Indications for Symptomatic Patients & Surveillance of Groups at
advertisement
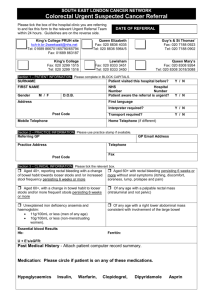
Indications for Symptomatic Patients & Surveillance of Groups at Increased Risk Southern District Health Board (District) Acute Indications and Priorities for Colonoscopy and CTC Continuous, > 4U of blood, normal gastroscopy Acute lower GI haemorrhage Emergency (If unstable consider CTA) Stable, requiring blood transfusion Next available list 2 week category A Suspected and severe IBD to establish diagnosis Known or suspected CRC (on imaging, or palpable, or visible on rectal examination for preoperative procedure to rule out synchronous pathology) Unexplained rectal bleeding with iron deficiency anaemia (benign anal causes treated – haemoglobin below local reference range) Altered bowel habit AND rectal bleeding (more frequent and/or looser stools; benign anal causes treated If > age 50 & > 6weeks duration or excluded) Altered bowel habit (more frequent and/or looser stools) Altered bowel habit AND rectal bleeding (more frequent and/or looser stools; benign anal causes treated If > age 50 & > 6weeks duration If age 40 - 50 & > 6weeks duration or excluded) Six week category B Unexplained rectal bleeding (benign anal causes treated) Iron deficient anaemia (haemoglobin below local reference range with low ferritin level) NZGG Cat. 2 plus one or more of altered bowel habit AND rectal bleeding looser stools; benign analhabit causesAND treated NZGG Cat. 3(more plusfrequent one orand/or more of altered bowel or excluded) rectal bleeding If > age 50 For woman < 55 menstruation history should be obtained coeliac disease and urinary loss to be excluded If age > 40 If age > 25 (more frequent and/or looser stools; benign anal causes treated Imaging or excluded)reveals polyp > 5mm Suspected and moderately severe IBD for diagnosis / mapping Acute diarrhoea (likely infectious aetiology and self limited) Rectal bleeding (normal Hb – consider FSA or flexible sigmoidoscopy if no anal cause) Not accepted Irritable bowel syndrome Constipation < 6 weeks duration < age 50 May require FSA (as a single symptom) Uncomplicated CT proven diverticulitis without suspicious radiological features Abdominal pain (without any “six week category” features) Decreased ferritin (normal Hb) < age 50 Abdominal mass Refer for appropriate imaging Comments Metastatic adenocarcinoma of unknown primary (6% due to CRC – in absence of radiological or tumour marker evidence colonoscopy is not indicated) The indication of iron deficiency anaemia requires a haemoglobin level below the local reference range in association with a low ferritin level. Menstruation is the commonest cause of iron deficiency anaemia in women. Coeliac disease and urinary loss should be excluded. Use of faecal occult blood tests collected in asymptomatic individuals is not currently recommended in New Zealand and should not be encouraged. CT colonography is an acceptable alternative investigation to colonoscopy for many indications in the ‘six week category’ where direct mucosal visualisation is not required. CT colonography may also be the most appropriate investigation for patients with significant co-morbidities but who meet the criteria for investigation. Southern DHB 71404 V1 Issued 21/01/2013 Page 2 of 4 Surveillance CRC Pre- or within 12 months post- operation 1st rescope Subsequent rescope 3 years 5 years Surveillance intervals apply after complete removal and polyp clearance Serrated adenomas should be treated as adenomatous polyps Polyps Low risk 1 or 2 adenomas <10mm 5 years Intermediate risk 3-4 adenomas <10mm 1 or 2 adenomas if one is ≥10mm Histological polyps with villous features Polyps with high grade dysplasia 3 years High risk ≥5 adenomas <10mm ≥3adenomas if one is ≥10mm Consider to stop 3 years then stop 3 years 1 year if low or intermediate risk 1 year If high risk Piecemal polypectomy Not part of NZGG recommendations 3 months* According to risk level * check of polypectomy site, only Offer baseline colonoscopy 8-10 years after diagnosis for UC and colonic Crohn’s colitis (CC) Risk similar for UC and Crohn’s colitis with same extent Low risk Extensive but quiescent UC / CC; or Left sided UC/ CC (but not proctitis) Extensive UC or CC with mild active inflammation confirmed histologically; or Post-inflammatory polyps; or FH CRC in 1st degree relative≥50 Intermediate risk IBD High risk Extensive UC or CC with moderate or severe active inflammation confirmed histologically; or PSC (including after LT); or Colonic stricture in the past 5 years; or Any degree of dysplasia* within last 5 years; or FH of CRC in 1st degree relative <50 5 years 5 years 3 years 3 years^ 1 year 1 year^ ^ High or intermediate risk patients: consider extending the interval to 5 years after two consecutive colonoscopies with low risk findings * Interpreting dysplasia and visualising DALMs/adenomas is more difficult when there is active inflammation Dysplasia should be confirmed by a second pathologist before commencing treatment 1st colo Family History Cat 1 Cat 2 One FDR > age 55 No recommendation made One FDR < age 55 Starting at age 50 or at an age 10 years younger than earliest cancer in the family Two FDR of any ageA family history of FAP, HNPCC or other familial cancer syndromes One FDR plus ≥ 2 FDR or SDR C same side of the family, Cat 3 Two FDR Or One FDR plus ≥ 1SDR same side of the family o o o C And one such relative had CRC < 55 Or developed multiple CRC’s Or developed extra colonic tumour - ?HNPCC (endometrial, ovarian, stomach, small bowel, upper renal tract, pancreas, brain) polyps Index A personal history CRC age Or40One FDR with < age colonoscopy around – if normal noCRC further o - a genetic specialist / family cancer clinic or registry for further assessment and possible genetic testing - to a bowel cancer specialist to plan appropriate surveillance ≥ one FDR or SDR CRC in association with multiple Acromegaly 50 surveillance 5 years Refer to: at any age Subsequent rescope C where tumour has shown loss of mismatch repair gene Southern DHB 71404 V1 Issued 21/01/2013 Page 3 of 4 Indications for CTC High risk patients AND High risk for colonoscopy On warfarin – high risk to stop Frail /old Change in bowel habit (more frequent/looser stools) Appropriate Moderate risk patients Iron deficiency non responsive / relapsing to treatment High risk symptoms of long-term duration Indications Diverticulitis with thickened bowel on CT scan Moderate risk symptoms but <age 60 / long-term Low risk patients Inappropriate Indications Abnormal appendicitis presentation > age 60 and unusual High risk patients Unless colonoscopy carries high risks Known / strongly suspected polyp / tumour Where polypectomy and / or biopsy may be required Inflammatory bowel disease Initial diagnosis / mapping OR surveillance Polyp surveillance First surveillance examination Southern DHB 71404 V1 Issued 21/01/2013 Page 4 of 4