Draw and describe the circuitry of a cerebellar nucleus: Include
advertisement
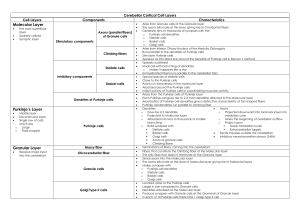
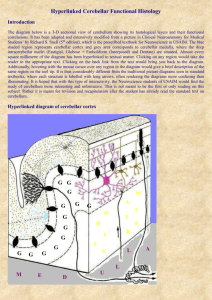
MSP Neuroscience Problem Set #2 1. Draw and label the circuitry of the cerebellar cortex. Include: inputs (climbing/mossy fibers), outputs (Purkinje cells, subcortical nuclei), and interneurons (granule cells plus basket, Golgi and stellate cells). Label synapses as excitatory or inhibitory. For the diagram of the cerebellar circuitry, see class notes page 3 and 5 All synapses are inhibitory except for granule cell synapses onto Purkinje cells (parallel fibers) and also the inputs from climbing/mossy fibers. 2. Both mossy fibers (via granule cells) and climbing fibers synapse onto the Purkinje cell. How does the location of the synapse (Purkinje soma and/or dendrite) and the number of synaptic contacts onto the Purkinje cell differ between these two cell types? What effect does this have on the electrical response of the Purkinje cell to synaptic input? Why is it “useful” to have two different kinds of inputs to the Purkinje cell? Each Purkinje cell is directly associated with only 1 or 2 climbing fibers [cf] (all climbing fibers come from the inferior olivary nucleus). Each cf makes 300-1000 synaptic contacts with the Purkinje cell they are associated with. Synapses are onto the soma and dendrites of the Purkinje cell. A cf evokes a very powerful, large EPSP in the Purkinje cell, and this triggers 3-10 action potentials (complex spike). Complex spike frequency is low (1-2/sec). In contrast, mossy fibers are indirectly associated with Purkinje cells (mossy fibers come from many sources). Mossy fibers synapse onto granule cells. The axons of granule cells (called parallel fibers) are arranged perpendicular to the dendritic fields of the Purkinje cells. Each granule cell can synapse with the dendrites of 45 Purkinje cells. According to the notes, a Purkinje cell can be affected by 7,000 mossy fibers! A Purkinje cell requires input from several parallel fibers in order for a small EPSP and a single action potential (simple spike) to be produced. The simple spike frequency can be high (10-50/sec). In summary, the Purkinje cells have 2 types of input. The first (cf) are from a single source, are directly associated in a 1:1 ratio with the Purkinje cell, and produce a powerful output. The second (mf) are from many sources, are indirectly associated with Purkinje cells, and produce small effects via summation. Having two vastly different inputs could theoretically be useful to the cerebellum since the two inputs could be compared for congruence – similar to a “checks and balances” system (other theories possible). 3. Complete the table on the next page, following the example provided. Note the major differences between the functional regions of the cerebellum, there are many patterns that make this information easier to remember! 4. If a patient suffers damage to the left, lateral side of his cerebellum, what functions might be affected and on what side of the body? Prepare a diagram showing the relevant circuitry. The lateral side of the cerebellum is primarily the neocerebellum. As shown in Q#3, damage to the neocerebellum causes incoordination of movement; the patient can present with: intention tremor dysmetria: inaccurate amplitude of movement asynergia: incoordination of agonist and antagonist muscles producing choppy movements decomposition of movement: absence of smooth execution of a sequence of movements ataxia: incoordination of movements dysdiadochokinesia: irregular pattern when pt attempts to perform rapid alternating movements dysarthria: speech difficulty. For cerebellar disease, it is a problem with sequencing syllables scanning speech nystagmus The pt will be affected on the LEFT side; lateral cerebellar damage causes ipsilateral deficits. See pg 11 of the class notes for the circuitry. The neocerebellum sends outputs via the dentate nucleus. There are two possible pathways – note that for both there are two decussations which result in same-side deficits: a. Dentate (decussate in the superior cerebellar peduncle) thalamus cortex pyramidal tract (decussation in the pyramidal decussation) b. Dentate (decussate in the superior cerebellar peduncle) red nucleus rubrospinal tract (which also decussates) 5. Draw and describe the BBB, separating it into the BBB and the blood-CSF barrier. Discuss the several ways in which a substance can cross this barrier to enter and exit the brain. The blood brain barrier, which separates the blood from the extracellular fluid (ECF) of the brain, is made up by the endothelial cells of the brain microvessels. There are tight junctions between these cells, which means that substances crossing the BBB must actually cross through the endothelial cell (as opposed to traveling between cells). Remind the students that although astrocyte processes surround brain capillaries, this is NOT the BBB. The choroid plexuses, the arachnoid membrane and the arachnoid villi comprise the bloodCSF barrier. There are tight junctions between the epithelial cells that make up these structures, so once again, substances must pass transcellularly to get past the blood-CSF barrier. Note that both components (the BBB and blood-CSF) are important since there is free exchange between the ECF and the CSF via the pia and the edendyma. Any change in CSF composition will be reflected in the composition of the ECF, and will affect neuronal/brain functioning. Thus, the composition of the CSF must be maintained very constant even if plasma composition is fluctuating. Clinical note: lumbar taps are especially useful to the neurologist/psychiatrist due to the fact CSF is a good representation of brain ECF! Substances can enter and exit the brain by the following mechanisms: Diffusion: hydrophobic, non polar molecules with a higher oil/water partition coefficient will enter the brain more readily than hydrophilic, polar molecules with a low oil/water partition coefficient Channels/pores: rate of entry determined by # of channels, permeability of channel, and driving forces present (concentration/voltage gradients) Facilitated diffusion Active transport Endocytosis If you want, mention that the permeability of the BBB to a substance may be increased during periods of inflammation, and this will effect drug delivery (little prelude to Pharm )