HOW DO I CHOOSE A FLUID
advertisement
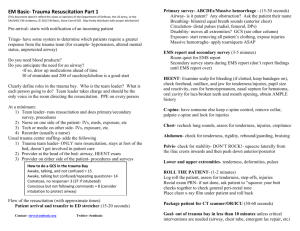
FLUID RESUSCITATION OF THE TRAUMA PATIENT Steven L. Marks, BVSc, MS, MRCVS, DACVIM Small Animal Track 2012 ISVMA Annual Conference Proceedings INTRODUCTION Fluid therapy is one of the cornerstones of medical management in the emergency room. In the trauma patient, fluid therapy for volume resuscitation is an integral part of the initial management. Blunt or penetrating trauma is a common reason for the small animal patients to be presented to the emergency room. These cases must be triaged and rapidly and efficiently evaluated in order to construct a successful diagnostic and therapeutic plan. The most common volume related syndrome in the trauma patient is hypovolemic shock. PATIENT EVALUATON Triage Triage is defined as a process of determining the priority of need and proper order of treatment when evaluating a clinical situation. In practical terms this means to be able to prioritize which cases should be treated first and within each case which problems and which systems should be evaluated first. In other words the clinician must follow a systematic approach when evaluating the trauma patient. Initial Assessment Following the A, B, C’s is a quick and effective way of initially assessing the trauma patient. Airway Breathing Circulation When evaluating the circulatory system in the trauma patient, it is a priority to look for signs of shock. The cardinal signs of shock are mucous membrane pallor, tachycardia, weak peripheral pulses, hypothermia and depressed mentation. Assessment of volume status and requirements are relegated to the circulatory system in this triage format. LOW VOLUME VERSUS HIGH VOLUME RESUSCITATION The traditional protocol for volume resuscitation is to provide rapid volume expansion with isotonic replacement crystalloid solutions. The ideal solutions are .9% saline or LRS. The volumes that have been suggested are 90 ml/kg/hr for the dog and 45-60 ml/kg/hr for the cat. These volumes are based on either blood or plasma volumes respectively. One easy way to administer a shock volume of fluid is to divide the doses into increments. A very quick rule of thumb for the dog is to add a 0 to the body weight in pounds and this is approximately ¼ of a shock dose. Example: 40 pound dog = 400 ml (1/4 shock volume). This volume is administered over approximately 15 minutes and the patient is reassessed. If required the total volume of 1600 ml can be infused. If you compare this to the 90 ml/kg/hr volume (total of 1800 ml), it is very close. In the feline patient, a very similar rule can be applied. If you add a 0 to the body weight in kilograms, this is approximately ¼ of a shock dose. Example: 10 pound cat = ~ 5 kg cat = 50 ml (1/4 shock volume). This volume is administered over approximately 15 minutes and the patient reassessed. If required the total volume of 200 ml can be infused. The volume to be infused by the formula of 45 ml/kg x 5 kg = 225 ml, which compares favorably with the 200 ml calculated with the quick rule. Although this type of fluid resuscitation has been the standard of care in veterinary medicine, more recently there has been some incentive to utilize low volume resuscitation in some veterinary trauma patients. This is particularly true if there is recent or uncontrolled hemorrhage. The concerns of high volume resuscitation stem from the recognition of resuscitation injury. This may come in the form of worsening of clinical bleeding, disruption of preformed clots and interstitial edema. In addition to hemorrhage, head trauma and pulmonary trauma may also be situations where judicious use of volume resuscitation is indicated. In these situations the goal has become to restore circulating volume with the minimal amount of fluid possible and to avoid overhydration. There has been some work performed looking at resuscitation end points such as mean arterial pressure (MAP) or systolic arterial pressure. Although there is some debate it seems reasonable to resuscitate to a MAP of 60 mmHg or 80 mmHg systolic blood pressure in order to maintain organ perfusion. If indirect or direct blood pressure monitoring is unavailable, femoral pulses typically cannot be palpated if the MAP is less than 60 mmHg and this can be used as a guide. FLUID SELECTION It appears that fluid selection has little to do