summary of product characteristics
advertisement

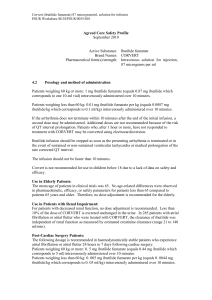
SUMMARY OF PRODUCT CHARACTERISTICS 1 NAME OF THE MEDICINAL PRODUCT CORVERT 87 microgram/ml, solution for infusion 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Ibutilide fumarate (INN) 0.1 mg/ml corresponding to ibutilide 87 microgram/ml. For a full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Solution for infusion. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Acute conversion of atrial fibrillation or atrial flutter to sinus rhythm. Please see section 5.1 for efficacy rates in clinical trials. 4.2 Posology and method of administration Patients weighing 60 kg or more: 1 mg ibutilide fumarate (equals 0.87 mg ibutilide which corresponds to one 10-ml vial) intravenously administered over 10 minutes. Patients weighing less than 60 kg: 0.01 mg ibutilide fumarate per kg (equals 0.0087 mg ibutilide/kg which corresponds to 0.1 ml/kg) intravenously administered over 10 minutes. If the arrhythmia does not terminate within 10 minutes after the end of the initial infusion, a second dose may be administered. Additional doses are not recommended because of the risk of QT interval prolongation. Patients who, after 1 hour or more, have not responded to treatment with CORVERT may be converted using electrocardioversion. Ibutilide infusion should be stopped as soon as the presenting arrhythmia is terminated or in the event of sustained or non-sustained ventricular tachycardia or marked prolongation of the rate corrected QT interval. The infusion should not be faster than 10 minutes. Corvert is not recommended for use in children below 18 due to a lack of data on safety and efficacy. Use in Elderly Patients: The mean age of patients in clinical trials was 65. No age-related differences were observed in pharmacokinetic, efficacy, or safety parameters for patients less than 65 compared to patients 65 years and older. Therefore, no dose adjustment is recommended for the elderly. Use in Patients with Renal Impairment: For patients with decreased renal function, no dose adjustment is recommended. Less than 10% of the dose of CORVERT is excreted unchanged in the urine. In 285 patients with atrial fibrillation or atrial flutter who were treated with CORVERT, the clearance of ibutilide was independent of renal function as measured by estimated creatinine clearance (range 21 to 140 ml/min). Post-Cardiac Surgery Patients: The following dosage is recommended in haemodynamically stable patients who experience atrial fibrillation or atrial flutter 24 hours to 7 days following cardiac surgery. Patients weighing 60 kg or more: 0. 5 mg ibutilide fumarate (equals 0.44 mg ibutilide which corresponds to 5 ml) intravenously administered over 10 minutes. Patients weighing less than 60 kg: 0. 005 mg ibutilide fumarate per kg (equals 0. 0044 mg ibutilide/kg which corresponds to 0. 05 ml/kg) intravenously administered over 10 minutes. If the arrhythmia does not terminate within 10 minutes after completed infusion, a second dose may be administered. Treatment Control: If ventricular arrhythmia arises or is worsened during administration of CORVERT, the infusion should be stopped immediately (see section 4.4 - Special warnings and special precautions for use). 4.3 4.4 Contraindications Hypersensitivity to the active substance or to any of the excipients CORVERT, solution for infusion should not be given to patients who have previously demonstrated: o Polymorphic ventricular tachycardia (e.g. torsades de pointe) o Symptomatic heart failure o Prolonged QT interval (> 440 msec) o Second and third degree AV-block in patients without pacemakers o Sick sinus syndrome o Recent myocardial infarction (< 1 month) o Hypokalemia o Hypomagnesemia Concomitant treatment with class I or class III antiarrhythmic agents Severe hepatic impairment Special warnings and precautions for use CORVERT may induce life-threatening ventricular arrhythmias (torsades de pointe). Polymorphic tachycardia was seen in about 5% of the patients treated for atrial fibrillation/flutter in clinical studies. Life-threatening sustained polymorphic ventricular tachycardia was seen in 1.9% of the treated patients. The polymorphic ventricular tachycardia