Defibrillation and Cardioversion
advertisement

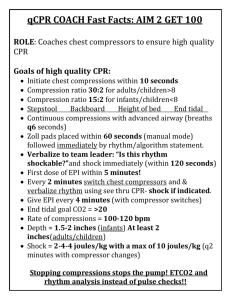
Defibrillation and Cardioversion 9/1/04 Hi all. Another one! As usual, please remember that this is not an “official” reference in any way at all – it’s what a preceptor would teach to a new orientee at the shop-floor level. Please let me know when you find mistakes – I’ll fix them right away. Thanks! 1- What is fibrillation? 1-1: What is atrial fibrillation? 1-2: What is ventricular fibrillation? 2- What is de-fibrillation? 3- What is cardioversion? 4- What is a defibrillator? 4-1: the monitor 4-2: the capacitor 4-3: the numbered buttons 1,2,3; output dials 4-4: the paddles and the pads 5- How do defibrillators work? 5-1: What is depolarization? 5-2: What does electricity have to do with it? 5-3: What is a joule? 5-4: What is monophasic defibrillation? 5-5: What is biphasic defibrillation? 5-6: What is “transthoracic impedance”? 6- How do I cardiovert someone? 6-1: Cardioverting a-fib. 6-2: Cardioverting VT-with-a-pressure. 7- How do I defibrillate someone? 7-1: Defibrillating VT 7-2: Defibrillating VF 8- What bad things do I have to watch for during cardioversion or defibrillation? 8-1: Using synchronization correctly. 8-2: Keeping the process orderly. 8-3: Clearing the bed. 8-4: Using contact gel properly – contact burns. 9- What things should I do after the cardioversion/defibrillation? 1- What is fibrillation? Fibrillation is an arrhythmia that affects either the atria as a pair, or the ventricles as a pair, producing “a-fib”, or “v-fib”, respectively. (Come to think of it, if a person is in VF, do their atria fibrillate as well? Does it matter?) Most cardiac rhythms are organized – they’re regular in some way, producing some sort of regular (as opposed to disorganized), rhythmic motion of the chambers, hopefully producing a blood pressure. In fibrillation, the cardiac tissue of the chambers involved wiggles about like (classic phrase) “a bag of worms”. Does a chamber wiggling like a bag of worms pump any blood, produce a cardiac output, eject any fraction of its contents? No, it does not! As I always try to point out, all the waves that you see on EKG strips actually represent some kind of physical motion of one or the other set of cardiac chambers, and the trick is to try to visualize what those chambers are doing in any given rhythm situation. Let’s see if a quick review of some strips helps the visualization process. Can I have the first slide please? 2 Here we are: look familiar? Sinus rhythm. Organized, rhythmic, producing stable contraction of the chambers – first the atria, then the ventricles. So - visualizing on the mental screen, that’s what I see: nice orderly motion, first above, then below. Okay so far? Right – next slide, please. OK: atrial flutter. Still organized: the atria are contracting rapidly, sure, at about 300 bpm, and the ventricles are responding to every third or fourth impulse, slowly enough that the ventricular chambers have time to fill up nicely between beats, fast enough to probably maintain a good blood pressure. So I visualize the atria clipping along, with the ventricles contracting every third or fourth time. This one? Well – is it organized? Actually it is: see the pattern of doubles? It’s a little easier to figure out by looking at the lower part of the strip – this is a sinus rhythm, and after every sinus beat comes a PAC, followed by a compensatory pause. So yes, still organized. “Regularly irregular”. How about this one? Yup, VT. Ugly, scary, but still organized, regular – the chambers (which ones?) are moving in a steady manner. On your mental screen you should see the ventricular walls contracting very rapidly – do they have time to fill? Should we shock this rhythm? It depends… 3 1-1: What is atrial fibrillation? How about this one? Not organized? Should we shock this rhythm? A-fib for sure can be a shockable rhythm, but look at the QRS rate – in the 70’s. What would have to be happening to make this a shockable situation? What do you visualize here? Atria: bag of worms. Ventricles – occasional, but normally conducted QRS’s. Are they too slow or too fast to make a blood pressure? How do you tell? 1-2: What is ventricular fibrillation? Here’s an ugly one - you probably recognize this one right off. Doesn’t look organized to me! What rhythm is this? Visualize the ventricles – everybody see the worms? What should we do? 2- What is de-fibrillation? So: all set on organized, and not organized? The treatment for nasty arrhythmias is often electical, right? The point is: one type of treatment: cardioversion - is for the organized kind of rhythm, and the other is, uh…for the other kind! Defibrillation is for disorganized rhythms. What you want to do is to send a fixed amount of electrical energy along the normal conduction path of the heart: along the Lead II pathway. Can I have the next slide please? 