Clinical Preparation Sheet Sample
advertisement
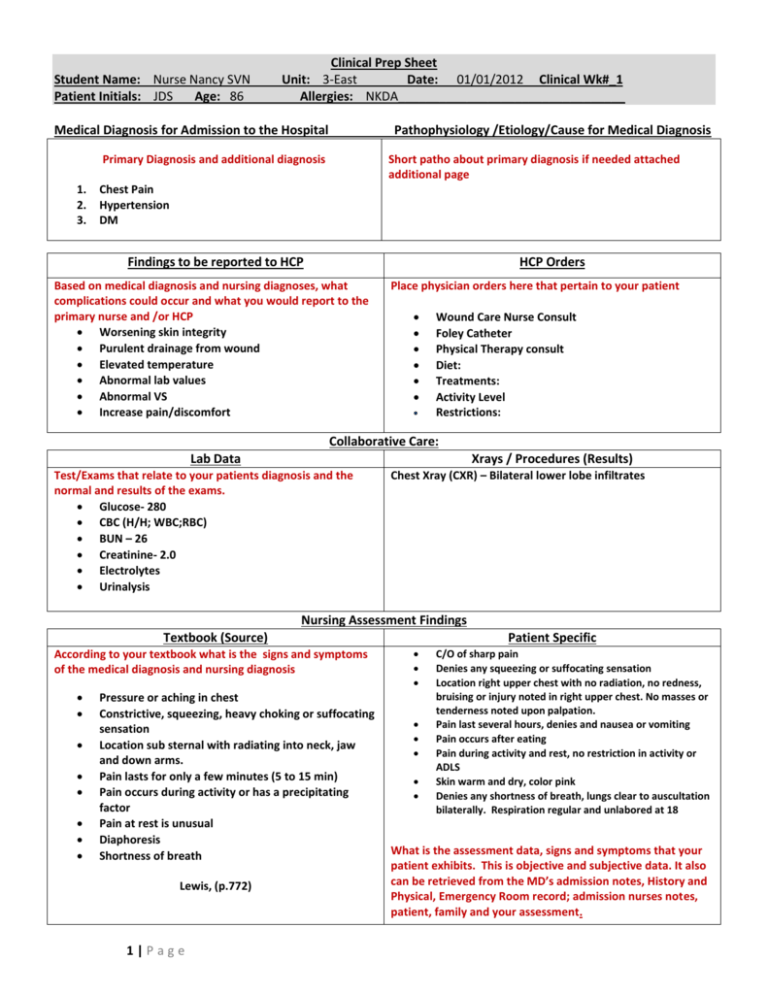
Student Name: Nurse Nancy SVN Patient Initials: JDS Age: 86 Clinical Prep Sheet Unit: 3-East Date: 01/01/2012 Clinical Wk#_1 Allergies: NKDA_________________________________ Medical Diagnosis for Admission to the Hospital Pathophysiology /Etiology/Cause for Medical Diagnosis Primary Diagnosis and additional diagnosis 1. 2. 3. Short patho about primary diagnosis if needed attached additional page Chest Pain Hypertension DM Findings to be reported to HCP HCP Orders Based on medical diagnosis and nursing diagnoses, what complications could occur and what you would report to the primary nurse and /or HCP Worsening skin integrity Purulent drainage from wound Elevated temperature Abnormal lab values Abnormal VS Increase pain/discomfort Place physician orders here that pertain to your patient Wound Care Nurse Consult Foley Catheter Physical Therapy consult Diet: Treatments: Activity Level Restrictions: Collaborative Care: Lab Data Xrays / Procedures (Results) Test/Exams that relate to your patients diagnosis and the normal and results of the exams. Glucose- 280 CBC (H/H; WBC;RBC) BUN – 26 Creatinine- 2.0 Electrolytes Urinalysis Chest Xray (CXR) – Bilateral lower lobe infiltrates Nursing Assessment Findings Textbook (Source) According to your textbook what is the signs and symptoms of the medical diagnosis and nursing diagnosis Pressure or aching in chest Constrictive, squeezing, heavy choking or suffocating sensation Location sub sternal with radiating into neck, jaw and down arms. Pain lasts for only a few minutes (5 to 15 min) Pain occurs during activity or has a precipitating factor Pain at rest is unusual Diaphoresis Shortness of breath Lewis, (p.772) 1|Page Patient Specific C/O of sharp pain Denies any squeezing or suffocating sensation Location right upper chest with no radiation, no redness, bruising or injury noted in right upper chest. No masses or tenderness noted upon palpation. Pain last several hours, denies and nausea or vomiting Pain occurs after eating Pain during activity and rest, no restriction in activity or ADLS Skin warm and dry, color pink Denies any shortness of breath, lungs clear to auscultation bilaterally. Respiration regular and unlabored at 18 What is the assessment data, signs and symptoms that your patient exhibits. This is objective and subjective data. It also can be retrieved from the MD’s admission notes, History and Physical, Emergency Room record; admission nurses notes, patient, family and your assessment. Student Name: Nurse Nancy SVN Patient Initials: JDS Age: 86 Clinical Prep Sheet Unit: 3-East Date: 01/01/2012 Clinical Wk#_1 Allergies: NKDA_________________________________ Nursing Diagnosis: Problem r/t etiology Refers to specific patient problem and need. NOT A MEDICAL DIAGNOSIS Short Term Goal Met, Partial Met, Not Met and Analysis Patient oriented, Realistic, Timed, and Measurable Patient will have improved skin integrity BEOS (by end of stay) AEB decreased redness and improved healing of stage 4 ulcer. Goal met patient wound healing without difficulty. If goal partial met or not met put why it was not met and what you plan to do. Example goal not met wound healing not improving, review and revise plan of care with patient and team members. Assessment Interventions What you would assess and monitor with rationale: Asses extremities’ for normal range of motion (limited movement can cause contractures) Assess VS and LOC (changes in memory, orientation, etc could indicate neurological deficits: and change in VS could indicate infection, resp./cardiac distress) Nursing Interventions: (Specific to Patient) Intervention with rationale 1. Linen wrinkle –free/dry (moisture and wrinkles increase breakdown of the skin) Evaluation of Interventions (Patient’s Response) Evaluations are patient oriented, not nurse oriented. There should be a patient response to the intervention performed. Skin remained free from further breakdown 2. Avoid friction when moving patient (to prevent skin breakdown) Used draw sheet-not friction or shearing of skin 3. Reposition every 1-2 hours; get patient out of bed. (prolonged pressure on bony prominences decreases circulation and increases skin breakdown) Turned and reposition q2, no increased reddened areas. 