Evaluation of colonoscopy performance in daily practice in a
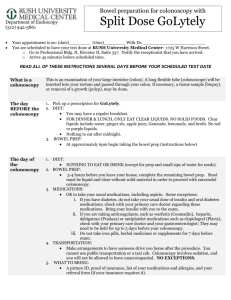
advertisement

Evaluation of colonoscopy performance in daily practice in a multicenter study Authors: de Jonge, Vincent1; Sint Nicolaas, Jerome1; van Baalen, Onno2; ter Borg, Frank3; Brouwer, Johannes T.4; Geldof, Han5; Hadithi, Muhammed6; Van Tilburg, Antonie J.P.7; Kuipers, Ernst J.1; van Leerdam, Monique E.1 Affiliations: Departments of Gastroenterology and Hepatology of 1Erasmus MC University Medical Center , Rotterdam, Netherlands; 2Beatrix Hospital, Gorinchem, Netherlands; 3Deventer Hospital, Deventer, Netherlands; 4Reinier de Graaf Hospital Group, Delft, Netherlands; 5IJsselland Hospital, Capelle aan de IJssel, Netherlands; 6Maasstad Hospital, Rotterdam, Netherlands; 7Sint Franciscus Gasthuis, Rotterdam, Netherlands. Introduction Colonoscopy demand rises among others because of the introduction of colorectal cancer screening. Various studies have reported large differences in the quality of colonoscopy. International assessment of this issue is of importance to allow optimal patient benefits, improvement of training and international comparison of data. Therefore we aimed to evaluate the performance of colonoscopy procedures in daily clinical practice. Methods Consecutive colonoscopy reports from 7 endoscopy units (1 academic, 6 general hospitals, 200 reports per site) were retrospectively reviewed from March to April 2009. Data captured included patient characteristics, indication, sedation and outcomes. Results 1,442 procedures were included (1,425 patients, 46% males, mean age: 58 yrs, ±16) from 55 endoscopists (mean: 25 procedures, ±17). Gastroenterologists referred 39% of patients, general practitioners 28%, internists 16% and others 17%. The most frequent indications were lower abdominal symptoms (28%), rectal blood loss (15%) and CRC surveillance (12%). Bowel preparation was not optimal in 30% of procedures. No association was found between inadequate bowel preparation and gender and age in multivariate regression. In 94% of procedures conscious sedation was applied by means of midazolam in 28%, fentanyl in 1% and the combination in 68%. Unadjusted cecal intubation rate was 90%. Most frequent reasons for failure of cecal intubation were looping and anatomic variations of the colon (21%), stenosis (19%), poor bowel preparation (19%) and pain (17%). Multivariate logistic regression showed that failure of cecal intubation was associated with insufficient bowel preparation (OR: 3.23, 95%CI: 2.04-5.10) and age ≥60 yrs (OR: 1.84, 95%CI: 1.152.96). Neoplasia was detected in 23% of patients including tubular adenomas in 55%, tubulovillous adenomas in 21%, villous adenomas in 4% and carcinoma in 20%. Advanced adenomas were found in 13% of all patients and 3% had ≥3 adenomas. Multivariate logistic regression showed that male gender (OR: 1.73, 95%CI: 1.25-2.37), bowel complaints (OR: 1.53, 95%CI: 1.11-2.12) and age ≥60 yrs (OR: 3.93, 95%CI: 2.80-5.52) were associated with the presence of neoplasia. One perforation was reported (0.07%) and 15 patients had minor bleeding after polypectomy (1%). Conclusion The technical quality of colonoscopy in daily practice in the Netherlands does reach the international standards, i.e. >90% cecal intubation, >20% adenoma detection and <0.1% perforation. However, improvement can be achieved among others with respect to bowel preparation. The quality indicators are helpful to assess quality of colonoscopy in daily clinical practice.