Cases
advertisement

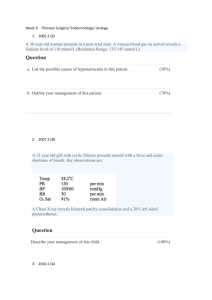
Cases For each of the following cases, suggest a plan for evaluation and treatment: A 69 year old man with a history of a perirectal abscess seven years ago now presents with mild perirectal pain and purulent discharge. Examination reveals an external opening in the right posterior perianal region. A 43 year old man presents with severe right-sided peri-rectal pain. He is pyrexial and unable to sit comfortably. There is a tender fluctuant mass in the right peri-rectal area with overlying erythema A 30 year old female presents with a two month history of pain and bleeding on defaecation. She has a 5 year history of constipation. She refuses to allow you perform a per rectum examination as she believes it would be too painful. A 68 year female with a long history of constipation presents with a three year history of protrusion of the rectum during bowel movements. Initially, the protrusion spontaneously reduced but on several recent occasions required manual reduction. Examination is unremarkable except for a somewhat lax internal sphincter. A 58 year old female is admitted with RUQ pain. Her temperature is 39°C with otherwise stable vitals. WCC is 12.3, bilirubin is 4, alkaline phosphatase is 1.5 times normal and an ultrasound shows gallstones and a dilated common duct measuring 1.3cm A 70 year old male diabetic (Type 1) presents with nausea, vomiting, RUQ pain and fever. PFA shows air in the wall of the gallbladder A 44 year old healthy female is noted to have gallstones by ultrasound for a suspected ovarian cyst. She has no symptoms of biliary tract disease. A 68 year old male presents with a five year history of intermittent crampy abdominal pain presents with a 48 hour history of left iliac fossa pain and a fever. He describes good health until the pain began 5 days ago. His only past medical history is hypertension for which is takes amlodipine 5mg od. He stopped smoking aged 40 and drinks occasionally. Physical exam reveals a slightly overweight male in moderate distress. His temperature s 38°C BP is 140/88, HR 100bpm. He is locally tender in the left iliac fossa but has no peritoneal signs. PR exam unremarkable, FOB-. Hb13.8, WCC 16.3, normal U&E. What is your differential diagnosis? What is your initial management? Do you plan any further studies at this time? If he had a palpable mass in the LIF how would your management change? A 64 yr old male presents with a complaint of passing air in the urine A 65 yr old male receives a barium enema examination for suspected diverticular disease. The radiologist is unable to determine whether it is diverticular disease with inflammatory scarring or carcinoma. How do you proceed? A 69 yr old female presents with peritoneal signs in her LID. Subsequent laparotomy reveal a free perforation of a sigmoid diverticulum. How do you proceed? A 55year old man with a seven year history of diverticular disease presents with left iliac fossa pain. His last bowel movement was 4 days prior to admission but he reports passing flatus. A 45 yr old male complains of heartburn partially relieved by lansoprazole and has been present for 4 years. He also has intermittent attacks of dysphagia and on occasions has regurgitated his food. A 63 yr old male presents with a two month history of increased difficulty swallowing. He has lost approximately 3 kg in weight over the last month. His past medical history is notable for a myocardial infarction two years ago. A 56 year old female has a two year history of chest pain. It has no clear relationship with exercise. She complains of intermittent trouble eating solid foods with occasional regurgitation of liquids. A 56 year old male with a longstanding history of GORD symptoms presents with dysphagia. Endoscopy reveals a stricture of the oesophagus 39cm from the incisors. A 74 year old white male presents with a history of choking sensation during eating. He notes frequent regurgitation of undigested food 12 to 36 hours after meals. He has a cough when lies down and has three episodes of aspiration pneumonia. A 32 year old female complains of severe substernal chest pain one hour after undergoing endoscopy. On exam he has crepitus/ A chest X-ray shows air in the mediastinum. A 55 yr old male presents with mild epigastric pain and an episode of blood-tinged vomitus. His past medical history reveals a previous MI 6 months ago for which he had a PCI. He is unsure of his current medications but reassures you he takes them every day. His BP in 110/70 and HR is 100 bpm. He has no significant findings on physical examination. His stool is FOB+. A 64 year old male presents with a week long history of loose stool and one episode of a large amount of bright red bleeding per rectum. BP is 105/60 and pulse is 104 pm. He has no significant findings on physical exam. He has frank red blood on rectal examination. A 54yr old alcoholic presents with haematemeis. He noted this began after violent retching A 34 yr old female presents with bloody diarrhoea. She has a recent history of 8 to 10 bowel movements containing blood and mucus associated with tenesmus. A 49 yr old South East Asian woman presents with vague abdominal pain and recent weight loss. She reports no significant past medical history. Her liver function tests are normal. A RUQ ultrasound reveals a 4cm mass in the right lobe of the liver A 64yr old male with multiple previous episodes of acute pancreatitis presents with massive haematemeis. His liver function test s normal. He has no signs of chronic liver disease. After stabilisation an upper GI scope reveals isolated gastric varices. What is the likely aetiology and treatment? A 61 yr old male has been hospitalised for 8 days after his fourth upper GI bleed secondary to oesophageal varices and alcoholic cirrhosis. Over the last 48 hours he has become increasingly lethargic and has asterixis on exam. His INR is 2.5, albumin 25 g/dl. What is the likely diagnosis and what do you recommend? A 31 yr old previously well female present with sudden onset acute RUQ pain and dizziness. She is hypotensive, tachycardic and tender in the RUQ. Her Hb is 9.4g/dl. Her only medical history is OCP use. A 52 year old male returns to hospital three weeks after an episode of acute pancreatitis with persistent abdominal pain and a serum amylase of 1700 A 49 yr old female s admitted with acute pancreatitis. Ultrasound reveals gallstones and dilated common ducts. Her amylase returns to normal and her pain settles. A 52 yr old man presents with painless jaundice weight loss of about a stone. Abdominal Ct reveals a 3cm mass in the head of the pancreas. A 39 year old male presents with several small pigmented lesions surrounding a previous melanoma excision site two years ago. He has axillary lymphadenopathy. A 69 yr old male presents with a one cm ulcerated lesion on the tip of his nose A 59 yr old farmer presents with a one cm ulcerating lesion on the right lateral aspect of his lower lip. A 49 year old male presents with a 5cm mass in the soft tissue of his right thigh. Biopsy reveals a fibrosarcoma. CXR reveals no evidence of metastatic disease. A 42 year old male has a 1.5 cm duodenal ulcer at endoscopy for epigastric pain. A 57 yr old male underwent endoscopy for abdominal pain and early satiety. There is a 2cm gastric ulcer. A 35 yr old man presents with recurrent gastric ulceration despite multiple courses of triple therapy and maintenance PPIs. A 25 year old male receives a “fight bite” over the dorsum of his 4th MCPJ. A 58yr old cachectic patient with oesophageal adenocarcinoma is to undergo neo-adjuvant chemoradiotherapy prior to surgery . He has dysphagia to most solids– how can you provide nutritional support? A 22 yr old man undergoes exploratory laparotomy after a stab wound to the abdomen. A small bowel laceration is repaired primarily. What is the ideal nutritional support for this patient?