Cardiovascular 21 – Thrombosis, Infarction and Embolism
advertisement

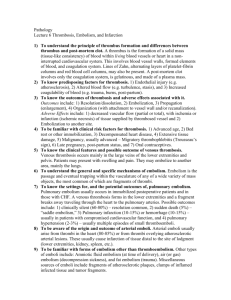
Cardio 21 – Thrombosis, Infarction and Embolism Anil Chopra 1. Define thrombus, embolus, and infarction. Thrombosis Pathological opposite of haemostasis. Inappropriate activation of normal haemostatic processes (e.g. if blood clot forms in uninjured or minorly injured vessel) Can develop in vein or artery Clot itself is known as a thrombus. Can become thrombo-embolism if a chunk breaks off. Embolus Something travelling in the blood stream that could potentially lodge itself in a blood vessel and block it. E.g. detached blood clot, bacteria clump, gas, fat droplet, tumour. Most are dislodged thrombi parts. Can be a consequence of infarction. Infarction An area of ischaemic (caused by lack of O2) necrosis (tissue death) by the occlusion of either arterial supply or venous drainage. E.g. myocardial infarction caused by death of the heart muscle due to atherosclerosis of coronary artery. 2. Define Virchow’s triad and compare/contrast the 3 elements. Virchow’s triad consists of 3 elements which are thought to contribute to the formation of a venous thrombosis. (1) endothelial injury (2) stasis/turbulence of blood flow (3) hypercoagulation of blood 3. Which of the triad has a dominant influence? ENDOTHELIAL INJURY has the most dominant effect on arterial thrombosis. Endothelium is supposed to act as a barrier, and anti-adhesive and anti-coagulant. Also produces nitrous oxide to mediate the relaxation of vessel wall. Normally AT III (anti-thrombin III) inhibits thrombin Normally tPA (tissue Plasminogen Activator) promotes fibrinolysis. Normally PGI2 (prostaglandin I2) inhibits platelet activation. Normally low E-selectin decreases cell adhesion and stops inflammation. Normally low VCAM1 also decreases cell adhesion If the endothelium is activated Barrier function is lost High E-selectin and high VCAM 1 also result in monocyte recruitment. If the endothelium becomes damaged Nitrous oxide levels decrease Platelet adhesion is increased. Fibrinolysis is decreased. Prostacyclin is decreased. Thrombosis is increased Exposure of subendothelial collagen which exposes tissue factor, depletes prostaglandin and tissue plasminogen activator. Resting vascular endothelium Activation or denudation of endothelium Provides barrier function Anti-thrombotic surface ↑ ATIII ↑ tPA ↑ PGI2 Anti-adhesive surface Loss of barrier function AT-III inhibits thrombin tPA promotes fibrinolysis PGI2 inhibits platelet activation mediates endothelial dependent relaxation ↓ thrombosis ↑ fibrinolysis ↓ E-selectin ↓ VCAM-1 Loss of vascular tone ENDOTHELIAL DAMAGE Decreased NO Increased platelet adhesion Decreased fibrinolysis Decreased Prostacyclin ↑ thrombosis ↓ fibrinolysis Loss of vascular tone ↓ PGI2 Thrombus formation / platelet aggregation 4. In what clinical situations is endothelial injury important? Endothelial Injury is Important in: Myocardial infarction Valvulitis (inflammation of heart valves) Ulcerated plaques Sites of Inflammation Hypertension Smoking ↑ PGI2 Thrombus formation / platelet aggregation ↑ E-sel. ↑ VCAM ↑ MCP-1 Monocyte recruitment 5. Describe normal blood flow and the importance of turbulence and stasis to thrombus formation. Blood Flow Blood flow is normally laminar (i.e. the central parts flow quicker than the peripheral regions) so the cellular elements of the blood flow centrally, and the slower moving outer fluid separates cells from endothelium If there is turbulence, endothelial injury/dysfunction can occur forming stasis (stopping of body fluid movement). This brings platelets into contact with the endothelium, increases the concentration of clotting factors and slows down the flow of clotting factor inhibitors, which contribute to thrombosis. 6. In what clinical situations is alteration of blood flow particularly important. Hypercoagulability (& stasis) important in: Congestive heart failure Trauma (burns) Surgery Puerperal (just after childbirth) and postpartum (long after childbirth). Disseminated carcinoma (Trousseau syndrome). 7. List some of the more important genetic and acquired causes of Hypercoagulability states. Inherited Hypercoagulability Factor V Leiden: results in lack of “natural” anticoagulants, antithrombin III, protein C or S. Elevated levels of homocysteine, can cause homocysteinuria which results in increased risk of thrombosis. Prothrombin 20210 Mutation, where an adenine is in place of a guanine in prothrombin in the 20210 position results in hypercoagulation leading high levels of prothrombin. Acquired Hypercoagulability Heparin (anticoagulant) induced thrombocytopenia (low platelet) Antiphospholipid antibody syndrome (autoimmune disease) Post surgery and post-childbirth 8. Describe the general morphology of thrombi. - Can occur anywhere in cardiovascular system Vary in shape and size. Arterial/cardiac thrombi usually begin at sites of turbulence or vessel injury. Venous thrombi usually begin at sites of stasis. Tail may fragment to become embolus. Before death they show up as alternating pale (platelets and fibrin) and dark (blood cell) lines. “Lines of Zahn”. After death, the blood tends to clot anyway forming a dark jelly like substance. 