Title A critique on T t he Policy Statement of the American Academy
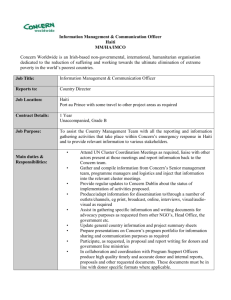
advertisement

1 Title 2 The Policy Statement of the American Academy of Pediatrics – Children as 3 Hematopoietic Stem Cell Donors – a proposal of amendments for better 4 protection of minors 5 6 Authors’ names 7 CHAN Tak Kwong 8 Assistant Professor, Anatomy, University of Hong Kong 9 Email: theo@hku.hk; Tel: 852-93863620; Fax: 852-28199205 10 Postal Address: L1-59, Laboratory Block, 21 Sassoon Road, Hong Kong 11 12 TIPOE George Lim 13 Associate Professor, Department of Anatomy, University of Hong Kong, 14 Hong Kong 15 Postal Address: L1-59, Laboratory Block, 21 Sassoon Road, Hong Kong 16 17 Correspondence to CHAN TK at theo@hku.hk 18 19 Word count: 2085 20 21 22 23 24 25 26 27 28 29 30 31 32 Keywords: policy, haematopoietic stem cell transplant, ethical concerns, donor siblings 1 1 2 3 Abstract: 4 With a view to addressing the moral concerns about the use of donor siblings, the 5 Policy Statement of the American Academy of Pediatrics - Children as Hematopoietic 6 Stem Cell Donors (the Policy) has laid out the criteria upon which tissue harvest from 7 a minor would be permissible. Background 8 9 Discussion 10 Although tissue harvest serves the best interests of recipient siblings, parents are also 11 obliged to act in the best interests of the donor sibling. Tissue harvest should proceed 12 if and only if it serves the best interests of both the donor and recipient. Parents 13 should be forbidden, and they are by law, to consent to tissue harvest unless there are 14 substantial benefits for an incompetent minor that can outweigh the potential harm. 15 There is no basis to subject a minor to the medical risks of tissue harvest if the 16 recipient sibling can wait without significant risks of complications until the donor 17 becomes Gillick competent. We also argue that the Policy fails to take into account 18 recent advances in haematopoietic transplantation from haploidentical donors or 19 related tissue-matched donors. As a proper ethical evaluation should have regard to 20 the availability of different types of suitable donors, fulfilling the criteria specified in 21 the Policy alone is not sufficient to justify tissue harvest from a donor sibling. 22 23 Summary 24 Unless a recipient sibling will suffer from serious complications or die without the 25 transplantation and no other medically equivalent donors are available, there is no 26 moral or legal basis to violate the donor sibling’s right to bodily integrity. 2 1 Accordingly, we propose that the Policy should be revised in order to fully address 2 our moral concerns in relation to tissue harvest from donor siblings. 3 4 BACKGROUND 5 6 In conjunction with preimplantation genetic diagnosis (PGD), assisted reproduction 7 can be used to avoid inheritable diseases. After successful in-vitro fertilization, PGD 8 can identify whether any of the embryos is affected by a genetic condition. Parents 9 now can even request selection of embryos on the basis of tissue type in order to 10 create a child to cure an existing sick child. In response to the moral concerns about 11 the use of paediatric haematopoietic cell donor siblings (donor siblings), the Policy 12 Statement of the American Academy of Pediatrics – Children as Hematopoietic Stem 13 Cell Donors (the Policy) suggests that tissue harvest should only proceed upon 14 satisfaction of all the following five criteria: 15 16 ‘(1) there is no medically equivalent histo-compatible adult relative who is willing 17 and able to donate; 18 (2) there is a strong personal and emotionally positive relationship between the donor 19 and recipient; 20 (3) there is some likelihood that the recipient will benefit from the transplantation; 21 (4) the clinical, emotional, and psychosocial risks to the donor are minimized and are 22 reasonable in relation to the benefits expected to accrue to the donor and to the 23 recipient; and 24 (5) parental permission and, where appropriate, child assent have been obtained.’1 3 1 Except that the fourth criterion requires the physician to minimise the risks of medical 2 procedures by, e.g. avoiding central venous catheter insertion and reducing 3 psychological risk by proper communication skills and the fifth requires that child 4 assent should be obtained where appropriate, the remaining criteria seem to merely 5 state the facts common to most cases of tissue harvest rather than regulating the 6 process. We contend that the Policy fails to sufficiently protect the interests of donor 7 siblings without addressing the availability of other types of donors and the type of 8 disease. 