with outcome in most studies that have compared fluid types. There are numerous publications comparing crystalloids and colloids and determining outcome. Overall it is difficult to show differences in survival when these solutions are compared for volume resuscitation. In many cases the choice is left to clinician discretion based on knowledge and experience. It is however still important to try to select a fluid that closely matches the patient’s requirements in this emergency situation. The replacement crystalloid solutions that are most commonly used for volume resuscitation are .9% saline and LRS. These solutions are primarily chosen based on the content of sodium and chloride and the ability for rapid volume expansion. Based on these selection criteria, other replacement solutions such as Normosol-R and Plasmalyte may also be appropriate choices. The major disadvantage of these solutions is their short-lived effect on the intravascular space as less than 25% remains in the intravascular compartment 1 hour following infusion. Colloid solutions that are often chosen for resuscitation of the trauma patient and the most commonly used is iHetastarch. These solutions are administered due to the high molecular weight of the particles found in solution. This property allows these solutions to have a prolonged effect on the intravascular volume. The major disadvantages of these solutions include cost and the possibility of induced coagulation problems. These synthetic colloids are typically administered as a 5 ml/kg bolus to effect or may be administered as a 24 hour CRI at a dosage of 20 ml/kg. They can be used as single agents or in combination with isotonic replacement crystalloid solutions or hypertonic saline. A newer colloid Voluven has recently gained favor due to its increased total daily volume (50 ml/kg/day) and its lack of contribution to coagulopathy. Oxyglobin, a hemoglobin based oxygen carrier is a unique colloid as it combines oncotic properties with the ability to provide oxygen carrying capacity. Oxyglobin can be administered at a dosage of 10-30 ml/kg and may be given to effect in the dog. When Oxyglobin is administered in the cat it is given with caution and at much lower dosages 2.5-5 ml/kg. Hypertonic saline (7-7.5%) is a hypertonic crystalloid which has the ability to rapidly increase the intravascular volume with considerably less volume administration than isotonic crystalloids. The dosage used for dogs is 4-7 ml/kg IV and in cats 2-4 ml/kg. Again this effect on the intravascular space is short lived but can be prolonged by adding a colloid solution such as Hetastarch to the infusion. A useful cocktail is to combine 43 ml of Hetastarch and 17 ml of 23.4% hypertonic saline (stock solution) in a syringe and administer this solution at a volume of 3-5 ml/kg IV. Transfusion products can be very useful in the trauma patient. Due to the availability of synthetic colloids, it is uncommon to use plasma product in the acute trauma patient. If the patient has significant hemorrhage and requires oxygen carrying capacity, red cell products may be indicated. In this situation the options would be fresh whole blood or packed red blood cells (pRBC). Whole blood can be administered at a dosage of 20 ml/kg to raise the patient PCV approximately 10%. pRBC transfusions may be administered at a dosage of 10-15 ml/kg in order to attain the same response. RESUSCITATION POINTS The traditional endpoints of fluid resuscitation have been CRT, heart rate, blood pressure, central venous pressure and urine output. It now appears that other end points such as lactate concentrations may also be useful. If we believe lactate is a marker for hypoxia and decreased perfusion, this may be an ideal endpoint for successful resuscitation. There is continued debate on what is the best technique to resuscitate the trauma patient. At the current time evidence based information is still lacking as to what volumes and what fluid choices will have the most significant impact on survival. REFERENCES B Driessen et al. J Vet Emerg Crit Care 2006;16:276. K Humm et al. JVIM 2007;21:656. KA Mathews. Vet Clin North Amer Small Anim Pract 1998;28:483. J Prittie. J Vet Emerg Crit Care 2006;16:329. D Silverstein et al. J Vet Emerg Crit Care 2005;15:185. Stern SA et al. Shock 2000;14:616. JL Vincent et al. Crit Care Med 2006;34:1333.