4 (What’s this one? Oh yeah...) Audience, this is the foxglove plant, the one that digitalis comes from. (The Chief Review Editor likes flowers…) Here’s a diagram of the normal lead II: the positive electrode is down near the apex of the ventricles, the negative one is at the atrial end. Everybody remembers that the normal direction that the cardiac impulse takes is from the SA node at the northwest corner, up near Oregon, down and towards the southeast in Florida, where the positive electrode lives? And that the signal moves along the pathway as the cells depolarize, in sequence, along that pathway? Negative electrode goes here (Oregon) (here) (Ground electrode goes here…) (here) Positive electrode here (Florida) www.arrhythmia.org/ general/whatis/ The idea is that applying an electrical impulse - of a specified amount of power - along the conduction pathway should depolarize all the rhythm-generating-and-transmitting cells at once. Bam! (Emeril? That you?) Now, hopefully, one of the normal, built-in, “intrinsic” pacemakers will take over – and in fact, often enough, they do! Remember: Defibrillation is the method to use in disorganized rhythms like VF, as in “Go defibrillate that disorganized rhythm, you doofus!” (Got to watch your language in those emergency situations.) 5 2- What is cardioversion? This is the other one. Cardioversion is the electrical maneuver that you use for organized rhythms.The difference between cardioversion and defibrillation is pretty simple – the secret lies in timing the shock correctly. If you’re treating an organized rhythm, and if the electricity you give the patient happens to arrive during the “vulnerable” period of the T-wave, then the unhappy “Ron-T” thing may occur. Everybody remember what that is?- an ectopic beat, (or a jolt of external electricity – in either case a stimulating electrical signal) landing in the conduction system during the vulnerable period can trigger VF. Bad! So – how to prevent this ugly thing? The defibrillator/cardioverter has the ability to track the QRS’s, and to stick a visible marker on each one. This lets the machine figure out when it’s safe to deliver the jolt. All too well do I remember seeing a patient once, cardioverted out of an a-fib with the machine in defib mode – that’s to say, not synchronized (forgot to push the “Sync” button, did ya?) – and who immediately went into VF, which responded to a defib shock. Fortunately. The three situations where I’ve seen cardioversions occur are: - Decompensated, rapid atrial fibrillation (afib with “RVR”: rapid ventricular response”) – this means that the ventricular response rate to the a-fib is so fast that the chambers can’t fill with blood between the beats. No filling, no blood pressure. Generally if a patient is in rapid a-fib and still has a blood pressure, the team will try meds first: verapamil, beta-blockers, etc. - VT-with-a-pressure (as opposed to VT- with-no-pressure; what ACLS calls “pulseless VT”). More on how to actually do a cardioversion below. - SVTs: narrow-complex rhythms, which are usually really bloody fast – up in the 200’s. Can your ventricles fill and empty properly at that rate? Mine can’t, mate! All organized rhythms. “Organized” is of course pretty relative: AF is a sort of “just-aboutorganized-enough” rhythm. 4- What is a defibrillator? The goal here is to try to understand what the machine is trying to do. Let’s say your patient pops into a nasty rhythm – not handling it very well, not making much of a blood pressure; and you want to deliver electricity – what do you need? 4-1: The monitor. First: you need to be able to see what’s going on. This is of course one of the reasons why our patients are monitored at the bedside: so you can see what rhythm your patient is in. Defibrillators are built to travel– so they have a monitor screen built in. Second: suppose you want to cardiovert instead of defibrillate – in other words, deliver a timed shock rather than a blind one. The machine is going to need to see the rhythm to do this, and you need to be able to make sure it’s seeing the right thing. This is a useful concept: lots of the devices in the unit are trying to “see” the patient in one way or the other – your job is to make sure they do, and that you learn how to interpret what they’re trying to tell you. 6 Anyhow, the machine needs to see the patient. You’re either going to have to put sensing wires on the patient that go back into the defibrillator (which may not have time for), or use the paddles as sensors. Our machines have a paddle-monitor mode called “quick look” – the procedure is to gel up the paddles, make sure the monitor is in paddle mode (the word ‘paddle’ appears on our monitors’ screens). Hold the paddles firmly against the skin in the defib position (with gel!) and get a good look at the patient’s rhythm. I bet that the newer defib pads do the same thing. I should know this… 4-2: The capacitor. Unless you have a really long electric cord, you’ll need a battery to run any transportable medical device. Rechargeable batteries are why all these devices are so flippin’ heavy, and the defibrillator is no exception, so we keep ours on rolling carts that we can whip up and down the unit. The battery stores electricity, but only if the machine is plugged in when you’re not using it. You do not want to arrive on the scene with a dead defibrillator! The battery feeds electricity into a capacitor – this I think of as a black box that holds whatever amount of electricity