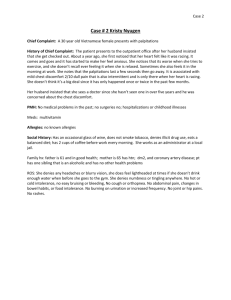
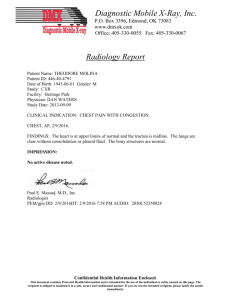
Patient 1: A 65 year old man has been experiencing fatigue and malaise for three months, with no other specific symptoms. He presents with sudden onset of severe shortness of breath and pleuritic chest pain. On examination his skin in cold and sweaty, he is tachycardic (HR 115), tachypneic (RR 28), and hypotensive (BP 90/60) while lying flat, with a oxygen saturation of 85% on room air. Chest radiograph shows possible hypoperfusion in both lower lung fields and an electrocardiogram shows signs of right ventricular strain. Troponin is 0.2. A CT pulmonary angiogram shows large bilateral pulmonary emboli. The patient reports no history of bleeding or symptoms suggesting peptic ulcer disease. You consult the thrombosis service who recommends the administration of tPA. Two hours following tPA administration the patient develops a severe headache and over the period of a few minutes loses consciousness. A CT of the head show a large intracranial haemorrhage.
Patient 2: A 32 year old previously health woman presents with onset of shortness of breath without chest pain over the period of a few hours. She has used oral contraceptive for the last three years. On examination, she appears unwell. Her heart rate is 90, her respiratory rate 24, her blood pressure 125/75, with a oxygen saturation of 92% on room air. Physical findings are otherwise normal, with no jugular venous distension. Her PO2 on room air is 75. You begin intravenous heparin and obtain an urgent echocardiogram which is interpreted as showing mild right ventricular dysfunction. You consult the thrombosis service. The attending (who was also the attending for the previous patient two weeks before) recommends against thrombolytic therapy.
Wondering about whether one or both of these patients received optimal therapy, you decide to consult one of your favourite practice guidelines, produced by the American College of Chest Physicians antithrombotic group, which latest recommendations appeared in January 2012.
Having been trained at McMaster to be unreasonably skeptical, you wonder about the process of developing the recommendations: are these really
trustworthy guidelines. You decide to look into both issues using the
“methods” articles associated with the guidelines.
Readings
1) Top priority: Guyatt GH, Norris SL, Schulman S, Hirsh J, Eckman MH, Akl
EA, Crowther M, Vandvik PO, Eikelboom JW, McDonagh MS, Lewis SZ,
Gutterman DD, Cook DJ, Schunemann HJ. Methodology for the Development of Antithrombotic Therapy and Prevention of Thrombosis Guidelines:
Antithrombotic Therapy and Prevention of Thrombosis, 9 th ed: American
College of Chest Physicians Evidence-Based Clinical Practice Guidelines.
Chest 2012 Feb;141(2 Suppl):53S-70S. Note, key sections highlighted. This is to encourage you to look at this befor the EBM day.
2) Guyatt G, Prasad K, Schunemann H, Jaeschke R, Cook DJ. How to use a patient management recommendation. In: Guyatt G, Rennie D, Meade M,
Cook D. Users' Guides to the Medical Literature: A Manual for Evidence-
Based Clinical Practice. McGraw-Hill, 2008.
Assignment
Decide, on the basis of the paper describing its methodology, the credibility of the guideline.