may degenerate into vetricular fibrillation. Patients with a history of congestive heart failure (CHF) or low left ventricular ejection fraction have a higher risk of developing serious proarrhythmia including sustained polymorphic ventricular tachycardia (see section 4.3 Contraindications). In the clinical studies, a higher incidence of monomorphic ventricular tachycardias was seen in women. Prior to the start of the treatment, the need for anticoagulant treatment should be decided upon and possible hypokalemia and hypomagnesemia should be corrected. Digoxin intoxication should be ruled out prior to treatment (see section 4.5 Interactions with other medicinal products and other forms of interactions). The cardiac rhythm should be continuously monitored during the entire infusion period and thereafter for a minimum of 4 hours after the infusion has been stopped. In those cases where the QTc interval has not returned to baseline, the cardiac rhythm should be supervised for more than 4 hours. Longer monitoring may be required if proarrhythmic activity is noted during CORVERT infusion or during the 4 hour monitoring period. If serious proarrhythmia occurs, this should be evaluated and care should be taken with the future use of medications which have potential to prolong the QT interval or cause proarrhythmia. The treatment should be monitored by personnel having knowledge of arrhythmia diagnostics and equipment for acute defibrillation must be readily available. Patients who previously have had ventricular arrhythmias should be monitored for at least 24 hours. Class I or class III antiarrhythmics should not be given earlier than 4 hours after the end of the ibutilide infusion and only if the QTc interval has returned to baseline. The cardiac rhythm in these patients should be monitored for at least 24 hours. 4.5 Interaction with other medicinal products and other forms of interaction Although formal interaction studies have not been performed, class I antiarrhythmic drugs (disopyramide, quinidine, procainamide) and other class III drugs (amiodarone, sotalol and dofetilide) should not be given concomitantly with CORVERT, within 4 hours, and only if the QTc interval has returned to baseline because of their potential to prolong refractoriness (see section 4.3 Contraindications). The potential for proarrhythmia may increase with the administration of CORVERT to patients who are being treated with drugs that prolong the QT interval, such as antipsychotic drugs (phenothiazines: thioridazine, chlorpromazine and levomepromazine; benzamides: sulpride, sultopride, amisulpride and tiapride; pimozide: haloperidol; droperidol), tricyclic or tetracyclic antidepressants, antibiotics (macrolides: erythromycin compounds; fluoroquinolones; pentamidine), some antihistamines (terfenadine and astemizole) and drugs of the other classes (bepridil; cisapride; diphemanil; halofanrin and mizolastine). The clinician should assess the risk/benefit ratio of concomitant use of ibutilide fumarate and the medications listed above and the risk of inducing torsades de pointes. Supraventricular arrhythmias may mask the cardiotoxicity associated with excessive digoxin levels. Therefore, it is advisable to be particularly cautious in patients whose plasma digoxin levels are above or suspected to be above the usual therapeutic range. Concomitant treatment with CORVERT and digoxin does not affect their individual plasma concentration. Concomitant treatment with beta-adrenergic blocking agents or with calcium channel blocking agents does not affect the pharmacokinetics of CORVERT. 4.6 Pregnancy and lactation Pregnancy There are no adequate data from the use of ibutilide in pregnant women. In one species, the rat, studies have shown embryotoxic and teratogenic effects. However animal studies are insufficient to conclude (see section 5.3). In view of the indication, CORVERT should be used during pregnancy when clearly necessary. Lactation The excretion of ibutilide in animal and human milk is unknown. Breast-feeding is therefore not recommended during treatment by ibutilide. 4.7 Effects on ability to drive and use machines Not relevant. 