you choose, for a fixed amount of time. The capacitor fills up with electricity when you push the button that selects the charge you want to give. Our machines charge up with sounds that let you know what’s happening: once you push the button, you hear a rising whine as the charge collects - that turns into a steady, high-pitched whistle when the machine is ready to discharge. Loud, but effective. Practice this. 4-3: Numbered buttons: 1,2,3: output dials Here the goal is to try to keep things very simple: there are three things you need to do when operating the defibrillator, and the people who make these machines are trying to help you do them when you may be, let us say, a bit distracted by the situation. I’m going by the machines in our institution here – make sure you know what to do with your own, although the three moves are probably the same: 1: Button number one (actually on our machines it’s a dial, but it has a big number one next to it) turns the machine on, and sets the machine with the joules (the amount of electrical energy) you want to give. 2: Button number two charges the capacitor to the level you picked. At this point we hear the rising tones that tell you that the capacitor is charging up, and then the steady tone that says that it’s ready to go. 3: Button number three lives on the paddles (there are actually two “number three” buttons, so you don’t squeeze just one by mistake and fire the device before you’re ready) and discharges them. 4-4: The paddles and the pads: I hear that (rather like myself), paddles are considered “old-tech” – nowadays the thing to do is to slap on sticky defibrillation pads that hook up to the machine – the same ones as external pacing pads – then stand back, charge and discharge the machine from a few feet away. I have seen this done, but most times in our unit we make one quick defib move or two – there’s much less defibrillating going on since clotbusters came along and fewer people complete their MI’s. 7 In the MICU, I think that the pads are more for the elective cardioversion kind of maneuver rather than the emergent defibrillation thing. The critical point is that you really want to just jump in there and shock that rhythm – you don’t want to futz around with the pad packaging, the wires, changing the cable connectors so the pads are hooked up instead of the paddles…get the job done quickly. If the paddles are hooked up and ready, use them – don’t waste time; you can hook up the pads later and leave them on the patient for use if the problem happens again. 5- How do defibrillators work? 5-1: What is depolarization? (I have to stick this in: my son pointed out a while ago that when a white bear is captured, and taken from his iceberg to the zoo, he becomes “de-polarized”. Excellent!) Here’s how I understand it. Cardiac pacing and conduction cells work by a sort of magic ion pump dance: the concentrated ions on the outside of the cells all flow inwards at once, then outwards again. Swoosh, swoosh. The charges around the cell reverse as the ions flow in, or out, and the polarity flips: the cells are de-polarized – then re-polarized. Is that clever engineering, or what? In the process of the depolarization dance along the cardiac conduction pathway, a measurable electrical energy is generated: (P-wave for atria, QRS for ventricles – remember?) Then repolarized. (T-wave.) The conduction cells do this dance in sequence, along the conduction route from the SA node to the AV node, along through the bundle of His, (hey - where’s Her bundle?) and on downwards through the bundle branches into the contractile tissues in the ventricles. Fine so far. But what happens in a lethal arrythmia? The big sign hanging on the inside of the walls of the ventricles says: “whosoever shall paceth these walls the fastest, shall captureth.” Right?- the fastest pacemaker always captures the heart. So what to do when a rapid, excitable, unpleasant little terrorist pacemaker down in the ventricles somewhere has taken over the rhythm, and generates VT? 5-2: What does electricity have to do with it? As we saw, it turns out that applying a jolt of electricity along the conduction pathway makes all the cells depolarize at once, interrupting the sequence. In sinus rhythm the conduction cells do their sequential dance along the normal route. In VT, they establish some other route – backwards along the normal conduction path? (Anybody know who the EPS fellow is this month?) Depolarizing all the cells at once interrupts the sequence as it’s travelling – in whatever direction and hopefully lets one of the intrinsic pacemakers take over. Which hopefully it does - but sometimes doesn’t…what can you do then? 5-3: What is a joule? (I always tell my family that they’re my joules.) Well. This is so incredibly simple that no one should have any trouble with it. Ready? Here’s the encyclopedia: “Joule: unit of work or energy…equal to the work done by a force of one newton acting through one metre….it equals 107 ergs, or approximately 0.7377 foot-pounds. In electrical terms, the joule equals one watt-second – i.e. the energy released in one second by a current of one ampere through a resistance of one ohm.” I can’t understand why I even had to mention this subject. I mean, really! 