9 10 DISCUSSION 11 The legal and ethical principles 12 One would not dispute that tissue harvest serves the best interests of recipient siblings. 13 As one’s liberty cannot be allowed to such an extent that another person suffers 14 harm,2 a donor sibling does not have an obligation to save the life of the recipient 15 sibling given the medical risks of transplantation. A Gillick competent donor should 16 be free to make an informed decision of whether to save the life of a recipient 17 sibling.3 In case the donor sibling is an incompetent minor, a parent must proceed to 18 assess the best interests of the donor. The assessment of best interests is a balance of 19 the benefits and risks of transplantation for the donor. The procedures need not be risk 20 free but parents should only consent to tissue harvest if the possible benefits for the 21 donor outweigh the potential harm. Although parents have the rights to make 22 decisions for incompetent minors, the Children Act 1989 in the United Kingdom 23 empowers the court to intervene if parents fail to act in the best interests of both 24 children.4, 5 In Birmingham City Council v H (a minor), Balcombe LJ said the 25 question of welfare of both children should be approached ‘without giving one 4 1 priority over the other.’6 Although the parents’ wishes should command very great 2 respect, the court is to exercise an independent and objective judgment.7 The ethical 3 principles of beneficence and non-maleficence also demand that parents should 4 consent to tissue harvest only if it serves the best interests of both the donor and 5 recipient. 6 7 8 The best interests of donor siblings Well-documented risks 9 The most ethically sound basis to oppose tissue harvest is that it imposes risks of 10 bodily injuries associated with the medical procedures of tissue harvest. The risks 11 depend on the source of cells namely bone marrow, peripheral blood and umbilical 12 cord blood, each with their own benefits and risks. It is known that harvest by 13 umbilical cord blood carries no medical risks except in case of modified delivery. 14 Therefore my analysis below focuses on bone marrow and peripheral blood 15 transplantation only. Minor complications like pain at collection sites, fatigue and 16 pain may occur in a small proportion of donors (6%-20%). Major and life-threatening 17 complications following marrow donation like anesthesia-related events, injuries to 18 bones, sacroiliac joint and sciatic nerve were estimated to occur in 0.1%-0.3% of 19 cases.8 Major risks of peripheral blood transplantation are mainly associated with 20 sedation, general anaesthesia and central venous catheter insertion, estimated to be 21 about 1.1% of cases.9 In light of one’s inviolable right to bodily integrity, minors 22 should not be exposed to the medical risks unless there are well-established benefits 23 of a significant magnitude that they can accrue from tissue harvest. 24 Potential benefits 5 1 The possible benefits for donor siblings are merely psychosocial. In an American case 2 Curran v. Bosze, Calvo J said that ‘the psychological benefit is grounded firmly in the 3 fact that the donor and the recipient are known to each other in a family. There may be 4 a psychological benefit to the child from donating bone marrow to a sibling.’10 We 5 consider that tissue harvest can have short-term and long-term psychosocial effects 6 for donor siblings. When presented with the idea of donation, younger donors were 7 found to focus more on the immediate pain and the frightening experience of the 8 procedure,12 whereas older children might feel pressure from family members or 9 medical staff to become a donor.11 MacLeod and others found that about a third of the 10 siblings donors thought that doctors and family members limited their opportunity to 11 say no, making them perceive they had a ‘forced no choice’.12 And donor siblings 12 reported higher levels of anxiety and lower self-esteem than non-donor siblings,13 13 which may be attributed to the lack of choice in the decision to donate. It follows that 14 a donor sibling is more likely to have short-term psychosocial burdens rather than 15 benefits. 