4.8 Undesirable effects Proarrhythmias are the most common and serious side-effects. In the clinical studies, 1.9% of the patients developed a life-threatening sustained polymorphic ventricular tachycardia (torsades de pointes) requiring acute cardioversion; Non-sustained polymorphic ventricular tachycardias were seen in 3.1%. All initial episodes of polymorphic ventricular tachycardia were seen within 40 minutes from the beginning of treatment. Patients with a history of congestive heart failure (CHF) or low left ventricular ejection fraction have a higher risk of developing serious proarrhythmia including sustained polymorphic ventricular tachycardia. The following undesirable effects have been observed and reported during treatment with ibutilide with the following frequencies: Very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); very rare (<1/10,000), not known (cannot be estimated form the available data). Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness System Organ Class Cardiac disorders Frequency common Undesirable effects Ventricular tachycardia (sustained polymorphic and monomorphic ventricular tachycardia, non-sustained polymorphic and monomorphic ventricular tachycardia) Ventricular extrasystoles Atrioventricular block Bundle branch block Bradycardia Vascular disorders Renal and Urinary disorders Investigations 4.9 Supraventricular tachycardia. Uncommon Ventricular fibrillation Angina pectoris Atrial fibrillation Common Hypotension Uncommon Hypertension Vasodilatation Uncommon Acute kidney failure common Electrocardiogram QT prolonged Overdose In the clinical trials, four patients were unintentionally overdosed. The largest dose was 3.4 mg ibutilide fumarate administered over 15 minutes. One patient developed increased ventricular ectopy and monomorphic ventricular tachycardia, another patient developed A-V block 3rd degree and nonsustained polymorphic ventricular tachycardia, and in the other two patients no adverse events were seen. In case of overdosage, the risk of occurrence of proarrhythmic events is therefore increased, especially in patients with a history of congestive heart failure and/or a decreased ejection fraction. The clinical effects of an overdosage with ibutilide could exaggerate the expected prolongation of repolarization seen at usually clinical doses. In case of overdosing, symptomatic and supporting therapy should be given. 5 PHARMACOLOGICAL PROPERTIES 5.1 Pharmacodynamic properties Pharmacotherapeutic group: Antiarrhythmics, class III, ATC code: C01B D05 Mechanism of action: CORVERT is an antiarrhythmic drug with predominantly class III (cardiac action potential prolongation) properties according to the Vaughan Williams classification. Ibutilide prolongs action potential duration in isolated adult cardiac myocytes and increases both atrial and ventricular refractoriness in vivo. Studies indicate that ibutilide, at nanomolar concentrations, delays repolarisation by activation of a slow, inward current (predominantly sodium), rather than by blocking outward potassium currents, which is the mechanism by which most other class III antiarrhythmics act. In humans, the predominant electrophysiologic property of CORVERT, solution for infusion is demonstrated by prolongation of effective refractory periods in atrial and ventricular muscle. Hemodynamics: When CORVERT was given intravenously to animals at doses greater than ten times the human dose, mild, negative, inotropic effects were observed (less than 8% decrease in left ventricular contractility). In a small hemodynamic study in patients (n=47), a statistically significant decrease in cardiac output (appr. 0.57 L/min) was seen in patients with an EF > 35%. This was not accompanied by any changes in pulmonary artery or capillary wedge pressures. Pharmacology: CORVERT produces a mild slowing of the atrioventricular conduction and a dose-dependent increase of the QT interval. CORVERT produces no clinically significant effect on QRS duration at intravenous doses up to 0.03 mg/kg administered over a 10-minute period. Ibutilide may prolong the AH-interval and affect sinus cycle length and maximum corrected sinus node recovery time. Clinical trials: In clinical trials in patients with atrial flutter and atrial fibrillation with a maximum duration of 90 days, ibutilide