9. What are the morphological characteristics of arterial vs. venous thrombi & 10. Explain why thrombi are clinically important. What are the relevant differences between arterial and venous thrombi in terms of their clinical consequences? Types of Arterial Thrombi: Mural thrombus – adherence to wall of heart chamber Can form vegetations on heart valves following infection with the development of large thrombotic masses. Aortic thrombus – ulcerated atherosclerotic plaque/aneurismal dilation. In coronary, cerebral or femoral arteries, usually grey-white, easily broken up, firmly adherent, composed of platelets, fibrin, erythrocytes, leukocytes – “white thrombi”. Risk Factors for Arterial Thrombi - Atherosclerosis Aortic and peripheral oesophagus Hypercoagulability Vasculitis Catheterisation Types of Venous Thrombi (Phelbothrombosis) Tend to have more enmeshed erythrocytes “Red thrombi” More likely to become pulmonary embolism Occur with Hypercoagulability and stasis Occur in superficial (rarely embolised but cause swelling, pain, tenderness and may lead to varicose ulcers) or deep (embolise easily, usually are bypassed by collateral channels, most are asymptomatic) veins and legs DVT. Deep Vein Thrombosis - Usually develops in the thigh because the blood moves slowly here, usually if legs have not been moved for a long time blood pools in the area and a clot develops. Only 1% of venous thrombi cause complications. Shed to form emboli (pulmonary very serious) Pulmonary Embolism – emboli passes through right side of heart from leg and then travels to lings where it can occlude in pulmonary artery or in smaller arterioles. One embolus usually sparks off more. It can result in sudden death, right heart failure, most are clinically silent. Risk Factors for Venous Thrombi - Stasis - Trauma/surgery - Obesity - Congestive heart failure - Recent pregnancy - Hypercoagulability - Drug abuse - Birth control pill Fate of Thrombi EMBOLISE: break off DISSOLUTION: fibrinolytic pathways break them down ORGANISATION:(1) macrophages cause inflammation (2) Phagocytosis of thrombotic material (3) Regeneration of vessel wall RECANALISATION: re-establishment of blood flow, thrombus incorporated as subendothelial swelling. 10. Describe the pathogenesis and clinical consequences of fat embolism, gas embolism and amniotic fluid embolism. Embolism can be a detached solid liquid or gas that can potentially lodge themselves in and block a blood vessel. It continues to travel until it reaches a small enough vessel that it gets stuck. Systemic Thromboembolism: these are emboli that are travelling in the arterial circulation that generally tend to come from intracardiac mural thrombi. (Left ventricular infarction, dilated left atria, valvular vegetation, aortic aneurysms. Air/Gas Embolism: bubbles of air circulating in the blood which eventually lead to endothelial irritation. They are often caused by dividing and contain a mixture of O2, CO2 and nitrogen. Fat Embolism: a fat globule that travels in the blood usually following a long bone fracture. It results in occlusion of multiple blood vessels with fat globules that are too large to pass through capillaries. They do not however completely occlude vessels as fat droplets are fluid and easily deformed. This causes an asymptomatic period followed by pulmonary and neurological manifestations along with small petechial haemorrhages (small red dots on skin). Amniotic Fluid Embolism: amniotic fluid travels in blood during pregnancy and causes blockage of blood vessels, especially in the lung. Foetal cells & hair are also present. Amniotic fluid enters the uterine veins when: (1) amniotic sac is ruptured (2) uterine or cervical veins are ruptured (3) there is a pressure gradient from the uterus to the veins. The fluid then enters the maternal circulation and First – the patient experiences shortness of breath, extreme hypertension, cardiopulmonary arrest (low O2 to heart and lungs) and coma. Second – those who survive sill shiver, vomit, bleed heavily (blood loses coagulation ability). Foetal heart rate drops to 110bpm. 12 & 13. Outline the sequence of events following, factors that affect the development of, and the inciting events leading to infarction. Infarction An area of ischaemic necrosis due to lack of arterial supply or venous drainage. Usually secondary to thrombotic or embolic events. (Other events can include local vasospasm, expansion of atheroma, compression of vessel extrinsically, twisting of vessels due to trauma. Normally occur in the lungs (pulmonary), heart (myocardial), kidney (renal), brain (stroke), spleen. Development of infarct influenced by nature of vascular supply, rate of development of block, vulnerability of the tissue (to hypoxia), oxygen content of the blood. Venous infarcts are rare as venous thromboses usually occur in the leg were if the vessel is congested, by-pass channels open. Only occur if organ has single outflow. Red infarctions occur with venous occlusions, or those which allow blood to collect, those areas which have previously been congested and now have reestablished blood flow. White infarctions occur with arterial occlusions or in solid tissues where amount of haemorrhage is limited. They tend to show ischaemic, coagulative necrosis (except in the brain) Septic (caused by bacterial vegetation fragments) infarctions may develop as microbes seed necrotic tissues. Infarcts are thus converted to abscesses. Gangrene is a type of infarction that results in death of the tissue of the limbs (caused by blockage of a vessel and eventually reduction in O2 supply). It causes the skin to turn black and ooze pus. (generally it occurs in arms and legs but can occur in any part of the body). There are 2 types of gangrene: o Dry gangrene is caused by disturbance of blood supply to tissue usually caused by injury. o Moist gangrene is caused by toxin-producing bacteria. The skin looks as if it has bubbles beneath it. Pus and infection spread quickly. Risk factors for gangrene Diabetes / Atherosclerosis / Injury / Surgery / Immunosuppresion / Infection / Smoking / Alcohol / Burns