ECG quiz
advertisement

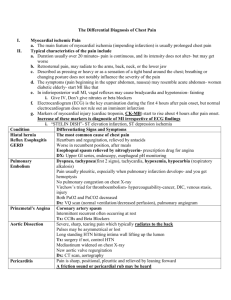
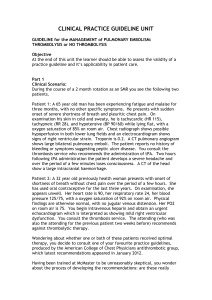
ECG, XR, Chest Pain, SOB Less Ca2+ influx superslow Ca2+ influx prolongs plateau phase prolongs ST segment prolong QT segment Clues: Metabolic situation, look at QT segments Shortened AP less plateau phase shortened segments Hyperkalemia: more positive outside RMP is more + phase 0 in presence of high K+, the number of Ca2+ decrease less Ca2+ in to cell slowing of impulse conduction QRS widening Axis: + in lead 1, + in lead aVF = normal Infarction: ST elevation in lead 3 = inferior infarction Hypertrophy: LVH = tall R wave in leads V4 or V6 RVH = dominant R waves in V1 Rate: 300/3 = ~100 Rhythm: regular sinus MI Anterior infarction: changes classically in leads V3- V4 (but also V2 and V5) Inferior: changes in lead III and aVF Lateral infarction: changes in leads I, aVL, V5-6. AV node is continuously bombarded with depolarization waves Conduction into ventricles is normal therefore QRS is normal however irregular Rate: 300/ 3-2 = 100150 Rhythm: no P wave Irregular Atrial filbrillation Rate: no relationship between P waves and QRS complexes Rhythm: sinus with complete heart block and AV junctional type escape rhythm Escape junctional beat or rhythm occurs when there is failure of impulse generation from the sinus node or atrial myocardium. The 4th and 5th beats of this tracing are junctional beats that are not preceeded by a P wave and occur after a pause that is longer than the underlying sinus cycle length Axis: RAD Hypertrophy: RVH – lead V1 R wave is larger than S wave Lead V6, S wave is larger than R wave Rate: 93 Answer: Right ventricular hypertrophy Rhythm: sinus The most likely diagnosis is A. congestive heart failure. B. pericardial effusion. C. intracardiac shunt. D. expiratory phase of respiration. E. pulmonic stenosis. This case represents an apparent "enlarged heart" due to an expiratory phase of respiration in an uncooperative patient. Note the decreased lung volumes and the elevation of the hemidiaphragms. The resultant crowding of vessels obscures much of the cardiac border. The technique of inspiratory PA radiograph is preferred to avoid "diagnosing" diseases that a patient does 60-year-old alcoholic man with shortness of breath. The most likely diagnosis is A. mediastinal mass. B. intracardiac shunts (ASD and VSD) C. pericardial effusion or cardiomyopathy D. combined aortic and pulmonary arterial disease. E.technical aberrations. 53-year-old woman examined in the emergency department for chest pain, tachycardia, and shortness of breath with normal ECG. The most likely cause of the patient's symptoms is A. pneumonia. B. pulmonary edema. C. interstitial lung disease. D. panic attack. E. pneumothorax. Panic attack In this case the chest radiograph was normal in a 53- year-old woman seen in the emergency department for left-sided chest pain. The electrocardiogram was also normal, and there was no obvious cause for the patient's pain. Note the well-defined pulmonary vessels in the perihilar region and normal branching of these vessels into the lungs. There is a gradient of pulmonary vascular markings from the bases to the apices on an upright radiograph due to the increased perfusion to the lower lobes. No pulmonary parenchymal abnormalities are present to support the other diagnoses. 50-year-old woman with acute shortness of breath. A. cardiac failure with pulmonary edema. B. pulmonic stenosis with pneumonia. C. pulmonary embolism. D. pneumomediastinum. E. pneumothorax. This case is an example of a pulmonary edema due to fluid overload and congestive heart failure. Note the increased size of the cardiac silhouette, the ill-defined reticular perihilar air-space opacities, the enlargement of the vascular pedicle, and the redistribution of blood flow to the upper lung zones. Chest pain Probability Dx of Chest Pain 3 of them Musculoskeletal (chest wall) Psychogenic Angina Serious not to be missed what are the systems/ categories? Cardiovascular myocardial infarction/unstable angina aortic dissection pulmonary embolism Neoplasia arcinoma lung tumours of spinal cord and meninges Infection pneumonia/pleurisy mediastinitis pericarditis Pneumothorax Pitfalls (often missed) Mitral valve prolapse Oesophageal spasm Gastro-oesophageal reflux Herpes zoster Fractured rib (e.g. cough fracture) Spinal dysfunction Probability dx of dyspnoea Bronchial asthma Bronchiolitis (children) Left heart failure COPD Obesity Lack of fitness From ‘how to treat’ paper (on wiki) 2. Bob, 50, is anxious and presents with chest pain. Which TWO aspects of the clinical history would be most helpful in deciding if the pain is cardiac in origin? a) His pain worsens while walking from the car park to your rooms and eases while sitting b) He describes sweating accompanying the pain c) He describes the pain as like a feeling of pressure d) His pain is relieved by nitrates given to him by your practice nurse Case study Peter, 47, A&E with left-sided chest pain Diagnosed with MSK condition Now returns to emergency few days later Same pain (central), pain in left side of neck and shoulder History of asthma, and now complains of slight SOB During ex – leaned back, winced in pain Changing position affected his pain, better when he sat up and leaned forward Lungs were clear and peak flow was normal DDX?? Intense, grating sound of a pericardial friction rub, confirming the diagnosis of pericarditis.