Infection Prevention Assessment Tool
advertisement

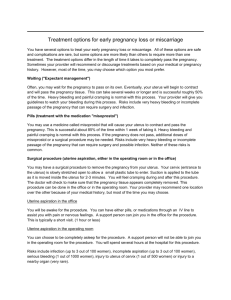
AREA: PREGNANCY COMPLICATION MANAGEMENT (HYPOVOLEMIC SHOCK, SEVERE PRE-ECLAMPSIA/ECLAMPSIA, ABDOMINAL PAIN) FACILITY: ________________________________________________________________________________________________________________ ASSESSOR: ____________________________________________________________ DATE: PERFORMANCE STANDARDS __________________________________________ VERIFICATION CRITERIA Y, N COMMENTS Hypovolemic shock Instructions to the assessor: Interview a provider who is likely to manage a client with hypovolemic shock. 1. The provider can describe signs of shock. Ask the provider: “What are the signs of shock?” Pulse weak and equal to or greater than 110 Systolic BP less than 90mm Hg Rapid breathing (30 breaths per minute or above) Pale, skin feels cold and clammy (cold perspiration) Confusion or unconsciousness 2. The provider can describe the steps of rapid initial assessment of a woman with hypovolemic shock. Ask the provider: “How do you conduct a rapid initial assessment and management of a woman in hypovolemic shock?” Request assistance and immediately mobilize all available personnel Quickly shift the woman to an examining table Rapidly evaluate vital signs o Pulse o Blood pressure o Breathing Place the woman on her side to prevent aspiration Cover the woman with a blanket Raise the foot-end of the bed or elevate legs EOC Standards—March 2009 _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ Pregnancy Complications – 18 PERFORMANCE STANDARDS 3. The provider describes the management of shock. 4. The provider can describe the steps to identify the specific causes of shock. EOC Standards—March 2009 VERIFICATION CRITERIA Ask the provider to describe how to manage shock: Ensure client’s head is down and the foot-end of the bed is raised Place the client on her side to prevent aspiration Administer oxygen by mask at 6–8L/minute Extract blood for haemoglobin, coagulation, blood group and Rh (cross-matching) tests Request blood from donor Start two IV lines using a 16- or 18-gauge cannula Label IV bags with medications added, if any Replace fluids with: o Saline or Ringer’s solution o 1L over a 15–20 minute period (wide open rate) o Give 2 additional litres during the first hour over and above fluid replacement for continuing blood loss Continue to replace volume IV in accordance with the loss of blood (two or three times the estimated loss) Assess woman’s need for transfusion based upon signs and symptoms of shock or impending shock due to amount of blood lost Catheterize bladder and take baseline urine output Keep the patient warm Ask the provider: “How do you identify the causes of shock?” Take history (from patient or accompanying person) Perform an abdominal and pelvic examination as needed Assess findings to list possible causes of bleeding Y, N COMMENTS _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ _________ Pregnancy Complications – 19 PERFORMANCE STANDARDS 5. The provider can describe monitoring and evaluation of patient's response to the intervention and plan for the next step. 6. The provider records on the clinical history the information related to findings and procedures performed. EOC Standards—March 2009 VERIFICATION CRITERIA Ask the provider: How do you evaluate the women’s response to the immediate treatment? o Monitor every 15 minutes: Pulse BP Mental state (confusion) Urine output What would you do if the vital signs stabilize (pulse 90 or less, systolic BP 100mmHg or more, at least 30ml of urine per hour and less anxiety/confusion)? o Continue management of underlying cause of bleeding o Adjust IV infusion to 1L over a 6-hour period (60 drops/minute) o Continue to monitor vital signs What would you do if the conditions do not improve? o Continue IV solution 1L over a 6-hour period (60 drops/minute) o Continue to administer oxygen 6–8L/minute o Continue monitoring Observe whether the provider records: Admission condition Cause of shock Solutions, fluids, and drugs given (doses, time) Procedures performed Progress Y, N COMMENTS ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ _________ _________ _________ _________ _________ Pregnancy Complications – 20 PERFORMANCE STANDARDS 7. The provider shows the equipment and drugs to be used for management of shock. VERIFICATION CRITERIA Ask the provider to show the interviewer the following: Supplies for starting an IV line: o 16- or 18-gauge needle or cannula o IV equipment o Saline or Ringer’s lactate solution Equipment and supplies for administering oxygen: o Functioning oxygen cylinder and regulator o Nasal piece or oro-nasal mask Supplies for bladder catheterization: o Foley catheter o Urine collection bag Supplies for blood extraction o 10cc syringe and gauge 21 needle o Citrated and non-citrated test tube Y, N COMMENTS _________ _________ _________ _________ _________ _________ _________ _________ _________ Bleeding in Early Pregnancy Instructions to the assessor: Interview a provider that usually works in the emergency room or in the maternity ward and that is likely to manage an incomplete abortion. 