16 17 Long term positive effects for the donor siblings include greater sensitivity to the 18 needs of others14, enhanced self-sufficiency and independence15, increased family 19 closeness16, and most important of all, the possible companion of a healthy recipient 20 sibling. On the other hand, negative emotions were reported when their recipient 21 siblings developed long-lasting complications from the procedure. Furthermore, 22 anger, guilt, and blame were common amongst donor siblings with unsuccessful 23 transplant.12 While the Policy cited the findings of three studies that all donor siblings 24 agreed that the psychosocial benefits and harm of serving as a donor outweighed the 25 physical harms, Macleod,Wieners and others found that only 66.6% and 67% of 6 1 donor siblings reported a predominantly positive psychosocial experience.12, 17 2 Importantly, all reporting predominantly positive psychosocial experience had 3 successful transplant and only donors with unsuccessful transplant reported a 4 predominantly negative experience in Macleod’s study.12 As the psychosocial 5 experience is highly associated with the outcome for the recipient, we contend that the 6 long-term benefits for donor siblings mainly derive from the survival of the recipient 7 sibling rather than from process of tissue harvest per se. 8 9 Balance of benefits and risks 10 Whereas the advantages of tissue harvest for donor siblings are long-term and merely 11 psychosocial, the other side of balance sheet consists of short-term psychological 12 burden and life-threatening physical harm. One should bear in mind that the notion of 13 benefits and risks are both relative concepts. To consider the potential gains or losses 14 for donor siblings, we ought to consider what would likely happen to the donors and 15 recipients without tissue harvest. It cannot be said that tissue harvest can offer any 16 significant long-term benefits for the donor sibling if other available source of 17 transplant can offer a similar chance of success or if the sick sibling can survive 18 without serious complications even without transplantation. Those who do not agree 19 may argue that a donor sibling may in the future relish and take pride in being a donor 20 and therefore still want to donate even if other donors are available. Parents may 21 legitimately consider this factor when making decisions for incompetent minors. But 22 the remoteness of this benefit should take its edge off from the evaluation. The sense 23 of pride may not materialize if the grown-up donor sibling does not accept the filial or 24 social responsibility to save the recipient sibling, is disinterested in altruistic donation, 25 or does not relish in living in the shadows of the recipient sibling. In any event, it is 7 1 only for a competent individual to decide whether they want to take the risks in 2 exchange for just the goodwill and the pride of being ‘a donor and a saviour’. For 3 minors, we hold that the benefits of this alone are too remote and small in magnitude 4 to justify the medical risks of life-threatening bodily intrusion. In short, the only 5 circumstance where tissue harvest would serve the best interests of a minor donor is 6 that without the proposed transplantation taking place, the sick sibling will more 7 likely suffer serious complications or die. 8 9 Availability of other donors 10 In light of foregoing discussion, to determine whether tissue harvest is in a donor 11 sibling’s best interests, one should assess first whether the recipient sibling would 12 likely die or suffer from serious complications without a transplantation. If the answer 13 is affirmative, then one should see if donation from any mentally competent donors 14 can offer a similar chance of successful transplantation. 