fumarate was given in doses up to 2 mg. Atrial flutter was converted into sinus rhythm in 48-76% and atrial fibrillation in 22-51% of the treated patients. Placebo treatment resulted in conversion for 0-3%. The rate of conversion is dependent on the duration of the arrhythmia as shown in the following table. Duration of arrhythmia 0 - 3 days 4 - 30 days > 30 days 5.2 Success rate in atrial fibrillation (success/total patients) 45% (45/99) 31% (29/93) 20% (23/114) Success rate in atrial flutter (success/total patients) 67% 62% 34% (30/45) (50/81) (10/29) Pharmacokinetic properties The pharmacokinetics of ibutilide fumarate are linear within the dose range 0.01 to 0.1 mg/kg. Both enantiomers have similar pharmacokinetic properties. After an intravenous infusion plasma concentrations decline in a multiexponential fashion that varies between patients. Distribution: Protein binding is moderate, around 41%, and is therefore assumed not to influence the protein binding of other drugs. The volume of distribution at steady state in healthy volunteers is 11±4 L/kg, indicating extensive tissue distribution. Metabolism: Ibutilide is probably metabolised by cytochrome P450. Eight metabolites have been identified in urine. These metabolites are thought to be formed primarily by -oxidation followed by sequential -oxidation of the heptyl side chain. Seven of the metabolites exhibit little pharmacologic effect relative to ibutilide. The initial metabolite possesses in vitro activity similar to ibutilide but the plasma concentrations are less than 1% of ibutilide concentrations and thus it is assumed not to contribute to the overall pharmacologic effect. Elimination: Ibutilide has a high clearance, of the order of liver blood flow, 29+7 ml/min/kg. The initial halflife is short, around 1.5 minutes, the terminal half life is approximately 6 (range 2 -12) hours. In healthy volunteers 82% (78% within 24 hours) of the dose was excreted in the urine (6.7+1.8% of the dose as unchanged ibutilide) within 4 days of administration. The remainder (19%) was recovered in the feces within 7 days. 5.3 Preclinical safety data Preclinical data reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity and genotoxicity. In one species, the rat, studies have shown embryotoxic and teratogenic effects. However animal studies are insufficient to conclude (See section 4.6 Pregnancy and lactation). 6 PHARMACEUTICAL PARTICULARS 6.1 List of excipients Sodium Acetate (Granular Trihydrate) Sodium Chloride Sodium Hydroxide Solution 10% Hydrochloric Acid Solution 10% Water for Injections 6.2 Incompatibilities Not applicable 6.3 Shelf life 3 years Corvert as a single dose vial should be used only once and the admixture solution is chemically and physically stable for 24 hours at 25oC From a microbiological point of view, the product should be used immediately. If not used immediately, in-use storage times and conditions prior to use are the responsibility of the user and should not be longer than 24 hours at 2 oC to 8 oC, unless dilution has taken place in controlled and validated aseptic conditions 6.4 Special precautions for storage Do not store above 25oC. Do not refrigerate or freeze. Store in the original package. 6.5 Nature and contents of container Type I glass vial with rubber plug and aluminum cap, 10 ml pack size. 6.6 Special precautions for disposal and other handling CORVERT may be given in the concentrated form or diluted. One vial of 10 ml may be diluted with 50 ml solution for infusion. For post cardiac surgery patients, 5 ml may be diluted with 50 ml solution for infusion. The following diluents are compatible with CORVERT: Glucose 50 mg/ml (5%) solution for infusion Sodium Chloride 9 mg/ml (0,9%) solution for infusion Admixtures of the solution are compatible with polyvinyl chloride bags (PVC) and polyolefin bags. Allow the solution to obtain room temperature before infusion. Any unused product or waste material should be disposed of in accordance with local requirements. 7 MARKETING AUTHORISATION HOLDER To be completed nationally 8 MARKETING AUTHORISATION NUMBER(S) To be completed nationally 9 DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION 1996-12-13/2006-10-01 10 DATE OF REVISION OF THE TEXT 2011-06-09