8 Here’s the way I think of it. A joule is a hunk of electricity. You need a certain amount of electricity to cardiovert or defibrillate. That electricity is measured in joules. Fortunately for us, the medical engineering folks have done all the worrying about this, and made nice machines that fill themselves up with the right amount of joules when we ask them to. Let us never forget that we know about these amounts through the generosity of many, many selfless dogs, who went to heaven with frisbees and bones awaiting them (only beef, not chicken), never knowing that they gave their lives for us…thanks, dogs. Another way to think of it: I remember being told once that 360 joules is about the same amount of power that’s required to start a big diesel truck engine. (!) 5-4: What is monophasic defibrillation? “Monophasic” means that the current delivered by the machine travels in only one direction between the paddles. This has been the standard way of doing things for many years, but is now (like your preceptor) seen as out of date, and is being replaced with a newer method, called “biphasic” defibrillation. 5-5: What is biphasic defibrillation? Biphasic means that the current initially moves towards the positive paddle, then reverses direction and heads the other way. (My daughter used to drive this way.) The difference for us at the bedside is that biphasic shocks seem to be just as effective as the monophasic ones, but at lower power levels. This is a good thing for a couple of reasons: first, less power applied means less trauma to the patient. Second, less power required means longer battery life, and apparently all implanted defibrillators now use biphasic shocks for this reason – they can also be made smaller. I remember seeing patients come in with what looked like a small brick implanted under the skin of their chests… 5-6: What is transthoracic impedance? This is the electrical resistance that the patient’s chest creates between the paddles. If it’s high, then more electricity will be needed to successfully shock the patient. Apparently the new automatic external defibrillators that are being put in airports, phone booths and lunchboxes practically are able to automatically measure a patient’s impedance, and adjust the amount of electricity they deliver to match: less for a small person, more for a large one – just the right amount. Nice trick! 6- How do I cardiovert someone? Okay – let’s cardiovert somebody. Any volunteers from the audience? Many of the moves that you will make in either cardioversion or defibrillation are the same – so let’s go over the basics first, and then we’ll get to the specifics. Let’s remember that the decision to cardiovert means that your patient is not-quite-in-a-code-yet. As in every critical situation, remember: there’s time - more time than you think - available for you to make sure of your plan. How long until anoxic brain injury – 3 to 6 minutes, right? Five minutes 9 times sixty, that’s 360 seconds – a lot of seconds! There is always all the time you need. Let’s take a little of that time now to look at what needs to be set up: Make sure that you have everybody you need. In our hospital, elective cardioversions are supposed to include the presence of anesthesia, in case the patient codes and needs intubation. You certainly want to have the team coming if you start a non-elective electrical maneuver! Make sure your patient has IV access. More is better. If my patient were being intubated (this situation might turn into an intubation), I’d have a gravity bag dripping slowly. Make sure your line isn’t infiltrated. (How?) Make sure your patient is unconscious, or appropriately sedated. This is not a procedure to do on someone who’s awake. Make sure your patient is oxygenated. Why is your patient doing this rhythm in the first place? Ischemia? Or is the rhythm itself creating ischemia, because the heart is using up all the oxygen it’s getting, going so fast, but still needs more? (That’s what they mean by “rate-related ischemia”.) Anyhow, more oxygen to the myocardium is usually better than less, so apply some! (Does your patient have COPD? Why am I asking?) The Buttons: Button One: Turn the machine on, and pick the amount of energy you want to give. The ranges vary for different situations, but the general rules seem to be: for cardioversion start low – usually 50 joules for example, for elective cardioversion out of a “relatively” stable, a-fib with RVR. For VT/VF, ACLS says to start with 200 joules. (That’s the monophasic machine number – with the biphasic machine you start with 150 joules.) Usually you turn a twisty dial control to set the joules level. The numbers are clear, and there’s a simple arrow pointer that you line up with the number that you want. Make it a practice, every now and then, to go over to the machine and make sure you know how to work it. Familiarity comes with time, so do this a couple of times every week - at least when you’re starting out in the units. Obviously, you don’t want to have to stand there trying to figure out how the machine works in the middle of some busy situation. At this