15 16 In the past, tissue-matched related donors were considered to be the best sources of 17 donation. But now, many drawbacks of unrelated or haplo-identical transplants such 18 as graft failure and significant graft-versus-host diseases have been overcome due to 19 the development of new extensive T-cell depletion techniques with mega dose stem 20 cell administration over the last two decades. New approaches such as alloreactive T 21 cell depletion and post-transplant cell therapy have also improved immune 22 reconstitution in tissue-matched unrelated or haplo-identical transplants. Using haplo- 23 identical donors are now considered to be equally safe and effective transplant 24 strategies as tissue-matched donors for advanced leukemia.18 Leung and others 25 showed that the five year survival rates of recipient siblings with high risk leukemia 8 1 are promising regardless of donor types (68% for donor siblings, 74% for unrelated 2 donors and 77% for haplo-identical donors), and that the risks of death from graft- 3 versus-host diseases at five years is not significantly associated with the types of 4 donors (6.6% for donor siblings, 7.0% for unrelated donors, and 3.4% for haplo- 5 identical donors).19 Therefore, a search for competent family members, local and even 6 international bone marrow donor registry should be undertaken before parents are 7 permitted to consent to tissue harvest from donor siblings for recipients suffering 8 from advanced lymphoma or leukemia. For other diseases, Sodani and others reported 9 that haplo-identical transplant in thalassemia has 93% chance of survival and only 7% 10 mortality using new conditioning regimen.20 Bolaños-Meade and others showed that 11 the use of haplo-identical transplant for patients with sickle cell disease is highly 12 effective and safe despite the fact that graft failure still remains an obstacle.21 13 14 Proposed amendments of the Policy 15 It is already well established that the use of haplo-identical transplant is equally safe 16 and effective for advanced lymphoma or leukemia, whereas studies are still underway 17 to evaluate the results with non-malignant diseases like aplastic anemia, lupus and 18 sickle cell diseases. The above literature search by no means suggests that haplo- 19 identical transplant can replace tissue-matched transplant but, given the success of 20 new regimens of transplantation, doctors should look beyond the availability of 21 tissue-matched related donors for certain types of diseases. Parents and doctors should 22 make sure, if the medical conditions of the sick sibling permit a search, that no other 23 sources of equally or similarly effective transplant are available before subjecting a 24 minor to the physical risks and short-term psychological harm of tissue harvest. 25 9 1 In the circumstances, I propose that the following should replace the original first and 2 third criteria in the Policy: 3 4 1. If the medical conditions of the recipient permit a search, there is no medically 5 equivalent haplo-identical/histo-compatible adult who is willing and able to 6 donate; 7 8 9 3. The recipient sibling will likely suffer from serious complications or die without transplantation before the donor sibling becomes Gillick competent, 10 11 CONCLUSIONS 12 The parental choice to harvest tissues from donor siblings reflects the immense 13 ‘emotive desire to do something to help the recipient sibling’.22 However, donor 14 siblings may not necessarily reap any benefits in light of the risks of serious injuries 15 arising from bone marrow or peripheral blood transplantation. Fulfilling the criteria 16 specified in the Policy of the Academy alone is not sufficient to justify tissue harvest 17 from minors. Unless a recipient sibling will likely suffer from serious complications 18 or die without the transplantation and no tissue-matched unrelated donors or related 19 haploidentical donors are available, there is no moral or legal basis to violate the 20 donor sibling’s right to bodily integrity. In short, the Policy should be revised to fully 21 address our moral concerns in relation to tissue harvest from minor donor siblings. 22 23 24 Competing interests 10 1 The authors declare that they have no competing interests. 2 Author’s Contributions 3 Corresponding and first author Chan TK is the main researcher, writer and editor 4 responsible for the legal research and ethical analysis. 5 6 The co-author Tipoe GL, was responsible for identifying ethical issues, overseeing the 7 research and giving expert input into the ethical analysis and review. Both authors 8 read and approved the final manuscript. 9 10 Authors’ Information 11 CHAN TK, MBChB, MRCS, LLM(Medical Law and Ethics) 12 Assistant Professor 13 Anatomy 14 University of Hong Kong 15 L1-59 Laboratory Block, Faculty of Medicine Building, 21 Sassoon Road, Hong 16 Kong 17 18 19 TIPOE GL, MD, PhD 20 Asscoiate Professor 21 Anatomy 22 University of Hong Kong 23 24 1/F Laboratory Block, Faculty of Medicine Building, 21 Sassoon Road, Hong Kong 25 26 Acknowledgements 27 We would like to thank the reviewers Dr Wendy Rogers, Dr Joerg Halter, Dr Elaine 28 Morgan and Dr Heidi Mertes for their invaluable comment in revision of the 29 manuscript. 