8. The provider can list the different conditions causing early bleeding in pregnancy. EOC Standards—March 2009 Ask the provider to list conditions that cause early bleeding in pregnancy: Ectopic pregnancy Abortion or miscarriage Molar pregnancy ___________ ___________ ___________ Pregnancy Complications – 21 PERFORMANCE STANDARDS 9. The provider can describe the initial management of bleeding in early pregnancy. EOC Standards—March 2009 VERIFICATION CRITERIA Ask the provider: “What is the initial management of bleeding in early pregnancy?” Rapid evaluation of condition: o Check vital signs o Assess for hypovolemic shock o If in shock, manage accordingly (see above) Collect information to make presumptive diagnosis: o History o Abdominal examination o Pelvic examination Manage according to diagnosis: o Ectopic pregnancy o Threatened abortion o Incomplete abortion o Completed abortion o Molar pregnancy Y, N COMMENTS ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ Pregnancy Complications – 22 PERFORMANCE STANDARDS 10. The provider describes the sign and symptoms of abortion. EOC Standards—March 2009 VERIFICATION CRITERIA Ask the provider: “What are the sign and symptoms of abortion?” Threatened abortion: o Light bleeding o Closed cervix o Uterus corresponds to dates Inevitable abortion: o Heavy bleeding o Dilated cervix o Uterus corresponds to dates Incomplete abortion: o Heavy bleeding o Dilated cervix o Uterus is smaller than dates Complete abortion: o Light bleeding o Closed cervix o Uterus is smaller than dates and softer than normal Molar pregnancy: o Heavy bleeding o Dilated cervix o Uterus larger than dates o Uterus softer than normal o Partial expulsion of product of conception resembling grapes Y, N COMMENTS _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ Pregnancy Complications – 23 PERFORMANCE STANDARDS 11. The provider describes the management of abortions. EOC Standards—March 2009 VERIFICATION CRITERIA Ask the provider: “What is the correct management of abortions?” Threatened abortion: o Medical treatment is usually not necessary o Avoid strenuous activity and intercourse but bed-rest is not necessary o If bleeding persists assess for fetal viability (PT or US) or ectopic pregnancy. Persistent bleeding, particularly in the presence of a uterus larger than expected, may indicate twins or molar pregnancy Inevitable abortion: o If pregnancy is less than 16 weeks, plan for evacuation of uterine contents If immediate evacuation is not possible, give ergometrine 0.2mg IM and repeat after 15 min if necessary; or misoprostol 400 mcg by mouth (repeat once after 4 hours, if necessary) o If pregnancy is greater than 16 weeks, await spontaneous expulsion of POC and then evacuate the uterus to remove any remaining POC o If necessary, infuse oxytocin 40 units in 1L IV fluid (normal saline or Ringers lactate) at 40 drops per minute to help achieve expulsion of POC o Ensure follow-up of the woman after treatment Incomplete abortion: o If bleeding is mild to moderate and pregnancy is less than 16 weeks, use finger or sponge forceps to remove the POC o If bleeding is heavy and pregnancy is less than 16 weeks evacuate the uterus (MVA is preferred method) o If pregnancy is greater than 16 weeks infuse oxytocin 40 units in 1L IV fluids at the rate of 40 drops /min until the expulsion of POC o If necessary give misoprostol 200 mcg vaginally every 4 hours until expulsion and evacuate any remaining POC from the uterus Complete abortion: o Observe for heavy bleeding and ensure follow-up of woman Y, N COMMENTS _________________ _________________ _________________ _________________ _________________ _________________ ___________ _________________ _________________ _________________ _________________ _________________ _________________ Pregnancy Complications – 24 PERFORMANCE STANDARDS VERIFICATION CRITERIA 12. The provider can describe sign and symptoms of ectopic pregnancy. Molar Pregnancy o If diagnosis of molar pregnancy is certain, evacuate the uterus o Use vacuum aspiration o Infuse oxytocin 20 units in 1L IV fluids at 60 drops/min to prevent haemorrhage o Recommend hormonal FP method for at least one year o Follow-up every 8 weeks for at least one year with urine pregnancy tests: If urine pregnancy test is not negative after 8 weeks or becomes positive again, refer to a tertiary facility for follow-up Ask the provider: “What are the signs and symptoms of ectopic pregnancy?” History of amenorrhea Slight vaginal bleeding Abdominal pain Fainting Closed cervix Uterus slightly larger than normal 13. The provider can describe the management of ectopic pregnancy. Ask the provider: “What is the correct management of ectopic pregnancy?” Cross-match blood and prepare and perform laparotomy 14. The provider can describe post-abortion care steps. Ask the provider, “What would be the post-abortion steps to take before a woman is discharged?” Tell the woman that her fertility will return as early as 2 weeks after the event Provide counselling on healthy timing and spacing of pregnancy Assist her to choose a contraceptive method Provide method of choice before discharge EOC Standards—March 2009 Y, N COMMENTS _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ Pregnancy Complications – 25 PERFORMANCE STANDARDS VERIFICATION CRITERIA Y, N COMMENTS Preeclampsia and eclampsia 15. The provider can correctly describe the signs and symptoms of severe pre-eclampsia and eclampsia. 