point, make sure your patient’s rhythm is clearly visible on the defibrillator monitor. Cardioversion is by definition elective, so you should have time to do these things, or you’d be defibrillating, right? In this situation, take the time to connect the patient to the defibrillator’s sensing cable. External pacing boxes use the same method – generally, they have to see the patient somehow. Three sticky electrodes set up a standard lead II. Three wires go to a thicker cable, the cable plugs into a socket on the machine, and you should see the rhythm clearly. The monitor should let you choose between leads I, II , III (or paddle view –but that’s for quicklook, usually in defib) – choose the one that gives the clearest upright QRS waveform, Now comes the “synch” button. This is what makes cardioversion different from defibrillation, and you absolutely must use this properly. Luckily, it’s not hard at all. Push the button. You should see a blip, or a dot of some kind that the machine puts on each QRS – this shows you that the machine clearly sees the QRS, and knows when to deliver the shock – remember that cardioversion has to be properly timed to avoid the T-wave. Here’s an important point about the difference between cardioversion and defibrillation: with the synchronization on, the machine will wait after you hit the discharge buttons to make sure of it’s 10 timing, and it won’t discharge until it’s ready. So be prepared to hold those paddles down, hit those buttons, and wait – it might only be a second or two, but if you’re not ready for what the machine is doing, you may decide that it’s not working. Button Two: Charge the machine. Listen for the charging tones. Button Three: This discharges the electricity from the paddles, so make sure that everything is quite ready before you do this. Several things need to happen: Make sure the paddles have conduction gel on them. The electricity will not be properly transmitted to the chest wall without it. Also, even with the gel these paddles will often cause a second-degree skin burn – imagine what would happen without the gel! Make sure that you’ve cleared the bed. This means that just before defibrillating, you take a quick but careful look around to make sure that no one is holding onto the bed, or leaning on it. You should not be leaning against the bed either – you should get the rails down, and then lean over the patient with the paddles in your hands. Yes, it’s true that modern beds are electrically designed so well that any stray electricity should go into the grounding system, but would you want to be wrong and have to shock your friend the pharmacist who was leaning over the bottom of the bed, after you put him into VT? Bed’s clear? Steady tone from the machine? Place the paddles on the chest – here’s an image from the web… I know – if it’s elective, we’re supposed to be using the pads. What if you don’t got no pads? What if you’re in the CT scanner? Or MRI? Should you go running into the scanner room with the defibrillator? (NO!) What should you do? Who knows what the round silver thing is? Has to do with implanted pacemakers… http://www.usuhs.mil/psl/images/defib.JPG The idea is that the paddles are sending current from one end of the heart to the other: see that? The upper paddle sits where the negative lead II electrode lives, and the lower one sits where the positive electrode lives, so the current travels along the normal conduction path, and so depolarizes the whole system at once. (I know: I repeat myself a lot – my kids remind me all the time. Those stupid ginkgo pills – I can never remember to take them…) Hold the paddles down firmly – the book says 25 pounds of pressure – which is more than you might think. My wife brings a scale to her ACLS classes, and has the student press the paddles 11 down on the scale until it reads 25 pounds. (Is she smart or what?) It turns out to be a lot of pressure. Clear the bed. Yes, apparently it is quite true that the current can be transmitted to someone leaning on, or holding onto the patient’s bed. “One, I’m clear! Two – you’re clear! Three – everybody’s clear!” Push the third button. Our paddles have a button number three on each of them, so that you don’t mistake: you have to hit both, deliberately, to discharge the paddles. Remember now: are you defibrillating or cardioverting here? Will the paddles discharge right away, or will they wait – and should you? Watch the patient and the monitor at the same time – this is why you have two eyes, right?, to watch two things at once? Ask an old ICU nurse how many things he can watch at once…did the rhythm convert to normal sinus? Or VT? Or worse? Or was there no change at all? What’s the patient’s pressure like? What’s the sat like? What’s your pressure like? Ok – let’s do the pads. There’s some discussion about where they should go: This way, they take the same positions as the paddles would, right? http://www.virtualcpr.com/images/defib_pos.jpg This is the other way: “anteroposterior” pad placement. There’s all sorts of learned argument about which way works better – but we’ve recently gone with this one. This pad arrangement does seem to work better for transcutaneous