11 1 2 Funding 3 Funding not required 4 5 Ethical Approval 6 Ethical approval not required. 7 8 References 9 . American Academy of Pediatrics: Policy Statement—Children as Hematopoietic 10 Stem Cell Donors. Pediatrics 2010, 125:392-404. 11 2. Mill JS: On Liberty. Penguin Edition: 1974. 12 13 3. Gillick v West Norfolk and Wisbech Area Health Authority [1985] 3 All ER AC 14 112. 15 16 4. Section 1, Children Act 1989 17 [http://www.legislation.gov.uk/ukpga/1989/41/section/1] 18 19 5. Re C & F (Children) 2003 EWHC 1376 (Fam). 20 21 6. Birmingham City Council v H (a minor) [1993] 1 FLR 883. 22 23 7. Re Z (a minor) (freedom of publication) [1995] 4 All ER 961 at 986, [1997] Fam 1 24 at 32. 12 1 2 8. Bojanić I, Cepulić BG, Mazić S: Collection of hematopoietic progenitor cells 3 from healthy donors. Acta Med Croatica 2009, 63(3):237-44. 4 5 9. Pulsipher MA, Levine JE, Hayashi RJ, Chan KW, Anderson P, Duerst R, Osunkwo 6 I, Fisher V, Horn B, Grupp SA: Safety and efficacy of allogeneic PBSC collection 7 in normal pediatric donors: the pediatric blood and marrow transplant 8 consortium experience (PBMTC) 1996 –2003. Bone Marrow Transplant 2005, 9 35(4):361–367. 10 11 10. Curran v. Bosze (1990) 566 N.E. 2d 1319 12 13 11. Wass H: Helping children cope with death. In Papadatou D, Papadatou C: 14 Children and Death. New York: Hemisphere;1991:11-32. 15 16 12. MacLeod KD, Whitsett S, Mash EJ, Pelletier W: Pediatric Sibling Donors of 17 Successful and Unsuccessful Hematopoietic Stem Cell Transplants (HSCT): A 18 Qualitative Study of Their Psychosocial Experience. J Pediatr Psychol 2003, 19 28(4):223-230. 20 21 13. Packman WL, Crittenden MR, Schaeffer E, Bongar B, Fischer JB, Cowan MJ: 22 Psychosocial consequences of bone marrow transplantation in donor and 23 nondonor siblings. Journal of Developmental & Behavioral Pediatrics 1997, 18:244- 24 253. 25 13 1 14. Heffernan S, Zanelli A: Behavior changes exhibited by siblings of pediatric 2 oncology patients: A comparison between maternal and sibling descriptions. 3 Journal of Pediatric Oncology Nursing 1997, 14:3–14. 4 5 15. Barbarin OA, Sargent JR, Sahler OJ, Carpenter PJ, Copeland DR, Dolgin MJ: 6 Sibling Adaptation to Childhood Cancer Collaborative Study: Parental views of 7 pre- and post diagnosis adjustment of siblings of children with cancer. Journal of 8 Psychosocial Oncology 1995, 13:1–20. 9 16. Chesler MA, Allswede J, Barbarin OO: Voices from the margin of the family: 10 Siblings of Children with Cancer. Journal of Psychosocial Oncology 1991, 9:19– 11 42. 12 17. Wiener LS, Steffen-Smith E, Battles HB, Wayne A, Love CP, Fry T: Sibling 13 stem cell donor experiences at a single institution. Psychooncology 2008, 14 17(3):304-7. 15 16 18. Tischer J, Stemmler HJ, Engel N, Hubmann M, Fritsch S, Prevalsek D, Schulz C, 17 Zoellner AK, Bücklein V, Hill W, Ledderose G, Hausmann A: Feasibility of 18 clofarabine cytoreduction followed by haploidentical hematopoietic stem cell 19 transplantation in patients with relapsed or refractory advanced acute leukemia. 20 Ann Hematol 2013, doi 10.1007/s00277-013-1862-6. 21 22 19. Leung W, Campana D, Yang J, Pei D, Coustan-Smith E, Gan K, Rubnitz JE, 23 Sandlund JT, Ribeiro RC, Srinivasan A, Hartford C, Triplett BM, Dallas M, Pillai A, 24 Handgretinger R, Laver JH, Pui CH: High success rate of hematopoietic cell 14 1 transplantation regardless of donor source in children with very high-risk 2 leukemia. Blood 2011, 118(2):223–230. 3 4 20. Sodani P, Isgro A, Gaziev J, Paciaroni K, Marziali M, Simone MD, Roveda A, De 5 Angelis G, Gallucci C, Torelli F, Isacchi G, Zinno F, Landi F, Adorno G, Lanti A, 6 Testi M, Andreani M, Lucarelli G: T cell-depleted HLA-haploidentical stem cell 7 transplantation in thalassemia young patients. Paediat Rep 2011, 3(s2):e13. 8 9 21. Bolaños-Meade J, Fuchs EJ, Luznik L, Lanzkron SM, Gamper CJ, Jones RJ, 10 Brodsky RA: HLA-haploidentical bone marrow transplantation with post- 11 transplant cyclophosphamide expands the donor pool for patients with sickle cell 12 disease. Blood 2012 Sep 6 doi:10.1182/blood-2012-07-438408. 13 14 22. Lyons B: The good that is interred in their bones: are there property rights in 15 the child? Medical Law Review 2011, 19(3):372–400. 15