16. The provider can describe the correct management of severe pre-eclampsia and/or eclampsia. Ask the provider: “What are the signs and symptoms of severe pre-eclampsia and eclampsia?” Severe pre-eclampsia: o Diastolic BP 110mmHg or more o 20 weeks or more of gestation o Proteinuria 3+ Eclampsia: o Convulsions o Diastolic BP 90mmHg or more o 20 weeks or more of gestation o Proteinuria 2+ or more Ask the provider: “What is the correct management of severe preeclampsia/eclampsia?” Take vital signs including FHS every 15 minutes Insert catheter to start measuring urine output Give magnesium sulfate: Loading dose: o Administer 4g of 20% solution of magnesium sulphate in IV solution (20ml) slowly over a 5-minute period o Administer 5g of 50% magnesium sulphate solution (20ml), with 1ml of 2% lidocaine IM deep in each buttock (total 10g) o If convulsions reoccur after 15 min, give 2g 50% magnesium sulphate ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ slowly in IV over 5 min. EOC Standards—March 2009 Pregnancy Complications – 26 PERFORMANCE STANDARDS VERIFICATION CRITERIA Maintenance Dose o Administer 5g of 50% magnesium sulphate solution (20ml), with 1ml of 2% lidocaine IM deep every 4 hours into alternate buttocks o Continue treatment with magnesium sulphate for 24 hours after delivery or the last convulsion, whichever occurs last. Start IV line with saline or Ringer’s lactate solution Give antihypertensive to maintain diastolic pressure at 90-100mm Hg: o Plan 1: Hydralazine 5mg IV slowly every 5 min or 12.5mg IM every 2 hours, until diastolic BP stabilizes between 90 and 100mmHg, or o Plan 2: Nifedipine 5mg orally, repeating the dose if the diastolic BP is still more than 110 after 10 min Deliver within 24 hours of onset of severe pre-eclampsia and within 12 hours for eclampsia Monitor vital signs, FHS, reflexes and urine output Management of eclampsia o Give anticonvulsive – as above o Give antihypertensive-as above o Passively restrain for protection o Place on left side to minimize aspiration o Aspirate mouth and throat as needed post convulsion o Gather equipment (airway, suction, mask and bag, oxygen) o Deliver within 12 hours of start of convulsion Withhold or delay drug if: Respiratory rate falls below 16/min Patellar reflexes are absent Urinary output falls below 30ml per hour over preceding 4 hours Keep antidote ready: Assist ventilation (mask and bag, anaesthesia apparatus, intubation), and give oxygen at 4-6L per minute. Give calcium gluconate 1g (10mL of 10 % solution), in IV slowly until respiration begins to antagonize the effects of magnesium sulphate EOC Standards—March 2009 Y, N COMMENTS ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ ___________ Pregnancy Complications – 27 PERFORMANCE STANDARDS VERIFICATION CRITERIA Y, N COMMENTS Abdominal Pain in Early Pregnancy Instructions to the assessor: Interview a provider who usually works in the emergency room or in the maternity ward who is likely to manage abdominal pain in early pregnancy 17. The provider can list the different conditions causing pain in early pregnancy. 18. The provider can describe the initial management of abdominal pain in early pregnancy. EOC Standards—March 2009 Ask the provider to list conditions that cause pain in early pregnancy: Ovarian cyst – torsion Appendicitis Cystitis Acute pyelonephritis Peritonitis Ectopic pregnancy Abortion Ask the provider: “How do you initially manage abdominal pain in early pregnancy?” Rapid evaluation of condition: o Check vital signs o Assess for hypovolemic shock o If in shock, manage accordingly (see above) Collect information to make presumptive diagnosis: o History o Abdominal o Pelvic examination Manage according to diagnosis: o Ovarian cyst – torsion o Appendicitis o Cystitis o Acute pyelonephritis o Peritonitis o Ectopic pregnancy o Abortion _________________ _________________ _________________ _________________ _________________ _________________ _________________ _________________ ___________ ___________ _________________ ___________ ___________ _________________ ___________ ___________ ___________ ___________ ___________ ___________ Pregnancy Complications – 28 Total of standards 18 Total observed Total achieved EOC Standards—March 2009 Pregnancy Complications – 29