ANCA-associated small vessel vasculitides cause rapidly
advertisement
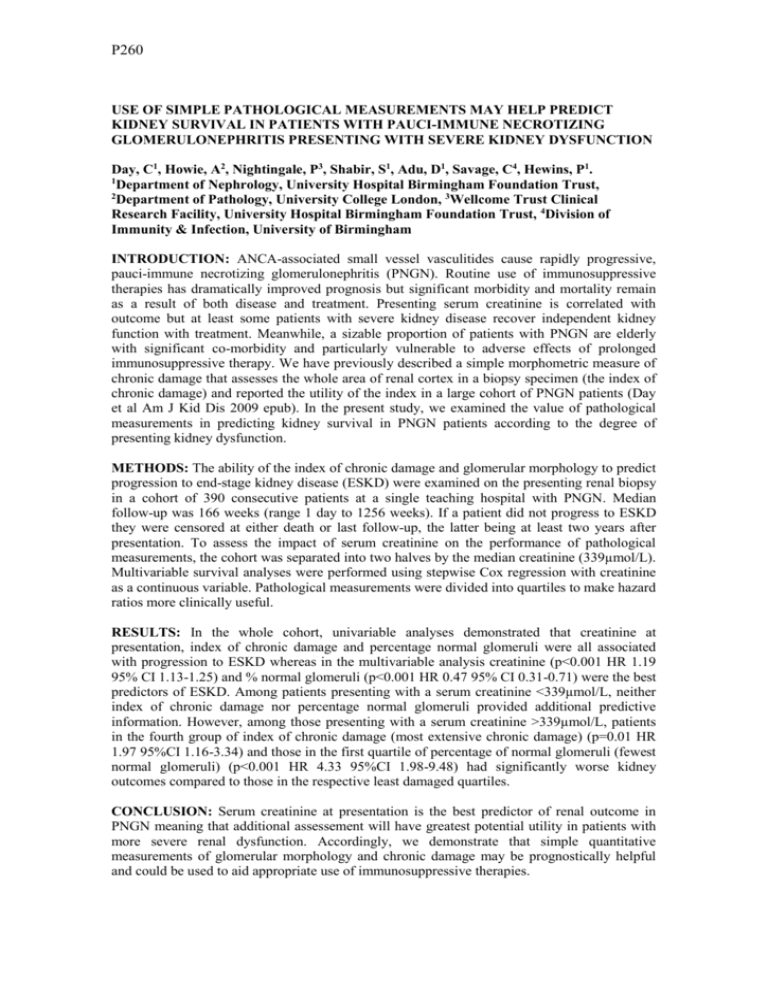
P260 USE OF SIMPLE PATHOLOGICAL MEASUREMENTS MAY HELP PREDICT KIDNEY SURVIVAL IN PATIENTS WITH PAUCI-IMMUNE NECROTIZING GLOMERULONEPHRITIS PRESENTING WITH SEVERE KIDNEY DYSFUNCTION Day, C1, Howie, A2, Nightingale, P3, Shabir, S1, Adu, D1, Savage, C4, Hewins, P1. 1 Department of Nephrology, University Hospital Birmingham Foundation Trust, 2 Department of Pathology, University College London, 3Wellcome Trust Clinical Research Facility, University Hospital Birmingham Foundation Trust, 4Division of Immunity & Infection, University of Birmingham INTRODUCTION: ANCA-associated small vessel vasculitides cause rapidly progressive, pauci-immune necrotizing glomerulonephritis (PNGN). Routine use of immunosuppressive therapies has dramatically improved prognosis but significant morbidity and mortality remain as a result of both disease and treatment. Presenting serum creatinine is correlated with outcome but at least some patients with severe kidney disease recover independent kidney function with treatment. Meanwhile, a sizable proportion of patients with PNGN are elderly with significant co-morbidity and particularly vulnerable to adverse effects of prolonged immunosuppressive therapy. We have previously described a simple morphometric measure of chronic damage that assesses the whole area of renal cortex in a biopsy specimen (the index of chronic damage) and reported the utility of the index in a large cohort of PNGN patients (Day et al Am J Kid Dis 2009 epub). In the present study, we examined the value of pathological measurements in predicting kidney survival in PNGN patients according to the degree of presenting kidney dysfunction. METHODS: The ability of the index of chronic damage and glomerular morphology to predict progression to end-stage kidney disease (ESKD) were examined on the presenting renal biopsy in a cohort of 390 consecutive patients at a single teaching hospital with PNGN. Median follow-up was 166 weeks (range 1 day to 1256 weeks). If a patient did not progress to ESKD they were censored at either death or last follow-up, the latter being at least two years after presentation. To assess the impact of serum creatinine on the performance of pathological measurements, the cohort was separated into two halves by the median creatinine (339µmol/L). Multivariable survival analyses were performed using stepwise Cox regression with creatinine as a continuous variable. Pathological measurements were divided into quartiles to make hazard ratios more clinically useful. RESULTS: In the whole cohort, univariable analyses demonstrated that creatinine at presentation, index of chronic damage and percentage normal glomeruli were all associated with progression to ESKD whereas in the multivariable analysis creatinine (p<0.001 HR 1.19 95% CI 1.13-1.25) and % normal glomeruli (p<0.001 HR 0.47 95% CI 0.31-0.71) were the best predictors of ESKD. Among patients presenting with a serum creatinine <339µmol/L, neither index of chronic damage nor percentage normal glomeruli provided additional predictive information. However, among those presenting with a serum creatinine >339µmol/L, patients in the fourth group of index of chronic damage (most extensive chronic damage) (p=0.01 HR 1.97 95%CI 1.16-3.34) and those in the first quartile of percentage of normal glomeruli (fewest normal glomeruli) (p<0.001 HR 4.33 95%CI 1.98-9.48) had significantly worse kidney outcomes compared to those in the respective least damaged quartiles. CONCLUSION: Serum creatinine at presentation is the best predictor of renal outcome in PNGN meaning that additional assessement will have greatest potential utility in patients with more severe renal dysfunction. Accordingly, we demonstrate that simple quantitative measurements of glomerular morphology and chronic damage may be prognostically helpful and could be used to aid appropriate use of immunosuppressive therapies.