4. Encourage ADLs ( to increase perfusion and circulation) Patient assisted with ADLs 5. ROM (passive and active) (increases circulation to prevent DVTS; maintains joint mobility and decreases development of contractures) FROM in bilateral arms decreased range of motion in both legs. Patient Education and Health Maintenance: Teaching 1. Referral Instruct active ROM exercises (see NI 5 above) 1. Evaluation: Patient demonstrated active ROM exercises Physical Therapy (assists with physical needs, RIM, ambulating, equipment) 2. Home Health (assists with needs at home, bathing, medications, dressing change) Interventions should be problem specific and performed interventions are to be highlighted and an evaluation done. 2|Page Student Name: Nurse Nancy SVN Patient Initials: JDS Age: 86 Clinical Prep Sheet Unit: 3-East Date: 01/01/2012 Clinical Wk#_1 Allergies: NKDA_________________________________ Therapeutic Communication (Must submit at least one (1) conversation per week – two exchanges) Non Verbal Behavior Verbal Behavior Nurse – Pulled up chair along side of bed and leaned forward. “You seem upset about something.” Patient – Makes contact with nurse. Shakes head yes. “I am” Nurse – Facing the patient. “Tell me more about your feelings.” Patient – Dries tears, looks angry. “I’m scared and angry.” Communication Technique Interpretation Evaluation Making Observation Therapeutic I think the client appears upset. I thought I could get the client to talk. Ineffective – There were no feelings of anger expressed. I could have said, “You seem angry.” Open ended question Therapeutic I think the client is angry. I thought I had made her angry. Effective – The client voices that she is scared and angry. Must submit one (1) communication interview per week. If you need more room you can continue on another CPS sheet. Reflection of Clinical Week (What did you expect, what really happened? How do you think you are progressing? ) Reflect over your clinical week. Put you thoughts, experiences, and feelings. If you found a specific strength or weakness you discovered about yourself you document here. State one thing you would have changed or done differently. 3|Page Student Name: Nurse Nancy SVN Patient Initials: JDS Age: 86 Clinical Prep Sheet Unit: 3-East Date: 01/01/2012 Clinical Wk#_1 Allergies: NKDA_________________________________ CPS Medication Sheet Medication Generic & Trade Dosage & Route digoxin Lanoxin Classification Why is your client taking this drug? Cardiac Glycoside CHF Loop Diuretic CHF 0.125 mg 1xday PO furosemide Lasix 40mg 1xday captopril PO Capoten ACE Inhibitor Hypertension 12.5mg every 8 hours PO potassium Cl K-Dur Electrolytes 10 mEq 2xday PO ibuprofen Motrin NSAID Electrolyte Replacement Muscle Pains 600mg every 6 hours PO v:\\vn level i\clinical\clinical prep sheet example 4|Page Nursing Implications Adverse Effects Most Serious implications and what information you need as a nurse to perform or assess before giving medication. Minimum of 3 implications. Minimum of 3 adverse effects. 1. Do not give if apical pulse less than 60. 2. Monitor digoxin level; electrolytes. 3. Monitor for violent vomiting. 1. I&O every shift, daily weight. 2. Monitor B/P, S/S overload/deficit. 3. Monitor potassium level. 1. Nausea/Vomiting 2. Yellow Hazes 3. Dysrhythmias 1. Monitor B/P-do not give if less than 90/60. 2. Monitor for orthostatic hypotension. 3. Teach to take when BP is within a normal range. 1. Dry cough 1. Monitor K level (>5.8). 2. Monitor high potassium foods. 3. Store at room temperature. 1. Muscle cramps 1. Take with food to minimize GI distress. 2. Take around the clock (ATC). 3. Advise to use sunscreen to prevent photosensitivity. 1. GI Bleed 1. Hypokalemia 2. Muscle cramps 3. Decreased BP 2. Angioedema 3. Bronchospasm 2. Bradycardia 3. Confusion 2.Hepatitis 3. Increased bleeding time 11/2012