pacing… All other things being equal, the pads really are a nice development. They’re larger in area than the paddles, and much stickier, which means less chance of burns, better transmission of the electricity…just make sure you know which method to use, and when. 12 6-1: Cardioverting A-fib: Here’s a nice strip of a not really too rapid a-fib, followed by artifact from the shock, and then – what? It’s a little fuzzy - I’ve blown it up a bit too big on purpose so you can really see. See the shock artifact – the big ugly thing there? How about this next one? Did it work? What’s the rhythm after the shock? My wife the ACLS instructor says that you should start with low monophasic discharge settings, 50 joules, followed by 100, then 200, then 300 if the patient doesn’t convert. A chart out on the web says that the equivalent biphasic shocks would be: 70, 120, 150, and 170 joules. After that, you might have to try chemical maneuvers again. Then again, it does pay to think a little about why your patient is doing this rhythm in the first place. Is she septic? Does the rapid rhythm mean that her heart is trying to keep the her pressure up in the face of a totally dilated arterial bed? Maybe she’s dry. Maybe ischemic. Maybe all of the above. Maybe she’s being totally stressed because of vent-weaning trials that she’s not ready for – how does the rhythm fit into the whole picture? It always pays to think about these things… 6-2: Cardioverting VT-with-a-pressure: As opposed to VT-with-no-pressure, right? This scenario is a little closer to a real code situation than the a-fib one, because these folks are very likely to lose whatever pressure they’ve got, at any time. Jayne says that you should set up for an elective cardioversion if you’ve got the time, but be ready to defibrillate pulseless VT at a moment’s notice. In practice, if your patient is sitting there smiling at you while in VT on the monitor, the team will try chemical cardioversion first. Up until recently this involved a lidocaine bolus, followed by a drip, then maybe procainamide – nowadays I understand that the first drug to try is amiodarone, 300mg IV over ten minutes, followed by a drip, and then maybe the procaine. Would someone please find out and let me know? 13 7- How do I defibrillate someone? 7-1: Defibrillating pulseless VT 7-2: Defibrillating VF This is by definition a code. In this situation the ACLS is very clear: shock them first. I would just add – establish unresponsiveness, right? Could be embarrassing if the rhythm turned out to be monitor artifact of some kind. (Ask me how I learned that.) It also helps to remember if your patient is a DNR… Here’s a pretty good strip, probably from an electrophysiology lab: the official description says that what’s happening here is first sinus rhythm, then pacing impulses to induce VT – then a defibrillation shock, and then – what? CCU nurses: what rhythm does that look like, there in the middle? Anybody got some mag in her pocket? Defibrillation is obviously not an elective procedure – the studies show that the most effective thing to do in both pulseless VT and VF is go right on in there and shock them, starting with 200, then 300, then 360 joules (or 150/150/150 when using a biphasic device.) In this situation you don’t wait for the paddles to see the patient’s rhythm, you don’t wait for anything. One thing you should do is to keep the paddles on the patient’s chest between the shocks (“Shock shock shock!”) – they may be the only system you have running to monitor the patient’s rhythm. The monitor should be set to “paddle view” when defibbing – there’s a button marked “lead” – push it a couple of times to cycle through views until the monitor screen says “paddles” – but do that after you’ve shocked the patient! 8- What bad things do I have to watch for during cardioversion or defibrillation? We’ve covered a lot of them already: - - Don’t shock a patient who’s awake! Don’t forget to synchronize when cardioverting – a-fib can be turned into v-fib this way. Don’t forget the conduction gel. Don’t forget to clear the bed. Try to keep the process orderly. This means keeping yourself calm and deliberate when you’re not really sure you can. Set up systematically. Set up communication with the appropriate team member for orders – don’t take orders from two doctors at once! Do your best. Remember that no matter what situation you’re in, you may shortly be in a fullfledged code – make sure that backup help is on the way. 14 9- What things should I do after cardioversion/defibrillation? - Monitor the patient carefully – is the patient staying in the converted rhythm? - Keep the patient well-oxygenated. This is not the time to wean your patient’s oxygen! I would aim for a sat no lower than 98%. Remember however, about COPD patients and oxygen treatment… - Check up on your patient’s labs – does she need K+, or magnesium? Is she acidotic? – not a helpful thing. - Get a 12-lead after the cardioversion for documentation- was the patient having chest pain? Does she still? Is it gone now? Can she tell? - Talk to the team about cycling re-CPK’s and troponin studies. - Assess the patient’s skin – does he need treatment for skin burns?